Effects and Benefits of a Program to Promote Tooth Brushing Among 12-Year-Old School Children in the Dominican Republic
Yvonne A.B. Buunk-Werkhoven1,2* and Selma Y. Burrekers2
1International Oral Health Psychology, The Netherlands
2Foundation Bocas Sanas Holanda-Maimon, The Netherlands
Submission: April 10, 2019; Published: April 26, 2019
*Corresponding author: Dr. Yvonne A.B. Buunk-Werkhoven, Rozenstraat 74a| 1016 NX Amsterdam, The Netherlands
How to cite this article: Yvonne A.B. Buunk-Werkhoven, Selma Y. Burrekers. Effects and Benefits of a Program to Promote Tooth Brushing Among 12-Year-Old School Children in the Dominican Republic. Adv Dent & Oral Health. 2019; 10(5): 555799. DOI: 10.19080/ADOH.2019.10.555799
Abstract
Objective:
a. to examine whether the DMFT level has decreased among 12-year-old children in the Dominican Republic, and
b. to evaluate the impact of the School-based Oral Health Education and Hygiene program (based on ‘Fit for School’ approach) of the Foundation Bocas Sanas Holanda-Maimón (BSHM).
Methods: The DMFT and PUFA levels of 136 primary school children (intervention group N=65 and control group N=71) were measured around Puerto Plata by two dental hygienists. Moreover, 34 teachers and volunteers, who are involved in tooth brushing behavior program of the children at six ‘BSHM-schools’, completed voluntarily an evaluation questionnaire.
Results: Findings show that in seven years the DMFT-level at ‘BSHM-schools’ has significantly decreased from DMFT=3.9 to DMFT=3.6, p=0.025. The DMFT- and PUFA-levels were significantly different between both groups, i.e., less caries, fillings, pulpal involvement, and fistulas. More caries was seen at schools that were visited by tourists. The evaluation by teachers showed a moderate understanding, remembering, implementation of this BSHM-program, and the availability of enough fluoride toothpaste and water were the determining factors too.
Conclusion: A decreased DMFT level was found in 12-year-old children at the ‘BSHM-schools’. This BSHM program should be more focused on schools in regions with a negative impact of tourism on caries prevalence. It is important to create an optimal working alliance among teachers and BSHM-volunteers in the school-based oral health interventions. Insights into the benefits of this program and refinements of optimally targeted intervention, including longitudinal studies are needed to improve the results.
Keywords: School-based oral health education and hygiene program; Oral health promotion; Tooth brushing; Bocas Sanas Holanda-Maimón; Dominican Republic
Introduction
Caries, perhaps more than periodontitis, is a substantial public (oral) health problem in most industrialized, but also in developmental countries, and poor oral health has a negative effect on general health and quality of life [1]. However, to define poor oral health, it is necessary to know what constitutes optimal oral health. In 2016, the World Dental Federation (FDI) launched a new definition for oral health, which captures the full scope of oral health [2]: “Optimal oral health can be considered as a fundamental component of general health, including physical and mental well-being. Oral health is influenced by attitudes, experiences, perceptions, expectations and the ability to adapt to circumstances, of both individuals and communities. Oral health reflects the physiological, social and psychological attributes that are essential for the quality of life”. One of the important things captured in this definition is the ability of oral health to reflect on the quality of life. For instance, if a child has severe caries the quality of life is more likely to decrease pain because of caries may lead to school absence, which in turn reduces the ability to learn [3]. Globally, it is of great importance to lower the prevalence of caries in children. Like patterns in poor developmental countries, Dutch children of lower socio-economic classes (SES) have a bigger chance of developing caries [4], and for instance, a study in Iraq showed that a lower SES is associated with higher sugar consumption [5]. A trend can be seen where the assessed level of dental caries prevalence as well as dental treatment needs among populations -mostly measured with the index for decayed, missing, and filled teeth (DMFT)- in developed countries generally decreases, but increases in developing countries [6,7].
According to the World Health Organization [8] the Dominican Republic is a developing country, and the WHO recognizes that primary schools in all countries are centrally accessible, not only to improve awareness of the importance of (oral) health in children, but also to pay attention to adequate tooth brushing during early childhood. The primary school period is a crucial stage of child development when health-related behaviors that are practiced routinely are more likely to be habitual. For that reason, the WHO is involved in different school health programs worldwide [9]. More than two decades ago, in 1997, one of the main goals of the WHO was to reduce the number of decayed, missing, filled permanent teeth (DMFT) of 12-year-old children to a DMFT level of less than 3.0 in the year 2000 [6].
In 2003, the World Oral Health Report showed there was a moderate DMFT level in the Dominican Republic of 2.7 to 4.4, and therefore, an oral hygiene behavioral change intervention was, and is still needed in the Dominican Republic to lower the DMFT level. For many years, the Oral Health Program (ORH) of the WHO emphasizes the application of evidence-based strategies in oral health promotion and prevention as well as in the treatment of oral diseases worldwide [10]. Especially, because the success of health education initiatives and programs lies in the ability to understand the differences in psychosocial factors associated with oral hygiene behaviors (knowledge, attitudes, beliefs, environment, skill, behavior etcetera) at the individual and community level [11,12]. Knowing that oral hygiene interventions need to be embedded within oral health systems that are financially fair for disadvantaged and poor population groups [13], and to improve oral health of children in the Dominican Republic, in 2008 the Foundation Bocas Sanas Holanda-Maimón (BSHM) started a prevention program, i.e., more than a decade ago and mainly in the district of Maimón (rural environment) around the province of Puerto Plata. This BSHM program to promote oral health awareness and prevent oral diseases in Dominican Republic children- included oral health education and instruction (i.e., ‘tooth brushing behavior’, ‘hygiene’, and ‘food’), clinical intraoral examination, dental and periodontal screening, preventive and curative treatment. In similar vein and from an evaluation study in the Philippines, it was proven that such an integrated program, in which fluoride applications are included, or sealants in combination with other interventions, was effective in preventing caries [14].
At the start July 2008- of the Foundation Bocas Sanas Holanda- Maimón initiative, the DMFT level in the region of Maimón in the Dominican Republic was 3.9 [15]. In February 2010, findings of a field study on the determinants of oral hygiene behavior within the BSHM in the same region showed that social norms and attitude emerged as significant predictors of the intention to perform adequate oral hygiene behavior (OHB) within the next year. In addition, the perceived task complexity of OHB self-care practices and the feelings of control over OHB seemed to be important [16]. In a couple of years, in which the BSHM program and the professional oral health care were provided, socalled water bins to stimulate tooth brushing and hand washing were placed at selected schools. This combined approach was based on the ‘Fit for School’ approach. ‘Fit for School’ is a Filipino organization that focusses on the education sector and commits to improving the health of schoolchildren [17]. Nowadays, around Puerto Plata, nine schools are provided with a tooth brushing and hand washing bin [18].
The present evaluation study aimed to examine whether the DMFT and PUFA level has decreased among 12-year-old children in the region of Maimón in the Dominican Republic. In addition, this study aimed to evaluate the impact of the School-based Oral Health Education and Hygiene program of the Foundation Bocas Sanas Holanda-Maimón.
Methods
Research design and ethics statement
This quasi-experimental field study was conducted in accordance with the Declaration of Helsinki, and authorization for participation in this evaluation study was obtained from the Foundation Bocas Sanas Holanda-Maimón (Rhenen, the Netherlands). Involvement of the primary schools was confirmed, participation of the schoolboys and girls was on a voluntary basis, they were informed about what participation entailed and were free to refuse contribution. Therefore, an extensive formal written informed consent of the parents/caregivers and of the schoolchildren was waived, and only verbal informed consent was obtained. Confidentiality was assured; no pressure was placed on all participants to take part in the screening by Dutch qualified dental hygienists, who conducted the screening using a natural routine method based on their own professional daily practice experience, without mutual calibration. The ethical board, the Central Committee on Research Involving Human Subjects, affirms that research that requires completing a questionnaire for one occasion does not fall under the scope of the Medical Research Involving Human Subjects Act [19].
Participants and procedure
Based on a previous cross-sectional study [15], at the end of February/beginning of March 2015, the DMFT and PUFA levels of 136 12-year-old primary school children were measured around Puerto Plata, Dominican Republic by two volunteers of BSHM, who are Dutch dental hygienists with significant experience in qualifying these scores. Children who turned into 13 years, three months before, or those who turned into 12 years, within 3 months from, the date that they were examined, were included in the study. In total, 65 children who participated for at least three years in the prevention program of BSHM, and those who had their ‘card with oral health data’ available, were clinically examined (i.e., intervention group out of 4 BSHM-schools; ‘Juana Hutardo’ (visited by tourists), ‘Los Canos’, ‘Maggiolo’ and ‘Los Pasos de Sabiduria’). 71 primary school children who were not involved in the BSHM-project were clinically examined too (control group out of 3 schools; ‘Los Rieles’, ‘San Marcos Abajo’ (both visited by tourists) and ‘Salome Ureña’). It was assumed that children from these three schools -the control group- brush their teeth to normally Dominican habits. Observations whether schools were visited by tourists, as well as if the children bought candies at their school were included in the evaluation too.
Measures
Individual’s clinical oral health status was measured by using the DMFT and PUPA. Due to a limited and potentially misleading impression of the DMFT, and to include information about the level of caries-disease, and to meet with the ethical obligations, also the PUFA was measured [20]. The records of the DMFT indicated as: Decayed (D), Missing due to caries (M) or Filled (F; including Sealants) per element (T=Teeth), and the records of the PUFA indicated whether or not there was an exponation of the Pulp (P), Ulceration (U), Fistula (F) or Abscess (A). No distinction was made for milk- and permanent teeth. DMFT level was measured with a sum score of D, M and F. In a similar way the PUFA level was measured with a sum score of P, U, F and A. Only the teachers and volunteers, who are involved in tooth brushing behavior program of the children at ‘BSHM-schools’ -the intervention groupcompleted voluntarily a culturally adapted questionnaire.
Questionnaire for program evaluation
The questionnaire was developed by the authors, based on their expertise as aspirant and professional oral hygienists, combined with their clinical and research experience, and was completed with items used in previous unpublished evaluation studies. In addition, the questionnaire was checked and translated into Spanish as its mother tongue by a native Spanish speaker of Dominican Republic descent. In total 47 items were filled out by 34 teachers and volunteers -not by the school children- from six BSHM-schools to evaluate the prevention program: to what extent the provided education and instructions on ‘Tooth brushing behavior’, ‘Hygiene’, and ‘Food’ were understood, remembered and/or implemented by the Dominican Republican teachers and volunteers, and to get valuable insights in the ’Experiences with BSHM’ for the Foundation to become more effective in achieving their goals.
‘Tooth brushing behavior’ was measured with 24 items; 10 items could be scored with 1=correct or 0=incorrect, and a sum score was computed (ranging from 0 to 10); 14 items were open ended. Example items: “Do the children brush their teeth at school?” and “What is the main reason to brush the teeth at school?”
‘Hygiene’ was measured with 7 items; 3 items could be scored with 1=correct or 0=incorrect, and a sum score was computed (ranging from 0 to 3); 4 items were open ended. Example items: “Is soap available at the tooth brushing and hand washing bin?” and “How or where are the tooth brushes kept?”
‘Food’ was measured with 7 items; 4 items could be scored with 1=correct or 0=incorrect, and a sum score was computed (ranging from 0 to 4); 3 items were open ended. Example items: “Has your school been visited by tourists?” and “What kind of education or instruction about food do the children get?”
‘Experiences with BSHM’ was measured with 4 open ended items, e.g., “Do you think all primary schools in the Dominican Republic need a tooth brushing and hand washing bin?”. The variable ‘Pain’ was measured with 5 open ended items, e.g., “How many times did a child stay at home because of tooth ache or pain in the mouth?”
In total 30 items were open ended, and 17 questions were items with cut-off points. These cut-off points were set up in such a way, that an unsatisfactory grade was obtained when the amount of correct answers was smaller or equal to half of the total sum score. For instance, if three out of ten questions concerning ‘Tooth brushing behavior’ were answered correctly, the outcome of the school was: ‘tooth brushing behavior is insufficiently followed, understood, remembered and implemented’. If an open ended question was not answered this item was graded as ‘insufficient’. The ‘Tooth brushing behavior’, ‘Food’, and ‘Hygiene’ sum scores were computed by adding all the scores; a higher sum score indicates a higher level of ‘understanding, remembering and implementation of the BSHM program’.
Statistical analyses
The IBM Statistical Package for Social Sciences 16.0 (SPSS, Chicago, Illinois, USA) was used for data analysis. Frequency distributions were created from the DMFT and PUFA levels, and means, including standard deviations (SD), were calculated from all quantitative variables. The assumption of normality was evaluated using the Shapiro-Wilk test, Kolmogorov-Smirnov test and a visual inspection of the histograms. Moreover, unpaired t-tests were performed to determine significant differences in mean scores of the variables between the intervention group and control group (also for buying candies at school and tourism in relation to the DMFT level). Differences between the mean DMFT level of the control group and mean DMFT level measured in 2008 were measured by using a one-sample t-test.
Results
DMFT and PUFA levels
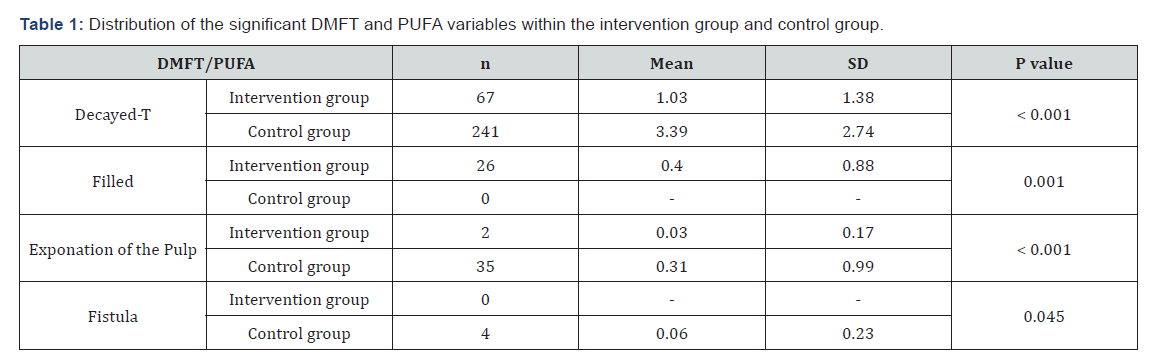
No significant differences between the intervention and control group were found for the variables Missing due to caries (M); intervention group (M=1.03, SD=0.64) versus control group (M=3.39, SD=0.59), Ulceration (U); intervention group (zero) versus control group (M=0.01, SD=0.12), Abscess (A); intervention group (zero) versus control group (M=0.01, SD=0.12), and Sealants; intervention group (M=0.06) versus control group (M=0.01) . However, the test showed a statistically significant difference between the intervention- and control group for the variables Decayed, Filled, exponation of the Pulp, and Fistula, i.e., children in the intervention group have less decayed teeth, less pulpal involvement, and less fistula, but their mean number of fillings was higher. Table 1 shows the distribution of DMFT and PUFA variables for the participants within the intervention group and control group 2015.
In seven years the DMFT-level at ‘BSHM-schools’ has significantly decreased from DMFT=3.9 in 2008 to DMFT=3.6 (p=0.025). In 2015, the mean DMFT was 2.7; intervention group (M=1.6) versus control group (M=3.6). In the intervention group 40% of the children had a DMFT=0 and 89.2% of the children had a DMFT < 3.0 versus the percentage of children in the control group 19.7% with a DMFT=0 and 52.2% with a DMFT < 3.0. The mean PUFA level was 0.32; intervention group (M=0.03) versus control group (M=0.58), (p=0.001).
More caries and more sealants were observed at schools that were visited by tourists (p=0.008 and p=0.024 respectively). The mean DMFT level at schools that were visited by tourists, was 3.1 versus the mean DMFT level of 2.1 at schools that were not visited by tourists (p=0.047). At one of the BSHM-schools, i.e., ‘Juana Hutardo’ that was visited by tourists, there were significantly more children without cavities (p < 0.001), than at the two schools that were not involved in the BSHM-project and were visited by tourists too, i.e., ‘Los Rieles’ and ‘San Marcos Abajo’.
Questionnaire for program evaluation
Teachers and volunteers of the schools ‘Juana Hutardo’(N=7), ‘Los Canos’ (N=4), ‘Maggiolo’ (N=1) and ‘Los Pasos de Sabiduria’(N=5), ‘Centro Educativo Las Avispas’ (N=7), ‘Conception Garcia’ (N=4), and ‘Unknown’ (N=5; the name of the school was missing) reported a moderate understanding, remembering, implementation of the BSHM-program (i.e., the provided education and instructions on ‘Tooth brushing behavior’, ‘Hygiene’, and ‘Food’). Almost all teachers and volunteers (N=32) reported to know that preventing caries is the main reason for brushing teeth at school. However, seven respondents reported not to brush daily at school, with main reasons: ‘there was no availability or sufficient fluoride toothpaste and water’ (N=17), ‘children had forgotten their tooth brush at home (N=5) or ‘no time’ (N=7). 30 teachers reported that the tooth brushes had to be cleaned with water; more than the half (N=19) reported to keep the tooth brushes at school, a quarter kept the tooth brush at home and three respondents kept it in their schoolbag. Only at 1 school soap was available at the tooth brushing and hand washing bin. Hand washing seemed not to be a regular activity; two-thirds reported to brush their hands after going to the toilet and others (52%) reported to wash the hands before or after tooth brushing. About the half (N=18) reported to provide education and instructions on food.
Four out of five (N=27) teachers and volunteers reported that the children bought candies or ice-creams during the school break. The same number of respondents was willing to discuss the sugar-problem with the shop owners and wanted to advise them to sell the children more sugar-free products, e.g., crackers, fruits, etcetera. Almost two-thirds (N=22) reported to prefer receiving alternatives as diverse school products from tourists who visited their schools. 20 teachers reported that children never complain about pain in the mouth. 10 respondents mentioned that sometimes children have complaints and that they inform the parents or bring the child to a dentist. At every school, a child had stayed at least once at home because of tooth ache or pain in the mouth. Moreover, not having money is the major reason for not going to the dentist (20). Almost all respondents preferred to have twice a year a control or visit by the BSHM-team to maintain the benefits of the BSHM program. The teachers and volunteers mentioned to have all primary schools in the Dominican Republic to get a tooth brushing and hand washing bin, including a follow-up of the School-based Oral Health Education and Hygiene program of the Foundation Bocas Sanas Holanda-Maimón.
Discussion
The aim of this evaluation study was to examine whether the DMFT and PUFA level has decreased among 12-year-old children in the region of Maimón, in the Dominican Republic. The additional aim of this study was - after seven years- to gain insight in the effects and benefits of the School-based Oral Health Education and Hygiene program of the Foundation Bocas Sanas Holanda- Maimón. A significantly decreased DMFT level of 3.6 was found in 12-year-old children in the Dominican Republic. However, the mean DMFT level in the intervention group was 1.6, and at schools that were not visited by tourists, the mean DMFT was 2.1; both these outcomes matched one of the main goals of the WHO, to reduce the DMFT of 12-year-old children to less than 3.0 [6].
Descriptive findings from participation in the questionnaire provided insight into the BSHM program, and demonstrated that over the years it was appreciated by the children and by the teachers and volunteers. In addition, the teachers and volunteers involved in the ‘BSHM-schools’ were more inclined to engage in the BSHM program when they had more feelings of control over this school-based oral health intervention, like they reported a moderate understanding, remembering, implementation of the BSHM-program. Therefore, it is very important to create an optimal working alliance among the teachers and BSHM-volunteers. Also it turned out that the BSHM program should be more focused on schools in regions with a negative impact of tourism on caries prevalence.
The present evaluation study has some limitations. First, the sample size used in this study was not calculated, but the sample was based on the number of children screened at the BSHMschools, which was in line with a previous cross-sectional study [15]. Second, although there was no calibration among the two dental hygienists, the use of the DMFT and PUFA as measurements to screen the oral condition is valuable and sufficient for the general status of the oral health of a target population [21]. Third, not all schools which participated in the BSHM program had completed the questionnaire; three out of nine ‘BSHM schools’ were excluded, because the participation of the children in the School-based Oral Health Education and Hygiene program was less than three years.
The findings of the present evaluation study provide not only actual insight into the oral health condition of 12-year-old children in the region of Maimón, in the Dominican Republic, it also supports the findings of previous studies that showed that prevention of caries should include oral health promotion and oral disease‐prevention interventions specifically designed for the target population [16,22]; specific groups as in this case young children in developmental countries with poorer oral health may need adjusted target interventions to prevent oral diseases [23].
To conclude, this study is in line with previous studies [24-26], and oral health-education and health-promoting interventions, such as the Kidsfabriek [27] and BSHM-program including instruction and feedback by important others as significant mediators and for instance, led by dental hygienists [20,28] would be the most effective method for executing the appropriate oral hygiene behavior in this context. Moreover, it may not only encourage an awareness and/or willingness by the teachers and volunteers to take better care of the school children’s dentition, but may also encourage children’s own oral self-care, including the awareness of parents and caregivers towards supervised brushing and re-brushing of their children’s teeth at home [16,27]. In general, the use of Intervention Mapping (IM) as a protocol for developing theory-based and evidence-based health promotion programs is a condition, more research investigating the oral health status, and the demographic and social characteristics of these 12-year-old school children with poorer oral health is warranted [29]. More insight in long term benefits of this BSHM program and refinements of optimally targeted intervention, including longitudinal studies are not only needed but especially recommended to be transferred to the national policy and to take over by the government of health in the Dominican Republic [20].
Acknowledgement
The authors would like to thank Cristina Doorman-Vasquez and all the health professionals from Bocas Sanas Holanda- Maímon as well as the children, teachers and others involved. Special thanks go to Nicolette Hooijschuur, Agatha Rijpma- Huitema, Yildou Anema, and Berdien Buurlage for their invaluable work and enthusiastic support. During the years the tooth brushes and fluoride toothpastes for the BSHM program were kindly supported by Colgate Palmolive Dominicana and various oral health sponsors in the Netherlands.
Conflict of Interest
The authors declare that they have no conflict of interest: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work; and no other relationships or activities that could appear to have influenced the submitted work.
References
- Petersen PE, Bourgeois D, Ogawa H, Estupinan-Day S, Ndiaye C (2005) The global burden of oral diseases and risks to oral health. Bull World Health Organ 83(9): 661-669.
- Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, et al. (2016) A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. J Am Dent Assoc 147(12): 915-917.
- Sheiham A (2006) Dental caries affects body weight, growth and quality of life in preschool children. Br Dent J 201(10): 625-626.
- Truin GJ, Schuller AA, Poorterman JH, MulderJ (2010) Secular trends of caries prevalence among 6 and 12 year-old youth in the Netherlands. Ned Tijdschr Tandheelkd 117(3): 143-147.v
- Ahmed NA, Astrom AN, Skaug N, Petersen PE (2007) Dental caries prevalence and risk factors among 12-year old schoolchildren from Baghdad, Iraq: a post-war survey. Int Dent J 57(1): 36-44.
- Petersen PE (2003) The World Oral Health Report 2003: continuous improvement of oral health in the 21st century - the approach of the WHO Global Oral Health Program. Community Dent Oral Epidemiol 31(suppl 1): 3-23.
- Petersen PE (2008) World Health Organization global policy for improvement of oral health - World Health Assembly 2007. Int Dent J 58(3): 115-121.
- World Health Organization. Dominican Republic [7 paragraphs].
- Petersen PE (2010) Improvement of global oral health - the leadership role of the World Health Organization. Community Dent Health 27(4): 194-199.
- World Health Organization. The objectives of the WHO Global Oral Health Program (ORH).
- Adair P, Ashcroft A (2007) Theory-based approaches to the planning and evaluation of oral health education programs. In: Pine C and Harris R, (Eds.), Community Oral Health. 2nd edn. United Kingdom: Quintessence 307-331p.
- Buunk-Werkhoven YAB, Dijkstra A, van der Schans CP (2011) Determinants of oral hygiene behavior: A study based on the theory of planned behavior. Community Dent Oral Epidemiol 39(3): 250-259.
- Petersen PE (2009) Global Policy for Improvement of Oral Health in the 21st Century-Implications to Oral Health Research of World Health Assembly 2007, World Health Organization. Community Dent Oral Epidemiol 37(1): 1-8.
- Monse B, Naliponguit E, Belizario V, Benzian H, van Palenstein Helderman W (2010) Essential health care package for children--the ‘Fit for School’ program in the Philippines. Int Dent J 60(2): 85-93.
- Everaars B (2009) The Prevalence of Dental Caries in 12-Year-Old Dominican Children, Bachelor Thesis. Utrecht: University of Applied Sciences.
- Everaars B (2009) The Prevalence of Dental Caries in 12-Year-Old Dominican Children, Bachelor Thesis. Utrecht: University of Applied Sciences.
- Monse B, Benzian H, Naliponguit E, Belizario V, Schratz A, et al. (2013) The Fit for School Health Outcome Study-a longitudinal survey to assess health impacts of an integrated school health program in the Philippines. BMC Public Health 13: 256.
- (2018) Foundation Bocas Sanas Holanda-Maimón (BSHM).
- (2018) Central Committee on Research Involving Human Subjects (CCMO). Questionnaire research.
- Katsman E (2007) Report on the activities carried out by ‘Sonrisas’ to promote oral health: the experience of a Canadian dental hygienist in the Dominican Republic. Int J Dent Hygiene 5(3): 139-144.
- Benzian H, Garg R, Monse B, Stauf N, Varenne B (2017) Promoting Oral Health through Programs in Middle Childhood and Adolescence. In: Bundy DAP, Silva Nd, Horton S, Jamison DT, Patton GC, (Eds.), Child and Adolescent Health and Development. (3rd edn), Washington (DC): The International Bank for Reconstruction and Development / The World Bank, USA.
- Brein DJ, Fleenor TJ, Kim SW, Krupat E (2016) Using the Theory of Planned Behavior to Identify Predictors of Oral Hygiene: A Collection of Unique Behaviors. J Periodontol 87(3): 312-319.
- Werner H, Hakeberg M, Dahlström L, Eriksson M, Sjögren P, et al. (2016) Psychological Interventions for Poor Oral Health: A Systematic Review. J Dent Res 95(5): 506-514.
- Blake H, Dawett B, Leighton P, Rose-Brady L, Deery C (2015) Schoolbased educational intervention to improve children’s oral healthrelated knowledge. Health Promot Pract 16(4): 571-582.
- Ghaffari M, Rakhshanderou S, Ramezankhani A, Buunk-Werkhoven Y, Noroozi M, et al. (2017) Are educating and promoting interventions effective in oral health?: A systematic review. J Dent Hygiene 16(1): 48- 58.
- Ghaffari M, Rakhshanderou S, Ramezankhani A, Noroozi M, Armoon B (2017) Oral health education and promotion programs: Meta-analysis of 17-year intervention. Int J Dent Hygiene 16(1): 59-67.
- Buunk-Werkhoven YAB, Takrovskaja K, Steverink-Jorna LM (2018) Kidsfabriek: Oral health awareness and promotion of oral self-care during a learning and play event for children and parents in The Netherlands. Annual Clin J Dent Health 7: 22-25.
- Buunk-Werkhoven YAB, Hollaar VRY, Jongbloed-Zoet C (2014) Work engagement among Dutch dental hygienists. J Publ Health Dent 74(3): 227-233.
- Kok G, Gottlieb NH, Peters GJ, Mullen PD, Parcel GS, et al. (2016) A taxonomy of behaviour change methods; an intervention mapping approach. Health Psychol Rev 10(3): 297-312.






























