Significance of Implant Distribution on a Screw-retained Implant-Supported Mandibular Hybrid Restoration of PEEK framework with Immediately Loaded Implants applying All-On-Six Protocol: A Two Years Clinical Study
Mostafa Helmy Mostafa Ahmed1, Henri Diederich2* and Enas Anter Abd El Ghaffar3
1Lecturer of Removable Prosthodontics, Cairo University, Egypt
2Dental surgeon, Dental Clinic Henri Diederich, Luxembourg
3Lecturer of Radiology, Cairo University, Egypt
Submission: May 08, 2018; Published: May 23, 2018
*Corresponding author:Henri Diederich, Dental surgeon, Dental Clinic Henri Diederich, 51 av Pasteur, L-2311Luxembourg, Europe, Tel: 00352621144664; Email: hdidi@pt.lu
How to cite this article:Mostafa H M A, Henri D, Enas A A E G. Significance of Implant Distribution on a Screw-retained Implant-Supported Mandibular Hybrid Restoration of PEEK framework with Immediately Loaded Implants applying All-On-Six Protocol: A Two Years Clinical Study. Adv Dent & Oral Health. 2018; 9(1): 555751. DOI: 10.19080/ADOH.2018.09.555751
Abstract
Objectives: The aim of this study was to compare the effect of the distribution of implants on a Screw-retained Implant-Supported Mandibular Full Arch Prosthesis with Immediately Loaded Implants utilizing All-On-Six Protocol, both clinically & radiographically. In addition to Patients’ satisfaction over two years of clinical investigation.
Materials & methods:For the purpose of this clinical study, fourteen patients with completely edentulous mandibular ridges with satisfactory bone quantity and quality were carefully selected to receive the screw-retained full arch mandibular prosthesis according to specific criteria. Patients were instinctively divided into two groups; First group (of seven patients) obtained an Implant-supported, fully-splinted screw-retained full arch mandibular prosthesis with immediate functional loading protocol utilizing 6 implants (placed in central incisors, canines & first molars regions Bilaterally), while Second group (of seven patients) obtained an Implant-supported, fully-splinted screw-retained full arch mandibular prosthesis with immediate functional loading protocol utilizing 6 implants (placed in first premolar, second premolar & first molars regions Bilaterally). The clinical & the radiographic outcomes of the Implants supporting the screw-retained full arch superstructure had been measured at time of implants insertion, 6 months and 12 months, 18 months & two years respectively. In addition, patients’ satisfaction was also measured utilizing a customized chart of question (A four-point scale).
Results:Regarding parametric data; repeated measures ANOVA test was used to study the changes by time within each group as well as to compare between the two groups. Bonferroni’s post-hoc test was used for pair-wise comparisons when ANOVA test is significant. Student’s t-test was used to compare between amounts of bone loss or gain in the two groups. Whereas for non-parametric data; Mann-Whitney U test was utilized to compare between the two groups. All data showed normal (parametric) distribution except for satisfaction scores data which showed non-normal (non-parametric) distribution.
Conclusion:Regarding this study, it may be concluded that proper distribution of immediately loaded implants used for supporting mandibular screw-retained implant-supported full arch restoration, through proper implant placement pattern results in favorable response in terms of clinical, radiographic outcomes as well as patients’ satisfaction. In addition, Both modalities presented a feasible treatment option for supporting a screw-retained mandibular prosthesis with better outcomes in first distribution pattern. Furthermore, the Bio-Hpp material used in implant supported prostheses had several benefits for the implant restorations such as lower chipping rate, reduces stress shielding, metal free, easily monitoring implant-abutment connection fit.
Keywords: Screw-retained restoration; Hybrid prosthesis; Implant distribution; Immediate loading; PEEK framework material
Introduction
Treatment of the edentulous mandible has always been one of the most challenging matters in dentistry [1-5]. Traditional full denture is the most common treatment modality for these cases. However, owing to lowered stability when compared with natural teeth or fixed partial dentures, patients often complain of struggle adapting to a removable prosthesis.
The introduction of osseointegrated implants has infinitely improved treatment consequences in patients with complete edentulism. Increased stability and retention of prostheses can be achieved by one of two means, either an implant-retained removable overdenture or an implant-supported fixed prosthesis [6-11].
Implant-retained dental restorations have verified to be a good solution for the rehabilitation of edentulous patients. The literature indicates that the implant-supported screw-retained prosthesis provides liable results with enhanced stability, function and a high degree of patient satisfaction compared to conventional removable dentures [12,13].
The oral rehabilitation of an edentulous patient treated through a fixed implant-supported prosthesis using appropriate biomechanical and prosthetic basics has been a target in oral implant research for the last years [14]. With the fixed implantsupported restoration, a satisfactory distribution of stress is highly significant to decrease implant and prosthetic failures [15]. Moreover, these failures can also be predisposed by several factors, including prosthetic design, implant number, implant distribution & occlusal scheme [16].
A common treatment strategy for an edentulous mandible is the placement of implants in the inter-foraminal region and a full arch fixed implant-supported prosthesis with distal cantilever [17-19]. However, this form of prosthesis can endorse a high level of stress that can be damaging to the implant and the surrounding bone because of the unfavorable lever arms [20]. For this reason, it has been recommended that the use of multiple implants in the anterior and posterior mandible could enhance the distribution of stress with more favorable implant support, avoiding lengthy cantilevers [21].
Completely edentulous patients with abundant bone height and width can be successfully restored with fixed implantsupported prostheses. The edentulous mandible can be restored successfully with an immediately-loaded implant-supported fixed prosthesis [22].
Immediate loading of dental implants permits immediate restoration of esthetics and functions with reduced morbidity of a second surgical intervention, and facilitates functional rehabilitation, consequently increasing patient acceptance and satisfaction. Furthermore, it eliminates the need for multiple and lengthy appointments that might affect the practitioner’s time for adjustment of provisional prostheses delivered to the patients during the healing period of delayed loaded implants [23-35].
An ideal stress profile is mandatory to preserve a strong and healthy jawbone: a stress that is too high might produce permanent injury to the jawbone; one that is too low may fail to stimulate the bone sufficiently for satisfactory healing of the wound and hence, for osseointegration. Moreover, the primary stability is especially crucial because the bone is still in a state of remodeling and dictates that the applied stresses to enhance bone growth [26-29].
Biomechanical considerations correlated to the stress transferred to the peri-implant bone and during function of the prosthesis might necessitate implants placement more distally, at premolar or molar regions, or to combine one anterior implant and the other posterior contralaterally [30].
Prosthetic management with a fixed, screw-retained restoration on four or six implants is a feasible concept as proposed by several authors [31]. Those techniques - frequently mentioned as all-on-four and all-on six - diminish or eliminate cantilever length by introducing implants in the distal regions. Following theses modalities, the entire dental arch could be securely rehabilitated.
Most of the studies examining all-on-four and all-on-six were performed using cylindrical implants. However, our knowledge regarding the increasingly popular tapered dental implants is pretty limited in this respect. Mostly, tapered implants appear to be superior to cylindrical implants for immediate loading as insertion torque has been proved to be the most rational prognostic factor for the Osseointegration of immediately loaded splinted implants [32].
Implant distribution in any dental arch can aid to reduce the stress applied separately on the implants. this could be achieved by bearing in mind the importance of the anteroposterior distance (A/P). The A/P spread measurement is a formula utilized to calculate the maximum specified cantilever length off the most posterior implant in a fixed restoration [33-35].
Undue force distribution pattern in peri-implant bone might trigger implant loss or mechanical failures in the prosthetic structure when the produced stresses and strains exceed the physiologic tolerance thresholds of the alveolar bone, consequently, certain studies have declared that the stresses beyond this threshold might cause marginal bone loss or complete loss of osseointegration [11].
Large cantilevers, parafunctional habits, improper occlusal designs and premature contacts may cause excessive loads which adversely affect the survival rate of the implants. Therefore, optimal occlusion within physiologic limits is an important factor to ensure the long-term implant success [36].
There is also a lack of randomized controlled trials (RCTs) to compare the outcome of specific enquiries related to the optimum distribution of implants used for screw-retained implantsupported superstructures [37].
Conventional metallic frameworks are the most commonly used modalities for implant-supported restorations. But the dark metal framework endures the natural esthetics. Recently, a paradigm shift in the replacement of all-ceramic framework for esthetic reasons.
Because of its mechanical advantages and high biocompatibility. The PEEK (Biohpp) framework material used in implant restorations develops many Advantages; the modulus of elasticity is close to that of bone that means during loading the bone related rotation can be reduced. Additional advantages are shock-absorbing, metal free restoration, low plaque accretion as well as no corrosion [38].
Polymer-based frameworks utilizing poly-ether-ether-ketone (PEEK) material has become an alternative predictable technique in screw-retained implant-supported full arch restorations. Moreover, use of prefabricated composite veneers for the restoration of full arch cases permits an aesthetic outcome similar to that for individual ceramic veneering [39].
The aim of this clinical study was to evaluate and compare the effect of two implant distribution patterns of mandibular implant-supported screw-retained restorations in terms of clinical and radiographic outcomes. The first pattern utilized six implants (placed in central incisors, canines & first molars regions bilaterally), while the second pattern utilized six implants (placed in first premolar, second premolar & first molars regions bilaterally).
The null hypothesis was that there will be no significant difference in outcomes between the two implant distribution patterns, over the whole investigation period.
Material and Methods
Fourteen patients were carefully selected from the outpatient clinic of the Removable department, Faculty of Oral and Dental Medicine, Cairo University. Where, patient selection was accomplished according to the following criteria:
a) Age ranged between 35-50 years.
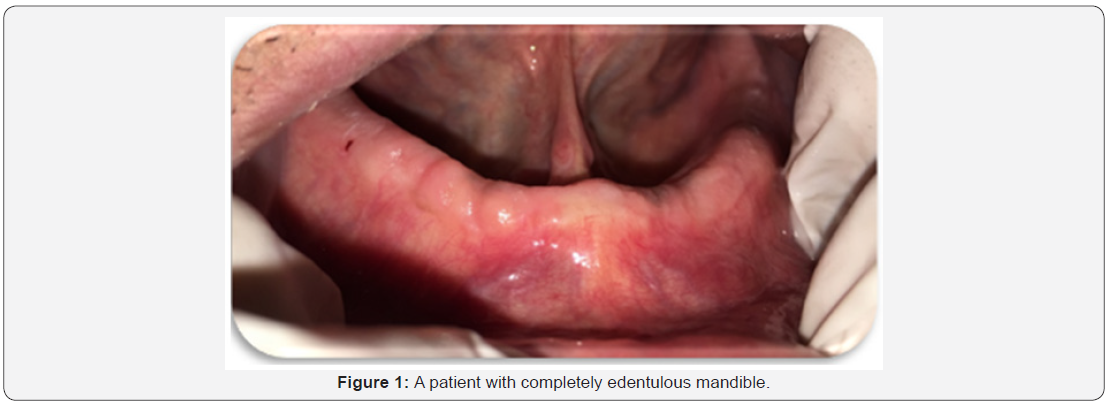
b) Patients with completely edentulous mandible (Figure 1).
c) Patients with good oral hygiene.
d) Patients free from bad oral habits.
e) Patients free from any systemic or debilitating diseases such as diabetes mellitus, bone diseases, blood discrasis or other diseases that affect bone healing around the implants.
f) Absence of any medical disorder that might obscure the surgical phase or disturb osseointegration.
g) Patients with Angle’s class І maxillo-mandibular relationship with normal occlusion.
h) Uncooperative patients were omitted & only cooperative patients were included in the study
The patients were asked for their approval to the conduction of the research & being recalled for follow-up appointments. All details were written & signed by the patients in consent forms. The study was conducted according to principles stated in Helsinki Declaration & being approved by the Faculty ethical committee. After taking full patient’s personal, medical and dental history, each patient received a thorough clinical and radiographic examination.
Construction of try-in mandibular denture
Upper and lower primary impressions were made utilizing alginate impression material1 according to the manufacturer’s instructions and poured into stone plaster2 to attain diagnostic casts over which acrylic resin3 special trays were fabricated.
a) For every patient, the casts were mounted on a simple hinge articulator aided by a Tentative inter-occlusal wax record. Afterwards, the occlusal relation between the upper and lower teeth was thoroughly examined.
Foot Note:
1Cavex alginate, dust free, high consistency, Holland
2Type III dental stone Lascod SP, sestofino, Italy
3Moldano. Bayer Leverkusen, pekatray, Germany
b) Final mandibular impressions were made by twostep rubber base impression material4 according to the manufacturer’s instructions.
c) Master casts were obtained, Occlusion blocks were constructed centric jaw relation was recorded using the traditional wax-wafer method.
d) Master casts were mounted on semi-adjustable articulator, where, the upper cast was mounted according to a face bow record & the lower cast was mounted by the aid of the recorded centric jaw relation record.
e) Setting-up of mandibular teeth then, Try-in stage was carried out in the usual manner
It is worth to clarify that all laboratory steps were made by the same dental technician in the same laboratory.
Patient imaging and case planning (Figure 2)
a) Duplication of the mandibular trial denture was encountered utilizing a radio-opaque material to construct radiographic stents for every patient.
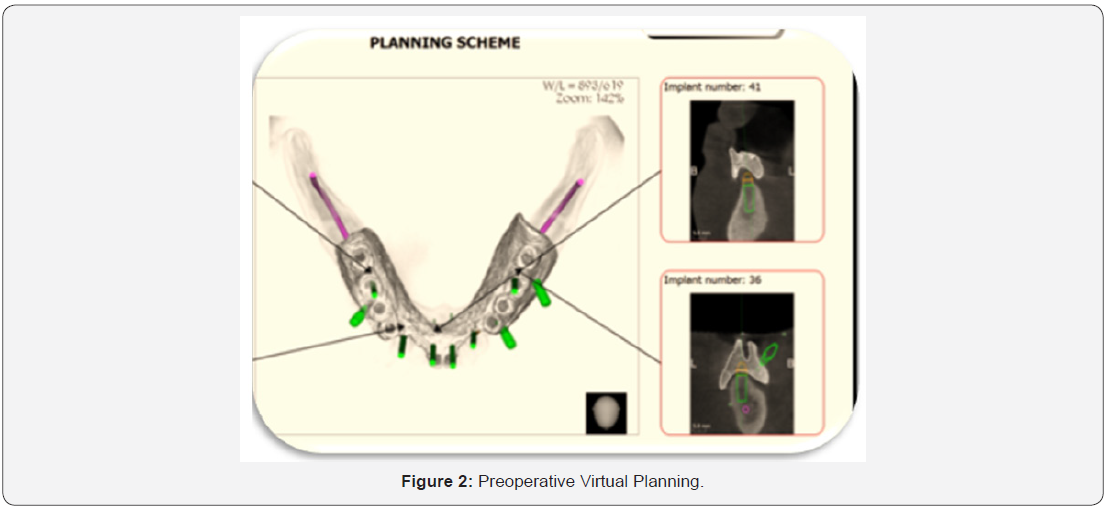
b) Patients were imaged using cone beam computed tomography scans (CBCT scans) through a cone beam CT machine (CBCT, i-CAT Vision)5. Each patient was instructed to bite on a piece of cotton to achieve adequate jaw separation. Finally, the resultant image was obtained as a DICOM file.
c) The images were processed using specialized image processing software (Blue Sky implant software)6.
Surgical guide fabrication
For Group [I]: Virtual implants were placed in the position of lower central incisors, canines & first molar teeth (bilaterally), A solid block was modeled & guiding holes denoting the implant direction were opened into the block & positioning sleeves were added.
For Group [II]: Virtual implants were placed in the position of first premolar, second premolar & first molars teeth (bilaterally). A solid block was modeled & guiding holes denoting the implant direction were opened into the block & positioning sleeves were added.
Pre-surgical steps
A. The surgical stent was sterilized chemically7 to be used during surgery.
B. The patient was instructed to take a prophylactic antibiotic preoperatively8 and to rinse with chlorohexidine mouth wash9 four hours before surgery.
Foot Note:
4Panasil, Katzenbach, Germany
5Imaging Sciences International, Hatfield, Pa, USA.
6Micro 10, A.B. Pharma.
7Blue Sky Bio, LLC
8Augmentin 625mg Beecham, MUP.
9Listerine mouthwash, USA.
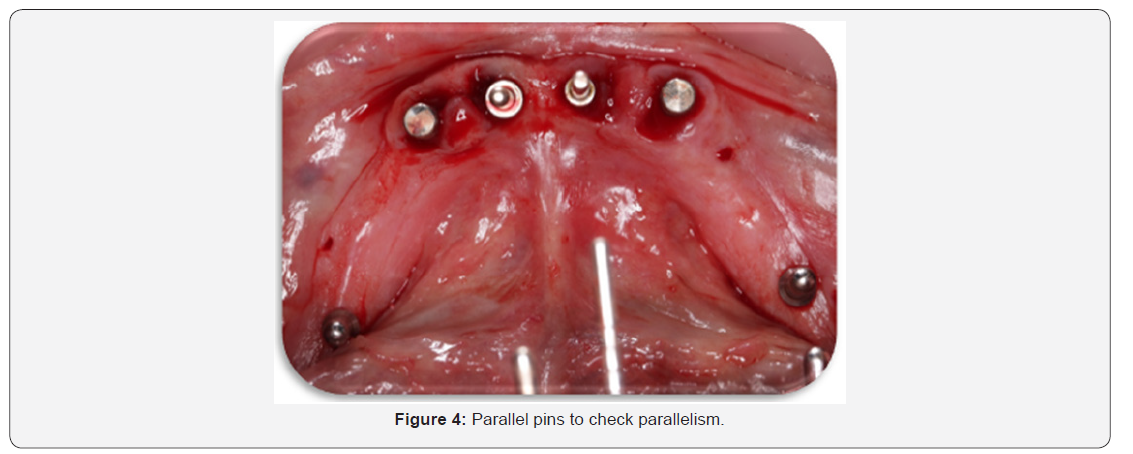
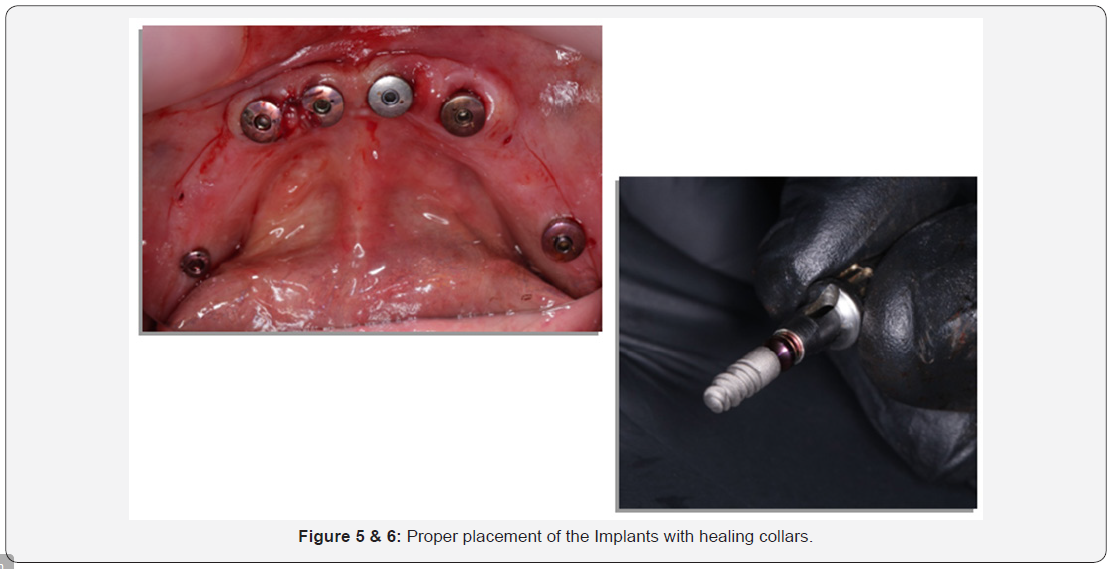
Surgical procedures (Figure 3-6)
One-stage surgery was followed, and the patients could wear their final prosthesis 5-7 days following surgery:

a) The entire surgical armamentarium was autoclaved.
b) The surgical places as well as the circumoral tissues were also disinfected by wiping them with antiseptic solution10.
c) Mandibular nerve block anaesthesia was given bilaterally, using 4% articaine anesthetic solution11. Also, field block anaesthesia was applied to diminish the bleeding as much as possible.
d) The fully computer-guided stent was introduced into the patient’s mouth, seated over the mandible & ensured accurate stability in place by the aid of an Occlusal Putty Index.
e) The computer-guided stent was then fixed in place by placement of three well distributed pins.
f) Osteotomy sites for the implants were sequentially performed using a series of drills until complete preparation of osteotomy sites.
g) The pins were easily detached, and the computer-guided stent was removed from the patient’s mouth.
Implant insertion in both groups
a) The sterile box of the implant12 was unwrapped, and then the inner vial was also opened & the implant osteotomy was washed thoroughly using sterile saline solution
b) The sterile implant was introduced into its site (according to the selected group), by screwing it using moderate finger pressure [self-tapping] Once resistance was felt, the abutment was unscrewed from the implant fixture & the ratchet wrench was adapted to the implant and the screwing process was continued.
c) The screwing process was stopped when the implant becomes flushed with the crest of the bone or preferably 0.5mm below the crestal bone level.
Then, utilizing the Osstell device13, four readings (buccal, lingual, mesial & distal) were obtained for each implant those readings represented the first clinical readings.
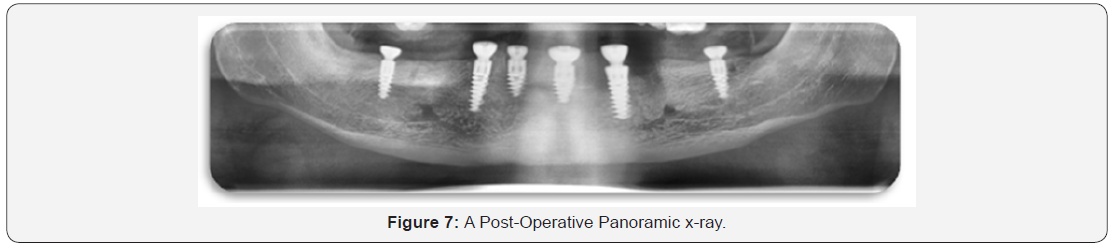
Finally, a Panoramic as well as CBCT radiographic pictures were obtained for the implants to ensure proper positioning. Whereas other separate radiographs were taken to be read out by the Digora computerized system to calculate the first radiographic readings (Figure 7).
Foot Note:
10Listerine mouthwash, USA.
11Listerine mouthwash, USA.
12ROOTT Two-piece Dental Implant, TRATE AG, Switzerland.
13Osstell AB, Sweden …
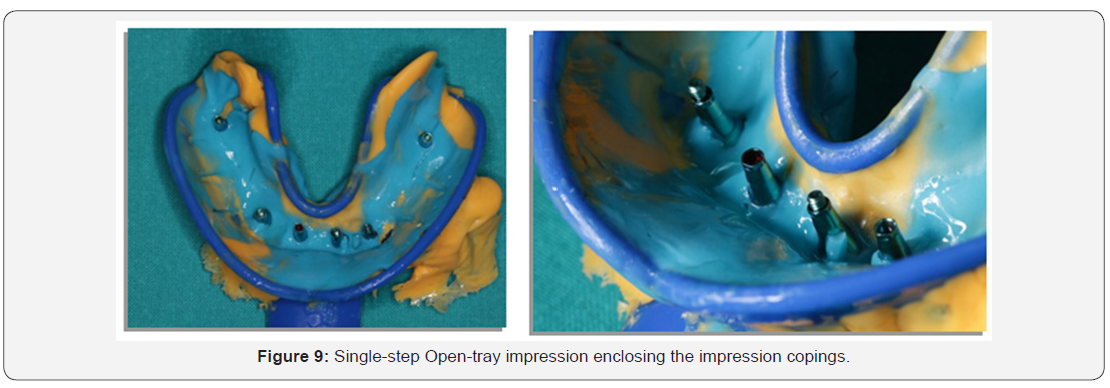
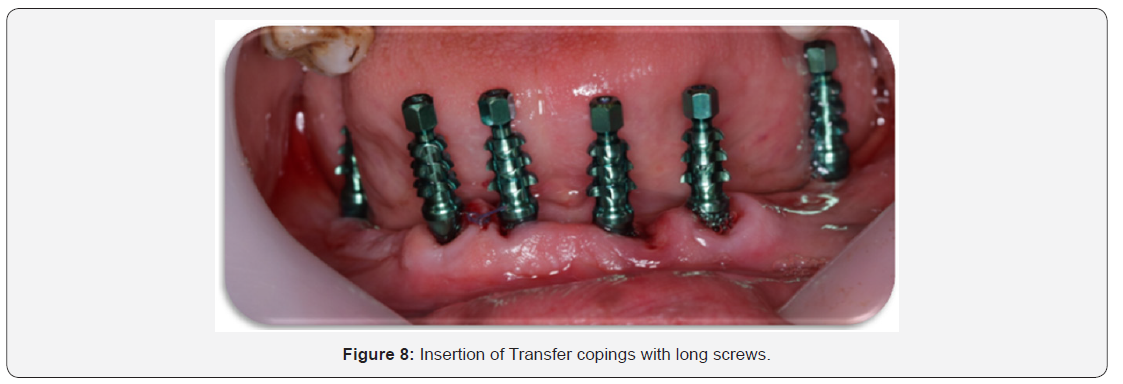
Restorative procedures: (Figure 8-19)
Directly following implant placement surgery, gingival formers were screwed onto corresponding implants, to ensure the need for any suturing required.
The gingival formers are then unscrewed from the implants and transfer copings with long screws were screwed into corresponding implants to start preparation of a single step Opentray impression (Implant level impression).
Windows were opened in a plastic stock tray (appropriate to the patient arch) opposite the transfers and widened mesiodistally, and then a single-step impression (utilizing Putty and light addition silicon rubber base impression)14 was made, as follows: Rapid dryness of the surgical field was accomplished using pieces of gauze. Then, a light-body impression material was injected around the implants necks and the transfer mounts, followed by insertion of the stock tray loaded by a putty rubber base impression material in the patient’s mouth. The tray was secured in place and detected for complete seating and finally, the open-tray impression making was completed by manipulating the oral tissues in the usual manner. Following complete setting of the impression material, the screw driver was utilized to unscrew those mounts from the implant fixtures. The tray was then removed from the patient’s mouth and the impression was cleaned, dried and checked for its accuracy in addition to enclosing the transfer mounts accurately in their places.
The gingival formers were placed onto the implants & secured in place & the patient was given important postoperative instructions
Post-surgical instructions
The patients were immediately given after surgery Diclofenac Sodium non-steroidal anti-inflammatory analgesic tablets (Voltaren 75mg)15. It was prescribed as one tablet three times daily for three days to reduce pain and swelling and were advised to follow the antibiotic regimen previously prescribed (Augmentin 1g) for 5-7 days. Patients were given the following instructions:
a) To apply ice packs for 10 minutes with 10 minutes intervals along a period of 3-4 hours immediately following surgery.
b) To follow strict oral hygiene protocol.
c) Asked for some recall appointments within the next days to complete the restorative procedures.
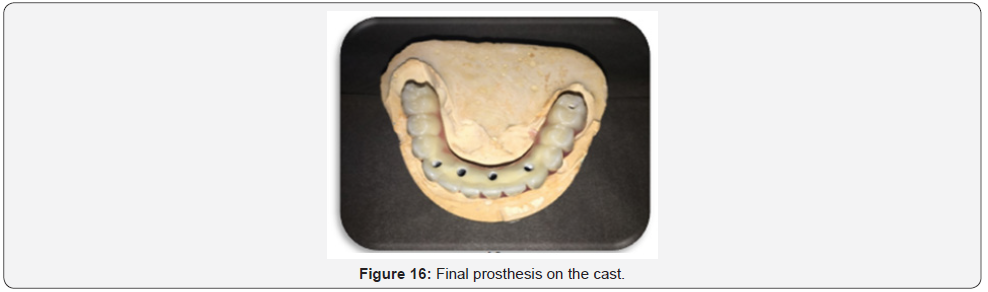
Laboratory Procedures
The implant analogues were fitted accurately into their corresponding mounts in the impression, using the screw driver.
In the laboratory, a small cotton pellet was utilized to varnish the impression surfaces surrounding the analogues with Vaseline. Then, a gingival mimic was created around the analogues using a plastic impression syringe loaded with a special gingival mimic material16 was performed, then impression was poured utilizing extra-hard stone to obtain a cast that enclosed the implant analogue part with attached abutment analogue were apparent from the cast.
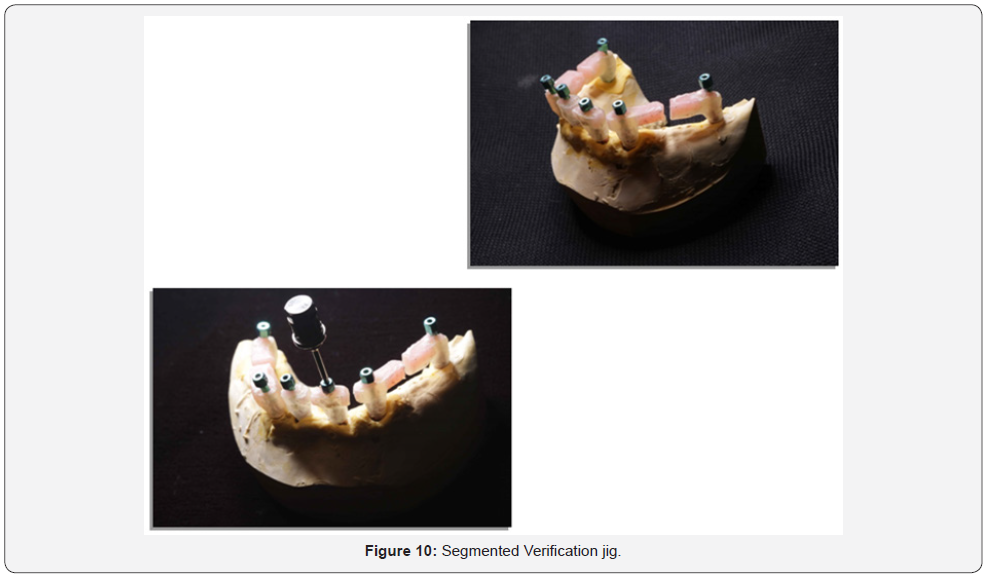
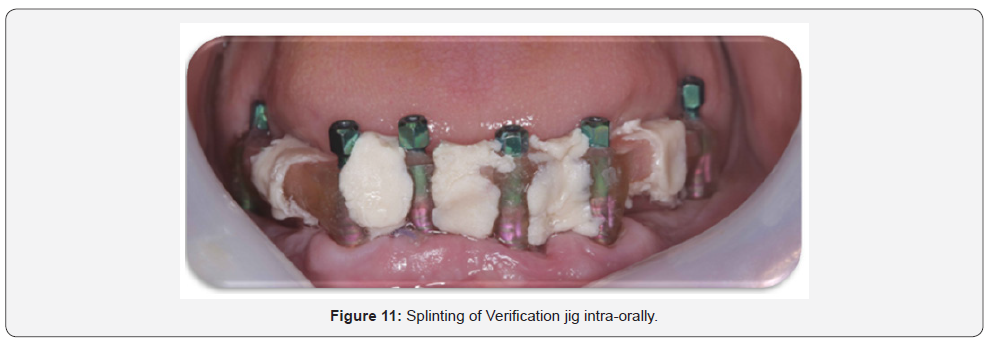
A custom tray, occlusion blocks and a segmented implant verification jig (IVJ) were fabricated. In the patient’s mouth, Evaluate the VDO, CR, esthetics, occlusion, phonetics and midline for a correct bite registration record utilizing the occlusion blocks, then, unscrew the gingival former in order to seat the verification jig in place
Verification jig
An implant verification jig (IVJ) that has been sectioned and numbered on a working model. Each acrylic section contains a titanium cylinder. This procedure should be followed to ensure an accurate final impression.
Seat each section of the jig onto the appropriate implant and tighten the guide pin. The sections should not be in contact. If necessary, remove one section, minimally trim it with a disc, and reseat it. Each section should have a gap about the thickness of a credit card. Visually verify gaps before luting. Then, lute the sections together with a suitable material17.
Allow the material to flow through and completely around the gaps. Ensure the material is completely cured. In addition, the clinician can test the passivity of the jig with a one-screw test. Tighten a single guide pin into one of the distal cylinders. No lifting of the jig should occur.
Check for a passive fit by visibly inspecting completely around each cylinder for complete seating. If any cylinder is not completely seated, the jig must be sectioned in that area, re-luted and rechecked until a passive fit is obtained.
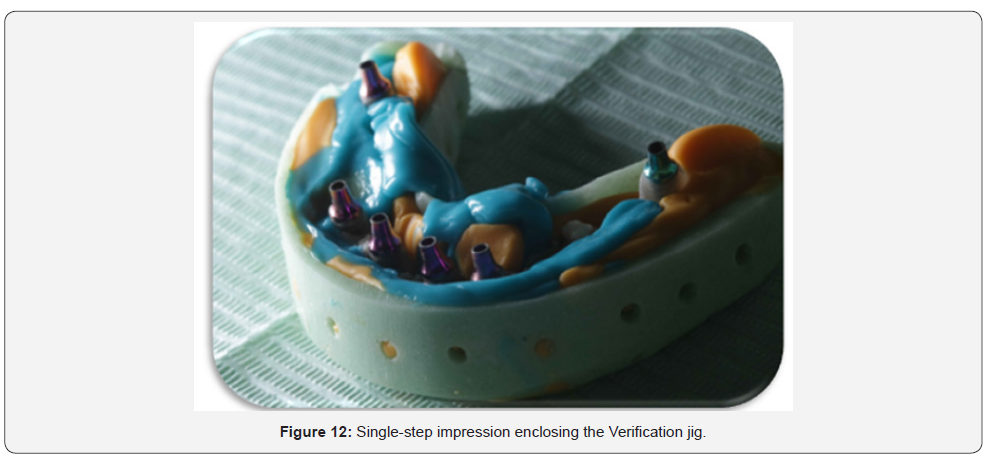
Final impression
Check the custom impression tray for proper fit (no contact with the jig or cylinders). Using a putty & light body VPS material, take the final impression with an open-tray technique in a single step, Inject light body VPS impression material under and around the jig to capture the ridge and all anatomical landmarks as for a full denture including full vestibular extensions (Figure 12).
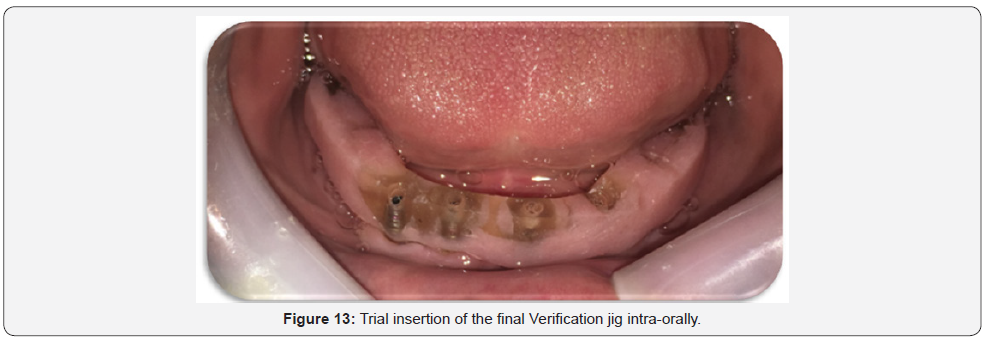
Completely fill the impression tray with putty VPS impression material. Seat the filled impression tray, ensuring the heads of the guide pins are exposed through the tray (Figure 13). Once the material has set, remove guide pins and then remove the impression; Ensuring that, the verification jig is picked up in the impression. Then, inspect the impression for the required details. And finally, replace the healing abutments again.
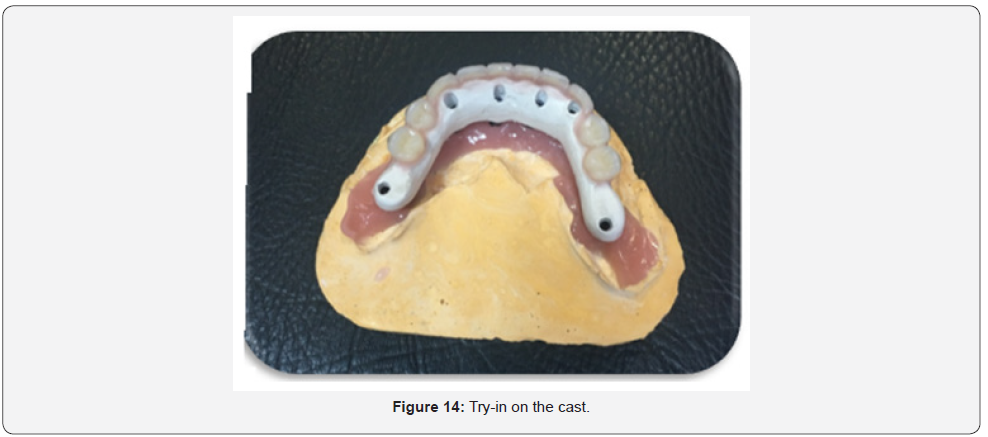
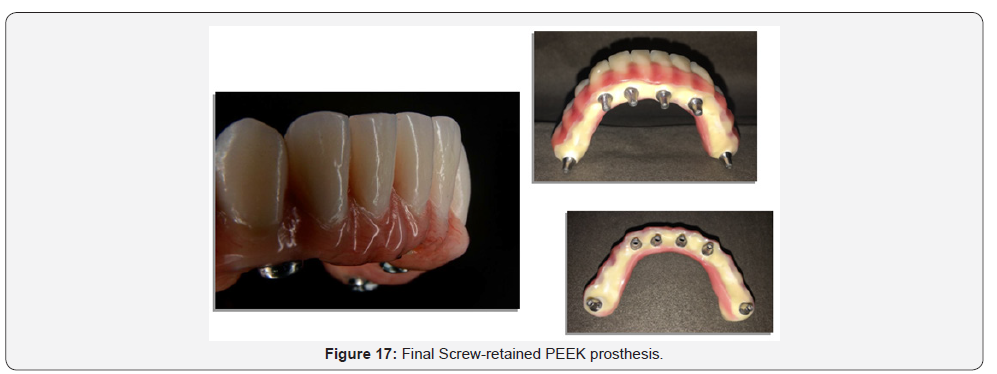
Framework try-in
The final implant-supported prosthesis framework was made using a precision-made custom CAD/CAM PEEK (BIOHPP) material18.
When receiving the PEEK framework from the Laboratory, remove the healing abutments, then check for the Passive fit of the PEEK framework which is critical for the long-term success of the case; this could be done by utilizing The single screw test, as follows; Tighten one screw and verify a passive fit on all of the implants (no lifting of the framework from any side). Remove the screw and repeat the process for each implant. Remove the framework & replace the healing abutments. Return the case to the Laboratory for setting up of teeth.
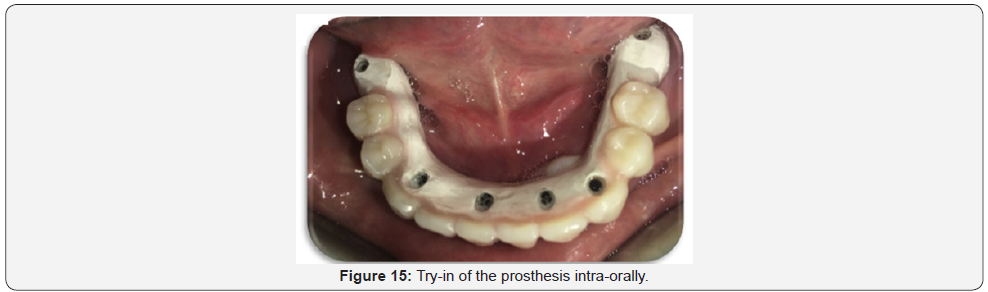
Final try in of framework with teeth
When receiving the PEEK framework with Visio-lign veneered teeth from the Laboratory, remove the healing abutments, and then check for the Passive fit (as previously done). Then, Verify the VDO, CR, occlusion, esthetics, shade, tooth arrangement, phonetics and midline (Figure 15). An articulating paper was utilized to detect any pressure areas, which were removed (if present) by spot grinding.
When accurate verification was assured, replace the healing abutments & return back the final try-in to the laboratory for processing into final restoration.
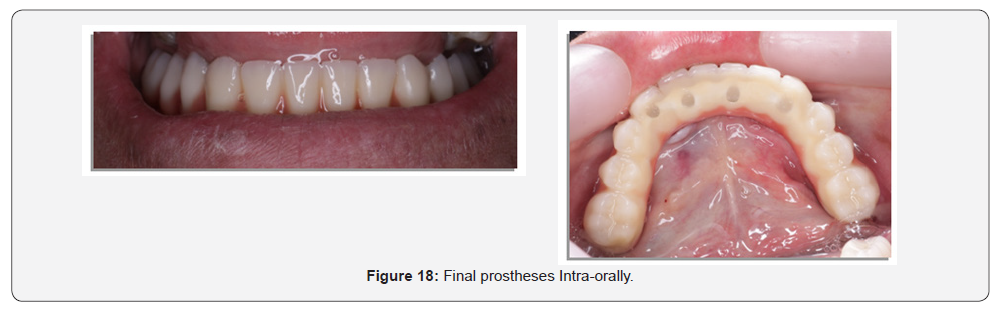
Delivery of final screw-retained denture
Remove the healing abutments, seat the final denture on the implants & hand tighten the prosthetic screws, alternating from one side to the other. Tighten the screws to the appropriate torque per manufacturer instructions. Wait approximately 5 minutes and retorque the screws. The occlusion was confirmed & any necessary adjustments were made. Then, place small amount of cotton in the screw access holes and fill with light cure composite prevent bacteria build-up. Final finishing and polishing of the light cured composite was then made.
Final adjustments & follow-up: After denture insertion and training the patient on easy insertion & removal of the denture; patients were instructed to follow strict oral hygiene measures and asked for a recall appointment every week in the first two months for any required denture adjustments &/or refinement of occlusion.
Clinical evaluation
This included the following:
Osstell measurements: A specially designed measuring tool termed “Smart Peg”19 was inserted with a special plastic cap (to measure the Implant Stability Quaint, ISQ), screwed into the internal surface of the implant. Then, utilizing the frequency transducer device “Osstell”20, four readings (buccal, lingual, mesial & distal) were obtained for each implant. Mean of the 4 readings will represent the ISO of that implant.
The procedure was repeated in other implants and finally, the mean of all implants ISQ was utilized to represent the mean Osstell reading in that stage. Measurements were made at time of implants insertion, 6 months, 12 months, 18 months and 24 months respectively
Radiographic evaluation: Direct digital radiography utilizing the Digora computerized system21 was applied for making intraoral digital radiographic images to assess the following:
a) Changes in the mesial and distal marginal bone height around the implants
b) Changes in bone density around the implants.
The imaging plate was introduced into a protective bag which was sealed by the Digora system. The stored images of every single patient were interpreted at the end of the follow up period. Digital images were made for the implants, immediately following their insertion, six months later and then every passing six months of the successive two years.
Image Analysis
The Digital images were used to analyze and evaluate the following:
Marginal bone height measurements (linear analysis)
Implant measurements were made as follow: The distance from the shoulder of the implant to the crest of the alveolar ridge, where a line was drawn tangential to the implant and parallel to its long axis. The mean value of both mesial and distal readings was taken, tabulated and statistically analyzed.
The procedure was repeated in other implants and finally, the mean of all implants measurements was utilized to represent the mean bone height reading in that stage.
The increase in the marginal bone height measurements denotes bone resorption.
Measurements of bone density (Radiometric/ Densitometric analysis):
The Digora system software was utilized for assessment of the changes in bone density mesial & distal to each implant. The measurements were as follows: Two lines were drawn; the first line extended mesial to the implant from the shoulder of the implant to the apex of the implant and parallel to its long axis, while the second line extended distal to the implant from the implant shoulder to its apex. Bone density alongside each of the two lines was documented and then the mean value of both readings was calculated for further assessment.
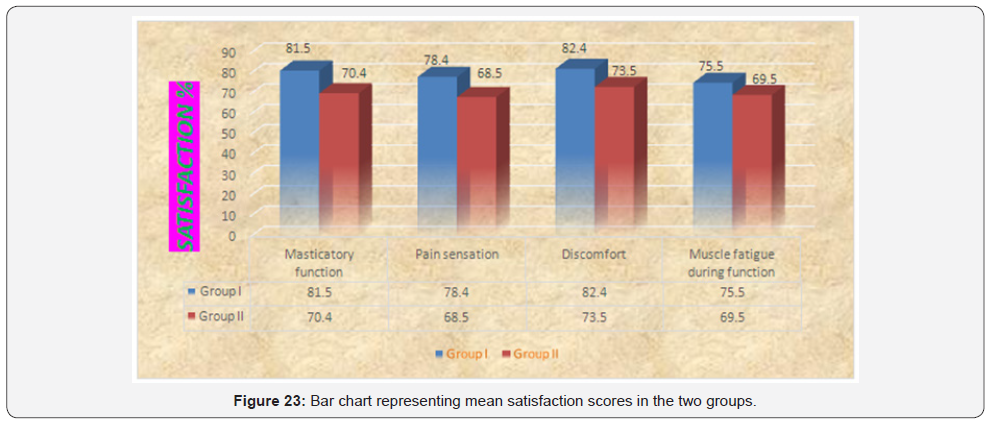
The procedure was repeated in other implants and finally, the mean of all implants measurements was utilized to represent the mean bone density measurement in that stage. Patients’ satisfaction was also measured (the day following prosthesis placement) utilizing a customized chart of question, where; Patients answered a series of questions to evaluate the IMPLANTSUPPORTED PROETHESIS in Both Groups (4 POINTS SCALE) in terms of; masticatory function, pain sensation, presence of any discomfort, muscle fatigue during function.
Finally, each patient had to give a number representing his General satisfaction (90-100%= Excellent, 80-89%= very good, 70-79%= good, 60-69%= fair, 50-59%= working, BELOW 50%= not satisfied) Regarding the previous questions.
a) Patients of both groups were asked for recall appointments every six months, following overdenture insertion till 2 years of implants insertion for measuring the clinical and radiographic outcomes.
b) All the results were calculated, tabulated and then statistically analyzed.
Results
Statistical analysis
Numerical data were explored for normality by checking the data distribution and using Kolmogorov-Smirnov and Shapiro- Wilk tests. All data showed normal (parametric) distribution except for satisfaction scores data which showed non-normal (non-parametric) distribution.
For parametric data, repeated measures ANOVA test was used to study the changes by time within each group as well as to compare between the two groups. Bonferroni’s post-hoc test was used for pair-wise comparisons when ANOVA test is significant. Student’s t-test was used to compare between amounts of bone loss or gain in the two groups. For non-parametric data, Mann- Whitney U test was used to compare between the two groups.
The significance level was set at P ≤ 0.05. Statistical analysis was performed with IBM® SPSS® Statistics Version 20 for Windows.
Osstell measurements
Comparison between the two groups: It revealed that at base line there was no statistically significant difference between the two groups. After 6, 12, 18 and 24 months; Group I showed statistically significantly higher mean Osstell values than Group II.
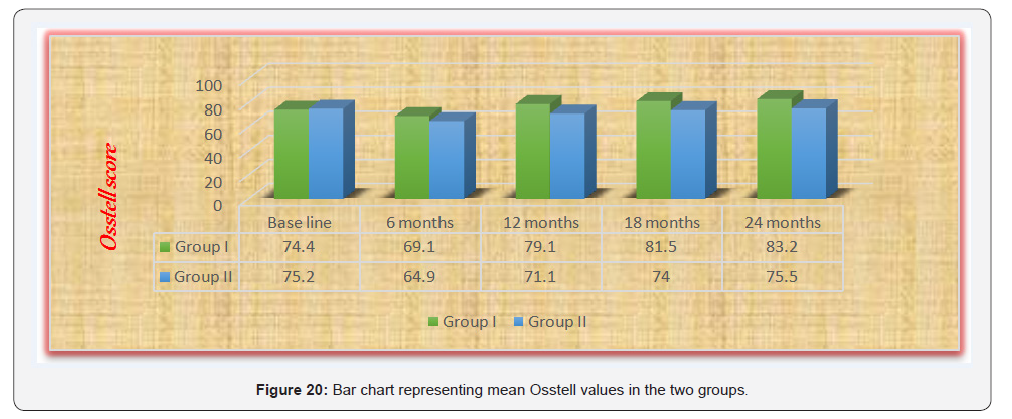
As regards the changes by time within each group: Both groups showed a statistically significant decrease in mean Osstell values after 6 months. From 6 months to 12 months, there was a statistically significant increase in mean Osstell values. From 12 months to 18 months as well as from 18 to 24 months, there was no statistically significant change in mean Osstell values. However, the mean Osstell value after 12 months showed statistically significantly higher values than base line measurement (Table 1 & Figure 20).
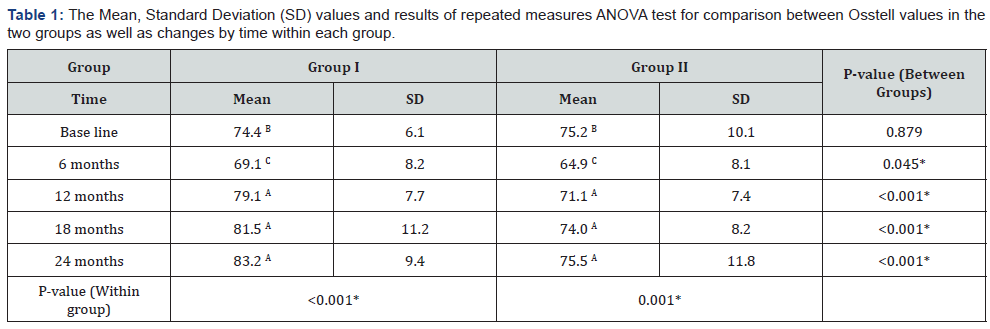
*: Significant at P ≤ 0.05, Different superscripts in the same column are statistically significantly different.
Bone height measurements
As regards Group I: A non-statistically significant increase in mean bone height measurements was detected after 6 months. From 6 months to 12 months; there was a statistically significant decrease in mean bone height measurements. From 12 months to 18 months as well as from 18 months to 24 months; a nonstatistically significant change in mean values was detected.
While in Group II: A statistically significant increase in mean bone height values was observed after 6 months. From 6 months to 12 months; there was non-statistically significant decrease in the mean bone height measurements. From 12 months to 18 months as well as from 18 months to 24 months; there was a statistically significant increase in the mean values.
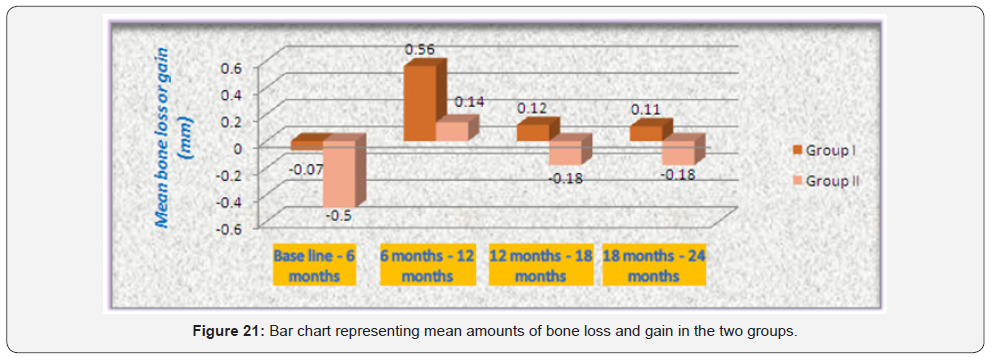
Comparison between amounts of bone loss or gain in the two groups: It revealed that after 6 months; Group I showed statistically significantly lower amount of bone loss than Group II. From 6 months to 12 months; Group I showed statistically significantly higher mean bone gain than Group II. From 12 to 18 as well as from 18 to 24 months; Group II showed statistically significantly higher mean amount of bone loss than Group I (which showed bone gain) (Table 2 & Figure 21).
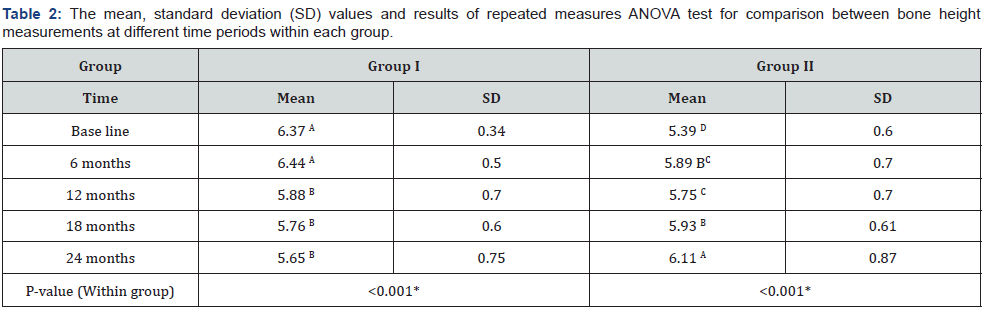
*: Significant at P ≤ 0.05, Different superscripts in the same column are statistically significantly different.
Bone density measurements
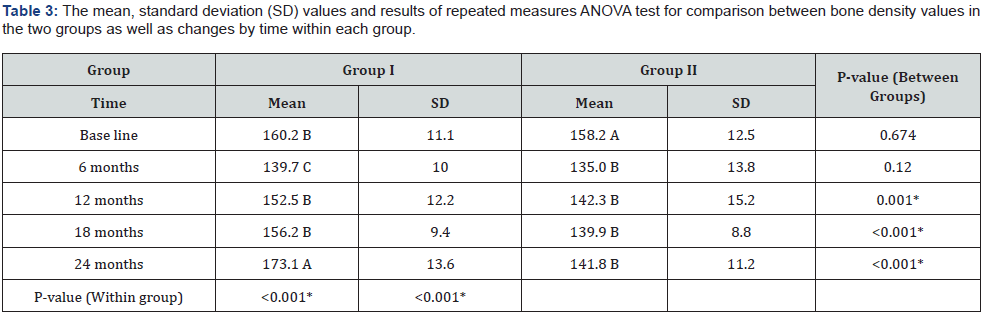
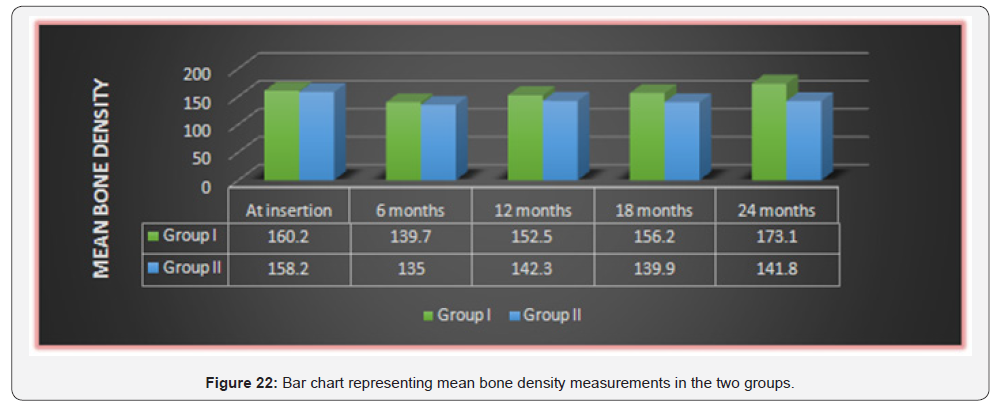
Comparison between the two groups revealed that at base line as well as after 6 months; there was no statistically significant difference between the two groups. After 12, 18 as well as 24 months; Group I showed statistically significantly higher mean bone density than Group II.
As regards the changes by time within Group I: There was a statistically significant decrease in mean bone density measurements after 6 months. From 6 months to 12 months, there was a statistically significant increase in mean bone density measurements. From 12 months to 18 months; there was no statistically significant change in mean values. From 18 months to 24 months; there was a statistically significant increase in mean bone density. The mean bone density after 24 months showed statistically significantly higher mean value than base line measurement.
While in Group II: There was a statistically significant decrease in mean bone density measurements after 6 months. From 6 months to 12 months, 12 months to 18 months as well as 18 months to 24 months; there was no statistically significant change in mean bone density measurements. However, the mean bone density after 24 months showed statistically significantly lower value than base line measurement (Table 3 & Figure 22).
*: Significant at P ≤ 0.05, Different superscripts in the same column are statistically significantly different.
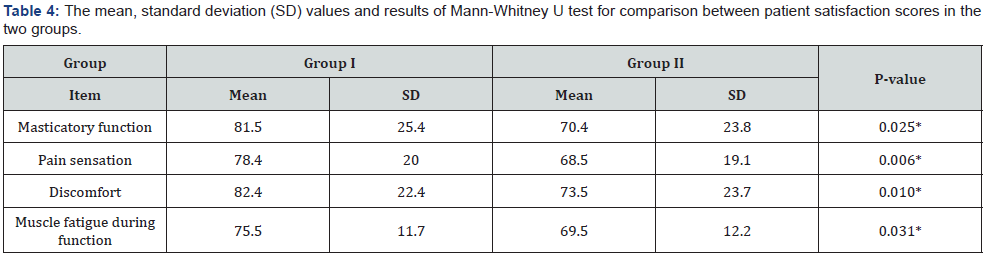
Patient satisfaction
Comparison between the two groups revealed that Group I showed statistically significantly higher mean satisfaction scores than Group II regarding all items of the questionnaire (Table 4 & Figure 23).
*: Significant at P ≤ 0.05.
Discussion
Discussion of Methodology
In this study, all factors that could affect the osseointegration of implants were carefully considered during patient selection and later after restoration. These factors may be biological or mechanical or both; The biological factors could be related to the patient’s selection, to the steps of implant installation and to the level of oral hygiene measures followed [40].
Fourteen healthy patients of edentulous mandibles of age ranging from 35-50 years old were included in this study to avoid any fluctuation in bone changes that might affect the obtained results. Maintenance of good oral hygiene has a great influence on the success of this study to the extent that it has a great impact on the osseointegration process. The oral hygiene of each patient was, therefore, evaluated at the beginning of the study and then throughout the whole investigation period.
Patients with superior general health were only selected, to avoid the reflection of any systemic disorder on the bone condition, and hence, osseointegration [35]. Only cases with normal maxillamandibular relation were included in the study to avoid the effect of transmission of abnormal forces to the implants.
Uncooperative patients were excluded, where only cooperative patients were included in the study to ensure their commitment to the oral hygiene measures and the regular follow up visit.
Bone quality and quantity were evaluated radiographically to ensure primary stability of the implant at the time of its placement. In addition, patients with sufficient bucco-lingual width at sites of implants placement were only selected to ensure at least one mm. thickness of bone remaining buccal and lingual to the implant after its placement [41].
Construction of a computer-guided surgical stent was carried out, to ensure accuracy of implant placement in the three dimensions as well as decreasing the human interfering factors that might affect the adjustment of implants angulation [37].
All implants used were Two-piece, threaded, self-tapping, root form implants, 12mm length and 3.8mm width. This implant design was used to ensure primary stability during the initial healing period, as well as, increasing the contact area between the implant and the surrounding bone for better osseointegration [42].
Panoramic radiograph was the imaging modality of choice in evaluating implants osseointegration, to avoid the metallic artifacts that accompany CBCT (due to presence of multiple implants) [43] In addition, post-operative CBCT was performed also to ensure accurate duplication of pre-operative planning
The cases were followed up for Two years to ensure proper evaluation of clinical & radiographic parameters as well as patients’ satisfaction throughout a suitable period of time.
Discussion of Results
An implant supported, screw-retained hybrid prosthesis that consists of minimalized framework enclosed in a bulk of PEEK material and artificial teeth in order to prevent overloading of the implants and to ensure a more acceptable esthetics. Obviously, the distribution of the load applied to the superstructure (i.e. the prosthesis) is more favorable when the superstructure is supported by well distributed six implants (in Group I), than in Group II.
Biomechanical implant complications have been related to several factors such as the bone quality, implant surface characteristics, presence of parafunctional habits and prosthetic design as well as implant number and distribution.
In implant-supported fixed prostheses, an ideal biomechanical distribution of stresses at the prosthetic superstructure and implant infrastructure is of dominant importance, being affected by several factors such as correct prosthetic design and occlusal scheme. Furthermore, attaining less stress in an implantsupported restorative system is one of the main goals of implant treatment.
Oral rehabilitation with implant-supported hybrid restoration in completely edentulous mandibles offers a wide range of treatment modalities based on the varying number & distribution of implants utilized, as well as the loading behaviors approached [44].
Criteria for the successful immediate loading of dental implants were strictly followed in this study according to the guidelines advocated by several authors [45,46] Clinical assessment of primary implant stability was ensured by the insertion torque at the moment of implant placement, which was no less than 30N. cm in almost all cases. This torque is considered by some authors [47-50] as the minimum torque necessary for osseointegration in cases of immediately loaded implants.
Tapered implants used in this study possess a progressive thread design, which is grit blasted to produce a sharp edge and a rough surface, ensuring fast cellular adhesion and osseointegration, high primary mechanical stability in bone immediately after their placement, and increased total surface contact with surrounding bone [51].
In the present work, properly distributed implants in Group (I) presented better clinical & radiographic outcomes, which might be attributed to better antero-posterior distance (AB distance) than present in Group (II).
A study of stress analysis has shown that frameworks constructed with a precise and passive fit induce significantly smaller amounts of stress on the implant [39] and this could be achieved by use of Verification jigs
Immobilization of the implants in the early healing phase was particularly important (early healing phase), where it acts as a splint by remaining firmly placed on the implants. Moreover, functional load was minimized by a soft diet in the first month of prosthesis insertion [52].
In the current study, the installation of posterior implants in both groups was used to decrease the lever arm, allowing greater posterior extension and increased occlusion scheme in the mandibular fixed implant-supported prosthesis, which provided a better distribution of occlusal forces and increased the prosthesis stability.
The statistically significant decrease in the mean Osstell measurements from base line to six months might be attributed to the inflammatory, resorptive and remodeling activities during the healing process.
These findings were in line with those studies which concluded that; although new implant surface and chemistry designs have shortened and improved osseointegration, the initial implant stability drop is still present and remains a challenge for future research and development [53].
Moreover, the mechanism behind the decrease of measurements during the first six months might be related to the changes of bone-implant interface as well as the properties of the surrounding bone (i.e. the interfacial stiffness). Firstly, the tapered implant creates a lateral compression of the bone tissue during insertion and it is likely that the relaxation of the inbuilt stresses between the implant and bone occurred after implant placement, which can be considered as a decrease in scores. Secondly, it can be speculated that loading might induce microfractures in the surrounding bone. These were in line with many similar studies [43].
The statistically significant increase in the mean Osstell readings from six months to twelve months of prosthesis insertion, indicating greater implant osseointegration [44]. The statistically significant increase in the mean Osstell readings from base line to twelve months matched the time frames of bone formation and maturation around the dental implants [44].
The significant increase in the mean bone height measurements in both groups, indicating increased crestal bone resorption in the first six months compared to those measurements from six to twelve months, which might be explained by the continuous remodeling process of bone surrounding the implant resulting in bone resorption, followed by bone deposition [45].
The crestal bone resorption around implants is a well-known phenomenon occurring mostly in the initial phase of functional implant loading and considered as an immediate bone response after insertion of the implant supported prosthesis. The mean marginal bone loss in the present study from base line to twelve months is considered within accepted permissible limits occurring with most dental implants [36].
Concerning changes of bone density around the implant, it was evident that there was a significant decrease of mean values of bone density at the first six months in both groups. This was mainly attributed to the surgical trauma during implant surgery. In addition to, the precautions given to the patient to maintain soft diet during the initial phase of treatment [46].
Peri-implant bone density measurements were our concern in this study as an evaluation of the overall bone response to the selected treatment protocols regarding distribution of immediately loaded implants supporting mandibular overdentures. The immediate loading protocol was preferred to the traditional delayed loading protocol according to the encouraging results of Barone et al. [22] who found that bone was significantly denser around immediately loaded than unloaded oral implants.
The statistically significant increase in the bone density measurements in periods from six to twelvemonths, indicating favorable bone reaction to the applied forces that were within the physiologic limit tolerated by the bone and hence, favorable progress of the osseointegration process.
During the recall periods of all patients, there were no complaints from the installed implant and all the patients followed the oral hygiene instructions to avoid any harmful effect which might influence the results of this study [54]. Several studies declared that, the patients’ quality of life had been improved by the increased retention and stability of their implant-supported fixed prostheses [45].
The statistically significant difference in patients’ satisfaction between the two groups throughout the whole study period showed that implant distribution would affect the efficiency of the used prosthesis [44]. The results of the present clinical investigation were in contradiction of the null hypothesis previously established.
Conclusion
Within the limits of this clinical research study, concerning the relatively small sample size, it could be conservatively determined that:
a) This study was conducted to compare the effect implant distribution on screw-retained, immediately-loaded mandibular hybrid prosthesis with immediate functional loading protocol.
b) The clinical & the radiographic outcomes of the Implants supporting the screw-retained full arch super structure had been calibrated at time of implants insertion, 6 months and 12 months, 18 months & two years respectively. In addition, patients’ satisfaction was also measured utilizing a customized chart of question (A four-point scale).
From the results of this study, the following conclusions could be achieved:
a) Within the limitations of this study, it may be concluded that proper distribution of immediately loaded implants used for supporting mandibular screw-retained implant-supported full arch restoration, through proper implant placement pattern results in favorable response in terms of clinical, radiographic outcomes as well as patients’ satisfaction.
b) Both modalities presented a feasible treatment option for supporting a screw-retained mandibular prosthesis with better outcomes in first distribution pattern.
c) The Bio-Hpp material used in implant supported prostheses had several benefits for the implant restorations such as lower chipping rate, reduces stress shielding, metal free, easily monitoring implant-abutment connection fit.
d) The use of composite veneering material allows a high aesthetic acceptance with a reduced complication rate.
e) Use of the combination of a PEEK- framework with resin veneering showed a good alternative modality in implantsupported full arch restorations.
f) Enhanced clinical investigations with larger sample sizes and over longer periods of time, are still needed.
References
- Jun RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS (2012) Systemic review of the survival rate and incidence of biologic, technical and esthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin.Oral Implants Res 23(suppl 6): 2-21.
- A G Paleari, C D Presoto, J A Vasconcelos, Nunes Reis JM, Pinelli LA, et al. (2015) An alternative technique for fabrication of frameworks in an immediate loading implant fixed mandibular prosthesis. Case Reports in Dentistry 2015: 102189.
- Nokar S, Naini RB (2005) The effect of superstructure design on stress analysis, International Journal of Oral & Maxillofacial Implants 20(4): 533-539.
- Attard NJ, Zarb GA (2005) Immediate and early implant loading protocols: a literature review of clinical studies. J Prosthet Dent 94(3): 242-258.
- Becker W, Goldstein M (2008) Immediate implant placement: treatment planning and surgical steps for successful outcome. Periodontol 2000 47(1): 79-89.
- Bernardes SR, de Araujo CA, Neto AJ, Simamoto Junior P, das Neves FD (2009) Photoelastic analysis of stress patterns from different implantabutment interfaces. Int J Oral Maxillofac Implants 24(5): 781-789.
- Blanes RJ (2009) To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res 20(suppl 4): 67-72.
- C Law, V Bennani, K Lyons, M Swain (2014) Influence of implant framework and mandibular flexure on the strain distribution on a Kennedy class II mandible restored with a long-span implant fixed restoration: a pilot study,” Journal of Prosthetic Dentistry 112(1): 31- 37.
- Fischman B (1990) The rotational aspect of mandibular flexure. J Prosthet Dent 4(4): 483-485.
- Zarone F, Apicella A, Nicolais L, Aversa R, Sorrentino R (2003) Mandibular lexure and stress build-up in mandibular full-arch fixed prostheses supported by osseointegrated implants. Clin Oral Implants Res 14(1): 103-114.
- Capelli M, Zuffetti F, Del Fabbro M, Testori T (2007) Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: a multicenter clinical study. Int J Oral Maxillofac Implants 22(4): 639-644.
- Carl E Misch (2005) Mandibular Full-Arch Implant Fixed Prosthetic Options: În: Misch C.E. Dental Implant Prosthetics, Elsevier Mosby, St Louis, pp. 256-264.
- Crespi R, Vinci R, Cappare P, Romanos GE, Gherlone E (2012) A clinical study of edentulous patients rehabilitated according to the “all on four” immediate function protocol. Int J Oral Maxillofac Implants 27(2): 428- 434.
- Degidi M, Nardi D, Piattelli A (2009) Immediate rehabilitation of the edentulous mandible with a definitive prosthesis supported by an intraorally welded titanium bar. Int J Oral Maxillofac Implants 24(2): 342-347.
- Esposito M, Grusovin MG, Willings M, Coulthard P, Worthington HV (2007) The effectiveness of immediate, early, and conventional loading of dental implants: a Cochrane systematic review of randomized controlled clinical trials. Int J Oral Maxillofac Implants 22(6): 893-904.
- Francetti L, Rodolfi A, Barbaro B, Taschieri S, Cavalli N, et al. (2015) Implant success rates in full-arch rehabilitations supported by upright and tilted implants: a retrospective investigation with up to five years of follow-up. J Periodontal Implant Sci 5(6): 210-215.
- Gallucci GO, Benic GI, Eckert SE, Papaspyridakos P, Schimmel M, et al. (2014) Consensus statements and clinical recommendations for implant loading protocols. Int J Oral Maxillofac Implants 29(suppl): 287-290.
- Jacques LB, Moura MS, Suedam V, Souza EA, Rubo JH (2009) Effect of cantilever length and framework alloy on the stress distribution of mandibular-cantilevered implant-supported prostheses. Clin Oral Implants Res 20(7): 737-741.
- Sahin S, Cehreli MC, Yalcin E (2002) The influence of functional forces on the biomechanics of implant-supported prostheses--a review. J Dent 30(7-8): 271-282.
- Kwon T, Bain PA, Levin L (2014) Systematic review of short- (5-10 years) and long-term (10 years or more) survival and success of fullarch fixed dental hybrid prostheses and supporting implants J Dent 42(10): 1228-1241.
- Millen C, Bragger U, Wittneben JG (2015) Influence of prosthesis type and retention mechanism on complications with fixed implantsupported prostheses: a systematic review applying multivariate analyses. Int J Oral Maxillofac Implants 30(1): 110-124.
- Paniz G, Stellini E, Meneghello R, Cerardi A, Gobbato EA, et al. (2013) The precision of fit of cast and milled full-arch implant-supported restorations. Int J Oral Maxillofac Implants 28(3): 687-693.
- G A Zarb, J Hobkirk, S Eckert, R Jacob (2013) Prosthodontic Treatment for Edentulous Patients: Complete Dentures and Implant-Supported Prostheses, (13th edition), Mosby, St. Louis, USA.
- Ali B CE, Meddah HM, Merdji A, Bouiadjra BAB (2013) Effects of overloading in mastication on the mechanical behaviour of dental implants. Materials and Design 47(1): 210-217.
- C Law, V Bennani, K Lyons, M Swain (2012) Mandibular flexure and its significance on implant fixed prostheses: a review. Journal of Prosthodontics 21(3): 219-224.
- Castellon P, Blatz MB, Block MS, Finger IM, Rogers B (2004) Immediate loading of dental implants in the edentulous mandible. J Am Dent Assoc 135(11): 1543-1549.
- Krennmair S, Weinlander M, Forstner T, Krennmair G, Stimmelmayr M (2016) Factors affecting peri-implant bone resorption in four Implant supported mandibular full-arch restorations: a 3-year prospective study. J Clin Periodontol 43(1): 92-101.
- Patzelt SB, Spies BC, Kohal RJ (2015) CAD/CAM-fabricated implantsupported restorations: a systematic review. Clin Oral Implants Res 26(suppl 11): 77-85.
- Drago C, Howell K (2012) Concepts for designing and fabricating metal implant frameworks for hybrid implant prostheses. J Prosthodont 21(5): 413-424.
- Small BW (2009) Maxillary immediately loaded fixed hybrid prosthesis: A case report. Gen Dent 57(1): 10-13.
- Balkaya MC (2014) Investigation of influence of different implant size and placement on stress distribution with 3-dimensional finite element analysis. Implant dent 23(6): 716-722.
- RB Naini, S Nokar (2009) Three-dimensional finite element analysis of the effect of 1-piece superstructure on mandibular flexure. Implant Dentistry 18(5): 428-437.
- Penarrocha Diago MA, Maestre Ferrin L, Demarchi CL, Penarrocha Oltra D, Penarrocha Diago M (2011) Immediate versus nonimmediate placement of implants for full-arch fixed restorations: a preliminary study. J Oral Maxillofac Surg 69(1): 154-159.
- Soydan SS, Cubuk S, Oguz Y, Uckan S (2013) Are success and survival rates of early implant placement higher than immediate implant placement? Int J Oral Maxillofac Surg 42(4): 511-515.
- Kern JS, Kern T, Wolfart S, Heussen N (2016) A systematic review and meta-analysis of removable and fixed implant-supported prostheses in edentulous jaws: post-loading implant loss. Clin Oral Implants Res 27(2): 174-195.
- Elsyad MA, Hammouda NI (2017) Expansion of mandibular knifeedge ridge and simultaneous implant placement to retain overdentures: One-year clinical and radiographic results of a prospective study. Clin Implant Dent Relat Res 19(1): 167-179.
- Strassburger C, Kerschbaum T, Heydecke G (2006) Influence of implant and conventional prostheses on satisfaction and quality of life: A literature review. Part 2: Qualitative analysis and evaluation of the studies. Int J Prosthodont 19(4): 339-348.
- Kuoppala R, Näpänkangas R, Raustia A (2013) Quality of Life of Patients Treated With Implant-Supported Mandibular Overdentures Evaluated With the Oral Health Impact Profile (OHIP-14): a Survey of 58 Patients. J Oral Maxillofac Res 4(2): e4.
- Wong N (2016) Future Trends in Implant Dentistry: Digitally Guided Surgery and Prosthetics. Dent Today 35: 86-91.
- Greco GD, Jansen WC, Landre Junior J, Seraidarian PI (2009) Stress analysis on the free-end distal extension of an implant-supported mandibular complete denture. Braz Oral Res 23(2): 182-189.
- Vogl S, Stopper M, Hof M, Wegscheider WA, Lorenzoni M (2015) Immediate occlusal versus non-occlusal loading of implants: a randomized clinical pilot study. Clin Implant Dent Relat Res 17(3): 589-597.
- Weinstein R, Agliardi E, Fabbro MD, Romeo D, Francetti L (2012) Immediate rehabilitation of the extremely atrophic mandible with fixed full-prosthesis supported by four implants. Clin Implant Dent Relat Res 14(3): 434-441.
- Gehrke SA, da Silva Neto UT, Del Fabro M (2015) Does implant design affect implant primary stability? A Resonance Frequency Analysisbased randomized split-mouth clinical trial. J Oral Implantol 41(6): e241-246.
- Gliardi E, Clerico M, Ciancio P, Massironi D (2010) Immediate loading of full-arch fixed prostheses supported by axial and tilted implants for the treatment of edentulous atrophic mandibles. Quintessence Int 41(4): 285-293.
- Chiapasco M (2004) Early and immediate restoration and loading of implants in completely edentulous patients. Int J Oral Maxillofac Implants 19(suppl): 76-91.
- Chang M, Chronopoulos V, Mattheos N (2013) Impact of excessive occlusal load on successfully-osseointegrated dental implants: A literature review. J Investig Clin Dent 4(3): 142-150.
- J Al Sukhun, M Helenius, C Lindqvist, J Kelleway (2007) Biomechanics of the mandible part I: Measurement of mandibular functional deformation using custom-fabricated displacement transducers, Journal of Oral and Maxillofacial Surgery 64(7): 1015-1022.
- Wong N (2016) Predictable immediate implant prosthetics using guided surgery and guided prosthetics: a case report. Oral Health 106(1): 66-78.
- T Satoh, Y Maeda, Y Komiyama (2005) Biomechanical rationale for intentionally inclined implants in the posterior mandible using 3D finite element analysis. Int J Oral Maxillofac Implants 20(4): 533-539.
- Drago CJ, Lazzara RJ (2006) Immediate occlusal Loading of Osseotite implants in mandibular edentulous patients: a prospective observational report with 18-month data. J Prosthodont 15(3): 187- 194.
- Geraets W, Zhang L, Liu Y, Wismeijer D (2014) Annual bone loss and success rates of dental implants based on radiographic measurements. Dento Maxillo Fac Radiol 4397): 20140007.
- Del Fabbro M, Ceresoli V (2014) The fate of marginal bone around axial vs. tilted implants: a systematic review. Eur J Oral Implantol 7(suppl 2): S171-189.
- Al Helal A, AlBader B, Kattadiyil MT, Garbacea A, Proussaefs P (2017) CAD-CAM implant-supported fixed complete dental prosthesis with titanium milled molars: A clinical report. J Prosthet Dent 117: 463-469.






























