Retention of Removable Partial Denture Fabricated by Digital Designing and 3D Printing Technology - A Cross Over Study
Waleed Hamed Maryod1* and Eatemad Rekaby Taha2
1Department of Removable Prosthodontics, University of Modern Science and Arts, Egypt
2Department of Removable Prosthodontics, Ahram Canadian University, Egypt
Submission: December 10, 2018; Published: February 26, 2019
*Corresponding author: Waleed Hamed Maryod, Department of Removable Prosthodontic, Faculty of Dentistry, Modern Science and Arts University (MSA), Cairo, Egypt
How to cite this article: Waleed Hamed Maryod, Eatemad Rekaby Taha. Retention of Removable Partial Denture Fabricated by Digital Designing and 3D Printing Technology - A Cross Over Study. Adv Dent & Oral Health. 2019; 10(3): 555789. DOI: 10.19080/ADOH.2019.10.555789
Abstract
Purpose: The goal of this clinical study is to evaluate retention of digital removable partial dentures as few clinical data is available regarding this new approach. The clinical trial compared retention of digital RPD fabricated with digital impression, digital designing and casting a 3D printed pattern with conventional RPD.
Materials and Methods: Twenty partially edentulous participants were enrolled in this study. Each patient received conventional RPD (group I) constructed for the lower arch. Its retention was evaluated during three months of follow up using digital force gauge device. Then, they were recalled, and a digital impression was taken. A three dimensional image was formed and converted into 3D computer file that could be read by the computer-aided design (CAD) software. The RPD framework was digitally designed and a 3D printed resin patterns was produced, which were then cast into a metal framework by conventional method. The digitally fabricated dentures (group II) were assessed for denture retention at delivery and after one and three months later. All data were tabulated and statistically analyzed.
Materials and Methods: Twenty partially edentulous participants were enrolled in this study. Each patient received conventional RPD (group I) constructed for the lower arch. Its retention was evaluated during three months of follow up using digital force gauge device. Then, they were recalled, and a digital impression was taken. A three dimensional image was formed and converted into 3D computer file that could be read by the computer-aided design (CAD) software. The RPD framework was digitally designed and a 3D printed resin patterns was produced, which were then cast into a metal framework by conventional method. The digitally fabricated dentures (group II) were assessed for denture retention at delivery and after one and three months later. All data were tabulated and statistically analyzed.
Conclusion: Retention of digital RPD fabricated with digital impression, digital designing and casting a 3D printed pattern was higher than conventional RPD.
Keywords: Partial denture; Retention; Digital impressions; Digitally designed framework; 3D printing
Abbrevations: CAD: Computer Aided Design; CAM: Computer Aided Manufacturing; CNC: Computer Numerical Control; 3D: 3 Dimensional; RP: Rapid Prototyping; SLM: Selective Laser Melting; SLS: Selective Laser Sintering; FDM: Fused Deposition Molding; SLA: Stereolithography; DLP: Digital Light Processing;
Introduction
Removable partial dentures are a conservative and economical treatment option to replace missing teeth in partially edentulous patients, improving their quality of life. However, its conventional fabrication is a complex and time-consuming process. To satisfy the patients aesthetically and functionally, new materials and new techniques of dentures manufacturing are developed [1-5].
Digital impressions for single crowns and fixed partial dentures have reported a high rate of success. This encourages some manufacturers to put great effort into the development of an intra-oral scanner to record hard and soft tissue morphology for the fabrication of a removable partial denture [6].
By using computer-aided design/computer-aided manufacturing (CAD/CAM) technology, removable partial dentures could be designed and produced [7,8]. CAD software allows for precise planning of the denture frame components in relation to individual teeth anatomy and the soft tissue of the oral cavity. In addition, it allows continuous control of sections of individual elements of the prosthesis, and hence the control of the planned mechanical parameters, and designing of minimally visible components [9,10].
The evolution of the CAD/ CAM technology decreases the duration of prosthesis manipulation and provide superior functional and esthetic outcomes. Also changes of the prosthesis volume and/ or shape is reduced or eliminated in this approach compared to the conventional procedures. Thus, the produced prosthesis adheres tightly to the tissue and uniformly transferring loads on it [6]. Furthermore, it permits easy duplication of the denture and manufacture of new one using stored digital data [9].
Digital designing of RPD framework is more complicated and takes much time than fixed prosthesis due to the variety of RPD parts and their irregular forms. Therefore, many researchers had investigated the proper CAD/CAM software for 3D designing of RPD framework [9-13].
The main benefits of introducing CAD/CAM in the fabrication of RPD framework involve automatic determination of a proposed path of insertion, the immediate elimination of undesirable undercuts, and the equally rapid identification of desirable undercuts. Not only is it a time saver, but also the CAD/CAM technology delivers inherent repeatability, which may assist in decreasing human errors and enhance quality control in the dental laboratory [11].
The CAD/CAM production of RPD framework based on two different processes: subtractive techniques (milling) or additive techniques. Subtractive manufacturing depends on milling the product from a block by computer numerical control machine (CNC). The subtractive procedures are greatly adapted to the fixed prosthesis. On the other hand, due to increased manufacturing time, complexity of the framework, material cost and wear, their implementation is more difficult to produce RPD framework [14].
Rapid prototyping, also known as layered manufacturing, is the collective term for various processing technologies that fabricate precise 3 dimensional (3D) models directly from computerized three-dimensional (3D) data in a short time using layer by layer building technique. CAD/CAM and RP have been successfully introduced over several years in the fabrication of inlays, on lays, crowns, fixed partial dentures. Lately, it has become commonly used for the fabrication of RPD frameworks as well as fixed restorations [15-18].
Basically, the manufacturing of RPD framework using CAD/ CAM and RP, starts with preparing dental casts using conventional or digital impressions. The casts obtained from conventional impression are scanned using digital scanner. Then, Path of insertion of the RPD is determined by the software, Followed by 3D designing of the framework components. Finally, digitally designed partial denture frameworks are produced with RP [12].
Rapid prototyping technologies (RP) include stereolithography (SLA), selective laser melting (SLM), selective laser sintering (SLS), selective deposition modeling, fused deposition molding (FDM), 3D printing and direct inkjet printing [15].The first prototyping technique introduced commercially and used in the fabrication of RPD frameworks was the Stereolithography. SLA was used to fabricate resin sacrificial patterns for RPD frameworks which were then conventionally cast into metal frameworks that showed appropriate fit. 7,9 SLA replicas are favored in specific cases requiring fine structures and internal geometry due to its high accuracy and relative low cost [19,20].
Selective laser sintering is a term used to describe the pattern fabrication from polymers or ceramics while selective laser melting refers to pattern fabrication from metal [21]. SLS and FDM have reported many disadvantages when used in making RPD pattern [22-24].
3D printing is a unique rapid prototyping technique that offers relatively low cost of machines and materials than do the other techniques and integrate with CAD software and other digital files. Currently, it is used in the fabrication of RPD frameworks by two main methods: One is to print firstly a sacrificial pattern in wax or resin materials which is then cast to metal frameworks, the other is the direct manufacture of metal frameworks by SLM technique. Direct manufacture of RPD framework is still of high production cost as well as its requirements for the property of printing machines and materials [25].
Since, the most persistent complaint about mandibular distal extension RPD’s was related to its retention [26], therefore this study was conducted to evaluate retention of RPD produced by new technologies to that of conventional RPD.
Materials and Methods
Participants enrolment
Twenty partially edentulous patients (11 women, 9 men, mean age 58.4 ± 8.3 years) were selected from the outpatient clinic of Modern Science and Arts University (MSA), Faculty of Dentistry, Egypt, to participate in this study. All patients having mandibular Kennedy class I with all posterior teeth missing. Detailed descriptions of the study were explained to each participant who signs a consent form. All participants can maintain adequate oral hygiene and clean their prostheses. They did not have major systemic health problems that may interfere with general oral health.
The ethical principles of the faculty of dentistry Research Ethics Committee, October University for Modern Sciences and Arts were followed (approval reference: E T H 1).
Prosthetic procedures
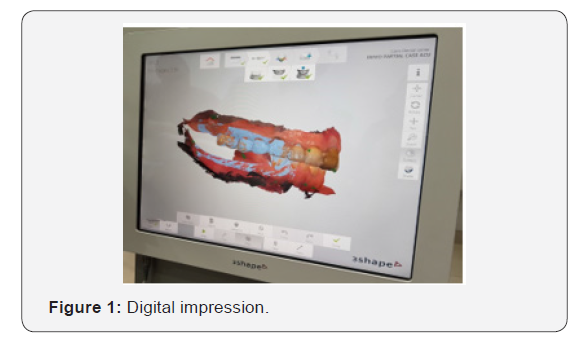
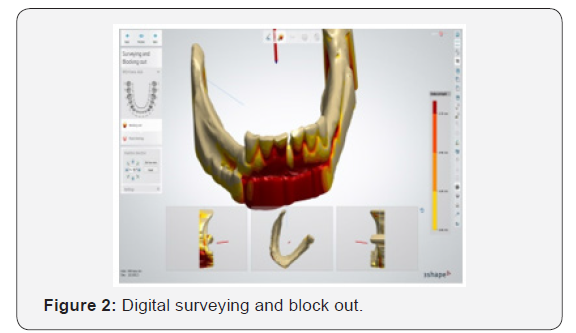
A conventional RPD were constructed for the lower arch and delivered for each patient. After 3 months of follow up and retention measurement, they were recalled and a full-arch digital impression of the mandibular arch was made with an intraoral scanner (Trios 3rd edition, 3 Shape, Copenhagen, Denmark), (Figure 1). A digital impression was made recording both the remaining teeth and the edentulous areas with special attention to capturing the soft tissues including the buccal and lingual vestibule (Figure 2). Also, a digital impression of the opposing arch and a digital buccal inter-occlusal record were made (Figure 3A & 3B).
A three-dimensional image was produced and was read by computer-aided design (CAD) software. The CAD software (3Shape Dental System, version 2.9.9.3) was then used to design the framework and generate a standard triangulation language (STL file).
The path of insertion was determined on the digital file, and the survey line was drawn with digital block-out for the undesirable undercuts (Figure 2).
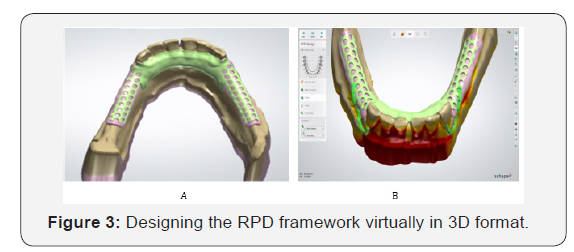
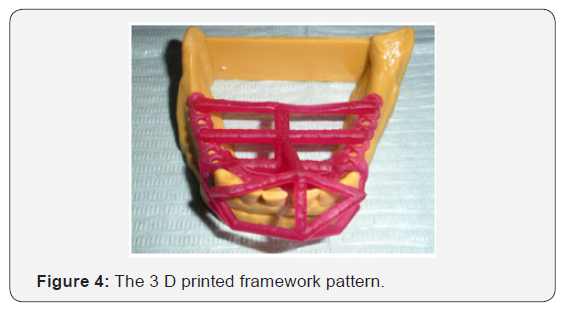
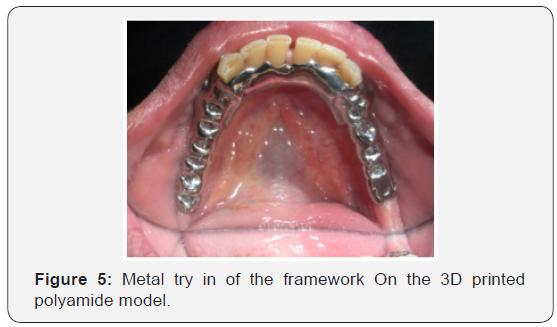
Then, the entire framework design was built virtually in 3D format and the different components of framework were added (Figure 3A & 3B). The standard triangulation language (STL) file was then transferred to a 3D printer (Rapid shape D30, Germany). This professional 3 D printer uses a digital light processing technology (DLP), a process like stereolithography (SLA). A HD resolution DLP projector, using a LED light source to photo cure liquid resin, layer by layer to build a 3d resin framework pattern of the RPD. The polyamide physical model was also obtained using the same 3D printer (Figure 4). The 3D printed materials were post cured in UV curing unit (L C 3 D print box, NEXTDENT UK) by U V light treatment. The printed resin pattern of the digital RPD is then invested and casted into cobalt- chromium framework using conventional casting technique. Metal try in of the framework was performed to check the fit and accuracy (Figure 5).
All laboratory procedures were performed by one technician at the same dental laboratory. RPD were completed in the usual manner. At the delivery visit, prosthesis adjustments were performed, and the patients were motivated to perform oral hygiene measures.
Evaluation of denture retention
Measurements were performed for each RPD at the time of denture insertion, after one month and three months later. Measurements were carried out using digital force gauge which is an advanced type of force meter device, used to measure tension or compression up to 20Kg. Lower denture retention is most accurately measured by pulling the denture in vertical direction from its geographic center.
Determination of the geographic center of the mandibular denture
This center was located on the duplicate mandibular cast by drawing four lines on the cast and extending them to the cast base in the following sequence;
a) Line (1) connecting two points at the apices of the retromolar pads of both sides of the arch.
b) Line (2) passing through the incisal edge of lower central incisors of the anterior ridge and parallel to the line (1).
c) Line (3) passing through the mid line of the cast and perpendicular to both lines (1) and (2).
d) On line 3, the midpoint between line (1) and (2) was determined and marked, (point a), which is the geographic center of the lower denture.
e) Line (4) passing through point (a) and running parallel to lines (1) and (2).
A trough was drilled at (point a) by round surgical bur. The bur maintained in the trough leaving about 25 mm of its length projecting from the cast. This length was the most appropriate length from which the application of force took place without endangering the upper jaw or being interfere with the tongue [27].
Preparation of the mandibular denture for the retention test
The finished mandibular denture was placed on duplicate cast after determination of its geographic center. Three 18 gauge orthodontic wire lopes were attached to lingual aspect of the denture, one at its midline and two posteriors at line (4), using self-cure acrylic resin. The three wire lopes were engaged by three metallic wires and the wires extended upwards to meet and joined in the geographic center of the denture, at the bur projecting from the cast base. A metallic loop was then used to join the three wires on the top of the bur [27].
Measuring the denture retention
The measurements were performed while the patient was sitting in an upright position with his head rested on the head rest and the lower occlusal plane parallel to the floor.
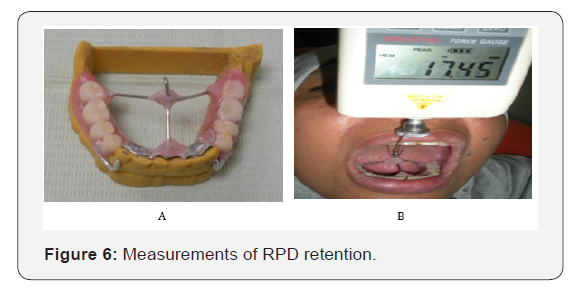
The metallic probe of the digital force gauge was attached to the metallic hook which is attached to the geometrical center of the mandibular partial denture (Figure 6A & 6B). The force gauge pulls the mandibular denture vertically upward until denture movement occurs. The force at which the denture dislodges was recorded in Newton. The process was repeated until three readings were taken, and the average was recorded. Data were collected, tabulated and statistically analyzed.
Statistical analysis
Measurements were taken for each group by digital gauge force-meter where used Newton (N) as a unit measure. Mean and standard deviation were calculated for further statistical study.
Exploration of data in Table 1 revealed normally distributed values using Kolmogrov-Smirnov normality test as P-value > 0.05. Using independent t test for comparison between both groups regarding retentive values, there was significant difference between both groups at different follow up periods as (P value < 0.05), listed in Table 2.
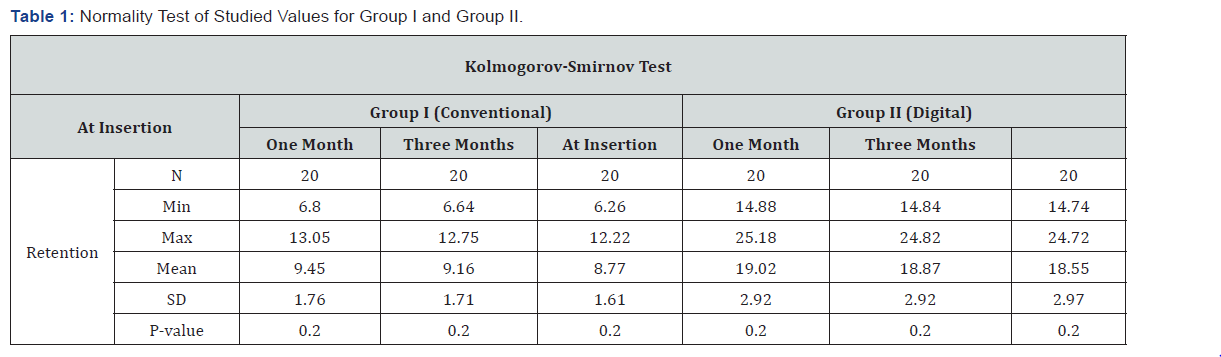
N: Number, Min: Minimum, Max: Maximum, M: Mean, SD: Standard deviation, P: Probability Level * Data set with a P-value > 0.05 rejects the null hypothesis that the data are from a normally distributed population.
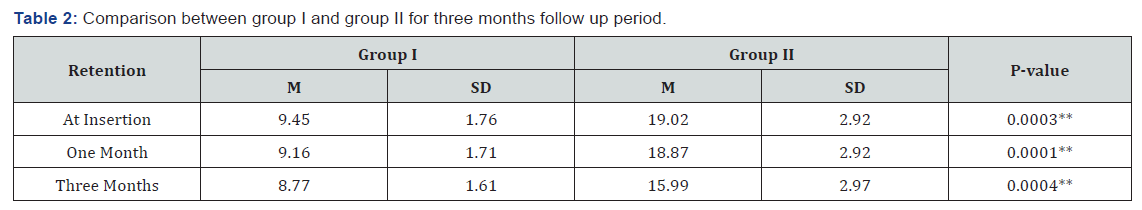
M: Mean, SD: Standard deviation, P: Probability Level, **significant difference.
For evaluating the effect of time on retention, mean change percentage was calculated for both groups for each follow up interval using the following equation
After mean change percentage calculation, one way analysis of variance (ANOVA) was performed to calculate the significance between different time intervals for each group followed by multiple comparisons using Tukey’s post-hoc test concluded that there was significant difference between different intervals for each group as (P-value < 0.05) except for group II as it was insignificant different between (insertion-three months) and (one-three months) intervals, listed in Table 3.
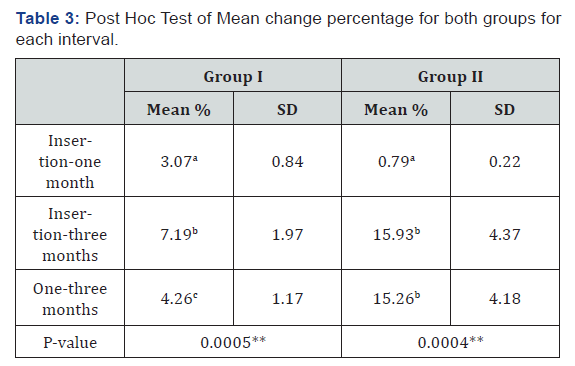
M%: Mean Percentage, SD: Standard deviation, P: Probability Level
Values with same superscript letter in the same column were insignificant different.
Values with different superscript letter in the same column were significant different.
**significant difference.
Discussion
Digital impression was introduced in dentistry in the mid- 1980s. The intra-oral scanner used in this study can record hard and soft tissue morphology accurately. A master cast prepared from an intraoral scanner eliminates the errors that may result from both the contraction of the impression material and the setting expansion of gypsum product. The accuracy of the 3D models made with digital impression was evaluated in a previous study and they reported a range of 50-70 microns which is close to the maximum precision of a milling machine [28]. Furthermore, Digital impressions present many advantages like less chair time, efficiency, ability of storing captured information and transferring digital images from the dental office to the laboratory [29].
Models surveyed by software are faster and more accurate in comparison to the manual surveying [30]. The mean retention values for digitally fabricated partial dentures recorded higher values than those of conventional dentures with statistically significant difference between both groups. This finding was also supported by a recent in vitro study evaluate the fit of cad cam manufactured one piece RPDs and concluded that their fit was better than those of traditional RPDs [31].
Also, these results were in accordance with another recent study by Wang et al, who fabricate RPD framework from a sacrificial pattern by SLA. They examined the quality of fit of both the sacrificial pattern and the casted framework and they found that it was subjectively estimated to be excellent [32]. Furthermore, the results of this study were also supported by Malara et al. [10], who found that the prosthesis which produced by CAD/CAM technology, adheres tightly to the tissue enhancing its retention, stability and transferring loads equally on the tissue, causing less interference in the oral mucosa [10].
Conventional fabrication methods include impression recording, pouring a stone model, manual surveying and blockout of undercuts. Then duplication of the modified master cast and constructing a wax pattern. Such steps necessitate considerable human intervention and materials manipulation that may additionally offer inherent processing shrinkage and/ or expansion. This may lead to increased processing errors and inaccuracies which may explain the decreased retention values of conventional dentures in comparison to those of digital dentures [32,33].
Conclusion
Within the limitations of this short-term clinical study the retention of digital RPD fabricated with digital impression, digital designing and casting a 3D printed pattern was higher than conventional RPD as it was associated with less human intervention.
References
- Vanzeveren C, D’Hoore W, Bercy P, Leloup G (2003) Treatment with removable partial dentures: a longitudinal study. Part I. J Oral Rehabil 30(5): 447-458.
- Knezović Zlatarić D, Celebić A, Valentić-Peruzović M, Jerolimov V, Pandurić J (2003) A survey of treatment outcomes with removable partial dentures. J Oral Rehabil 30(8): 847-854.
- Abuzar MA, Kahwagi E, Yamakawa T (2012) Investigating oral healthrelated quality of life and self-perceived satisfaction with partial dentures. J Investig Clin Dent 3(2):109-117.
- Wismeijer D, Tawse-Smith A, Payne AG (2013) Multicentre prospective evaluation of implant-assisted mandibular bilateral distal extension removable partial dentures: patient satisfaction. Clin Oral Implants Res 24(1): 20-27.
- Wu JH, Yang YH, Wang CH, Lee HE, Du JK (2012) Effects of denture maintenance on satisfaction levels of Taiwanese elderly using removable partial dentures: a pilot study. Gerodontology 29(2) :458- 463.
- Persson AS, Oden A, Andersson M (2009) Digitization of simulated clinical dental impressions: virtual three-dimensional analysis of exactness. Dent Mater 25(7): 929-936.
- Williams R, Bibb R, Rafik T (2004) A technique for fabricating patterns for removable partial denture frameworks using digitized casts and electronic surveying. J Prosthet Dent 91(1): 85-88.
- Williams R, Eggbeer D, Bibb R (2004) CAD/CAM in the fabrication of removable partial denture frameworks: a virtual method of surveying 3-dimensionally scanned dental casts. Quintessence Dent Technol 2: 268-276.
- El-Khamisy NE, Habib AH, El- Mekawy NE, Emera RM (2017) Digital versus Conventional Design For Mandibular Distal Extension RPD: A Study of Passivity of RPD Components and Principal Abutment Alveolar Bone Height Changes MJD 4: 6-13.
- Malara PA. Dobrzański LB, Dobrzańska JB (2015) Computer-aided designing and manufacturing of partial removable dentures. J Achiev Mater Manuf Eng 73(2): 157-164.
- Campbell SD, Cooper L, Craddock H, Hyde TP, Nattress B, et al. (2017) Removable partial denture: The clinical need for innovation. J Prosthet Dent 118(3): 273-280.
- Han J, Wang Y, Lü P (2010) A preliminary report of designing removable partial denture frameworks using a specifically developed software package. Int J Prosthodont 23(4): 370-375.
- Williams RJ, Bibb R, Eggbeer D, Collis J (2006) Use of CAD/CAM technology to fabricate a removable partial denture framework. J Prosthet Dent 96(2): 96-99.
- Cindy B, Guillaume B, Pascal B, Yannick G, Marion B, et al. (2017) Optical Impression and Removable Partial Denture: An Accurate and Actual Solution J Dent Oral Health 3(6): 1-4.
- Lima JM, Anami LC, Araujo RM, Pavanelli CA (2014) Removable partial dentures use of rapid prototyping. J Prosthodont 23(7): 588-591.
- Sun J, Zhang FQ (2012) The application of rapid prototyping in prosthodontics. J Prosthodont 21(8): 641-644.
- Webb PA (2000) A review of rapid prototyping (RP) techniques in the medical and biomedical sector. J Med Eng Technol 24(4): 149-153.
- Rahmati S, Farahmand F, Abbaszadeh F (2010) Application of rapid prototyping for development of custom‐made orthopedics prostheses: an investigative study. Int J Advanced Design and Manufacturing Technology 3(2): 11‐16.
- Santler G, Kärcher H, Gaggl A, Kern R (1998) Stereolithography versus milled three‐dimensional models: comparison of production method, indication, and accuracy, Comput Aided Surg 3(5): 248‐256.
- Sarment DP, Sukovic P, Clinthorne N (2003) Accuracy of implant placement with a stereolithographic surgical guide. Int J Oral Maxillofac Implants 18(4): 571‐577.
- van Noort R (2012) The future of dental devices is digital. Dent Mater 28(1): 3-12.
- Williams JM, Adewunmi A, Schek RM, Flanagan CL, Krebsbach PH, et al. (2005) Bone tissue engineering using polycaprolactone scaffolds fabricated via selective laser sintering. Biomaterials 26(23): 4817‐4827.
- Petzold R, Zeilhofer HF, Kalender WA (1999) Rapid protyping technology in medicine - basics and applications. Comput Med Imaging Graph 23(5): 277‐284.
- Tan KH, Chua CK, Leong KF, Cheah CM, Cheang P, et al. (2003) Scaffold development using selective laser sintering of polyetheretherketonehydroxyapatite biocomposite blends. Biomaterials 24(18): 3115‐3123.
- Gan N, Ruan Y, Sun J, Xiong Y, Jiao T (2018) Comparison of adaptation between the major connectors fabricated from intraoral digital impressions and extraoral digital impressions. Sci Rep 8(1):529.
- Etman MK, Bikey D (2012) Clinical performance of removable partial dentures: A retrospective clinical study. O J St 2(3): 173-181.
- Mostafa AZ (2015) Effect of the lingual ledge of neutral zone impression on the retention and stability of mandibular complete denture in elders with atrophied alveolar ridge. Tanta Dental Journal 12(2):111-118.
- Davidowitz G, Kotick PG (2011) The use of CAD/CAM in dentistry. Dent Clin North Am 55(3): 559-570.
- Kim SY, Kim MJ, Han JS, Yeo IS, Lim YJ, et al. (2013) Accuracy of dies captured by an intraoral digital impression system using parallel confocal imaging. Int J Prosthodont 26(2): 161-163.
- Hu F, Pei Z, Wen Y (2017) Using Intraoral Scanning Technology for Three-Dimensional Printing of Kennedy Class I Removable Partial Denture Metal Framework: A Clinical Report. J Prosthodont 28(2): 1-4.
- Ye H, Li X, Wang G, Kang J, Liu Y, et al. (2018) A Novel computer -Aided Design/computer assisted manufacture method for one-piece removable partial denture and evaluation of fit. Int J Prosthodont 2: 149-151.
- Wu J, Xiaobo W, Xianghui Z, Chunbao Z, Gao B (2012) A study on the fabrication method of removable partial denture framework by computer‐aided design and rapid prototyping. Rapid Prototyp J 18(4): 318-323.
- Wataha JC, Messer RL (2004) Casting alloys. Dent Clin North Am 48(2): 499-512.






























