Maxillofacial Trauma: A Case of Diacapitular Condylar Fracture
Krishna Prasad Regmi, Jun Bo Tu*, SuMengGe, Cheng Qun Hou, Li Feng Li and Jing Ting Du
Hospital of Stomatology, Xian Jiaotong University, China
Submission: April 13, 2017; Published: November 15, 2017
*Corresponding author: JunBoTu, Hospital of Stomatology, Xian Jiaotong University, China , Tel: +861-566-708-6735; Fax:+862982655059; Email: tujunbo@xj tu.edu.cn
How to cite this article: Krishna P R, Jun B T, SuMengGe, Cheng Q H, Li F L, Jing T D. Maxillofacial Trauma: A Case of Diacapitular Condylar Fracture. Adv Dent & Oral Health. 2017; 6(1): 555680.DOI:10.19080/ADOH.2017.06.555680
Abstract
The etiology and epidemiology of pediatric trauma involving the diacapitular condylar fractures (DFs) have been reported in a large series of patients. Nevertheless, little is known about treatment protocols for DFs in children. Accordingly, the treatment modalities for the management of pediatric fractures also differ. Here we suggest following PDA and Intracapsular ABC classification of Condylar fracture during treatment planning.
Keywords: Maxillofacial trauma; Diacapitular fracture; Condylar fracture; PDA classification
Introduction
Trauma, defined as a bodily injury resulting from an external force, is the leading health problem that children and adult are facing today. Their proneness to injury and clinical features they experience varies according to their social and economic development. Maxillofacial trauma in a pediatric group of patients is particularly challenging, as these patients have significant differences from adults as far as the facial skeleton is concerned [1,2]. Mandibular condylar fractures are common presentations to hospitals across the globe and remain the most important cause of temporomandibular joint (TMJ) ankylosis [3,4]. The etiology and epidemiology of pediatric trauma involving the facial skeleton have been reported in a large series of patients. Nevertheless, few of these reports review large numbers of pediatric patients, and little is known about treatment protocols for fractures in children. Accordingly, the treatment modalities for the management of pediatric fractures also differ.
Case Presentation
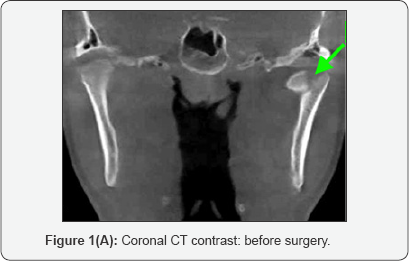
Fourteen years old male patient visited our hospital with the history of injury on his face and limited mouth opening. Patient history of the injury revealed that the victim had been accidentally fallen on the ground two days ago and got an injury on his face. There was no loss of consciousness. The initial management of soft tissue injury and pain management had been done in a local hospital. He had come to the clinic because of difficulty in chewing food due to limited mouth opening. The patient complained of pain on left anterior tragus region while on palpation. The mobility of condylar region was decreased. The mouth was deviated towards the side of injury with cross bite, premature tooth contact on left and right posterior region and open bite on the anterior region. Under Cone beam computed tomography examination visible fracture line was found to be on left lateral condylar projection with medial condylar head shifting inferomedially [5].
Diagnosis [6-9]
ABC classification: Left intracapsular condylar fracture- type A.
PDA classification: P 1 D 3 and A 2 - (type I).
Treatment method: Surgical intervention
Reason for surgical intervention:
Left intracapsular condylar fracture of type a,
Dislocation of condylar tip >5mm, >30o (lower portion of bone was still on contact)
The height of mandibular left ramus decreased.
Limited mouth opening, and
Occlusal disorders.
Treatment [7,9,10]
Operative treatment was done within one week of injury Open reduction with internal fixation was made under general anesthesia with the pre-auricular surgical approach. Two Lag screws (12 mm and 14 mm, with diameter 2 mm) were used for stabilization of reduced fractured bone.
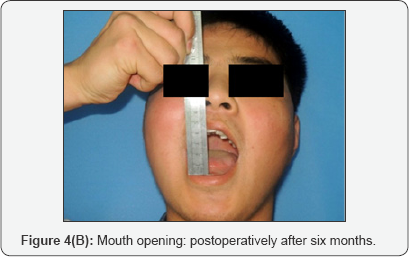
Postoperative: post-operatively slight motor dysfunction of operated side was seen. It may be related to retraction of muscle during surgical intervention. The patient was kept under the supervision of hospital care for one week. On discharge, soft diet and early mandible movement of mild degree for six months was suggested to the patient. Neurotrophic agents (cyanocobalamin) for one month were prescribed. On 6-month recall visit, the strength of stomatognathic unit was all restored to the normal condition as described by patients' subjective feelings. Mouth Opening was 40 mm. Occlusion restored stable to class one as the preoperative condition.
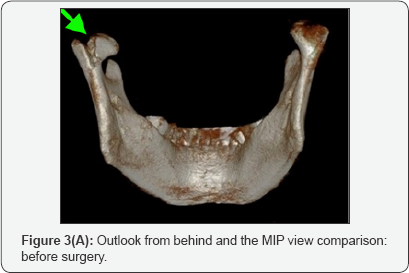
Imaging and pictures Comparison: (Figure 1-4).





Discussion
The current indications for open reduction and internal fixation ofdiacapitular fractures (DFs) described in the literature are: (a) fractures affecting the lateral condyle with reduction of mandibular height; (b) fractures in which the proximal fragment dislocates laterally out of the glenoid fossa, which cannot be reduced by closed or open treatment of another part of the mandibular fracture. The indications for conservative treatment are: (a) fractures that do not shorten the condylar height (a fracture with displacement of the medial parts of the condyle); (b) undisplaced fractures; (c) comminution of the condylar head, when the bony fragments are too small for stable fixation; and (d) fractures in children. As the temporomandibular joint disk plays an important role as a barrier preventing ankylosis, it is important to reposition the disk (if displaced/dislocated) during the surgical treatment of diacapitular fractures. The lateral pterygoid muscle should never be stripped from the medially displaced fragment because its disinsertion disrupts circulation to the medial bony fragment, and also because this muscle helps to restore the muscle function after surgery. Open reduction with internal fixation (ORIF) of selected diacapitular fractures improves prognosis by anatomical bone and soft tissue recovery when combined with physical therapy. If conducted properly, surgical treatment of DFs is a safe and predictable procedure and yields good results [11,12].
Here, we follow the PDA and intracapsular ABC classification of condylar fracture as a guide for the treatment of traumatized condyle. This classification assists the surgeons' expertise to increase the treatment efficacy. At the same time, recent advancement of surgical accessory tools will be a boon to increase the treatment accuracy of fracture reduction by helping the concerned surgeon to make the treatment with a broad concept of a comprehensive treatment protocol. Three-dimensional visualization of injured side increases the surgeons' confidence to reduce and stabilize as far possible as in a natural position.
Conclusion
We suggest following the PDA and intracapsular ABC classification of condylar fracture to increase the overall postoperative satisfaction level that bypasses the change of subjective feelings of patients' from preoperative to the postoperative condition. At the same time, use of 3-D technology and surgical navigation may also increase treatment accuracy.
Conflict of Interest Statement
We have no conflict of interest.
References
- Andrade NN, Choradia S, Sriram SG (2015) An institutional experience in the management of pediatric mandibular fractures:A study of 74 cases. J Craniomaxillofac Surg 43(7): 995-999.
- Iatrou I,Theologie Lygidakis N, Tzerbos F (2010) Surgical protocols and outcome for the treatment of maxillofacial fractures in children:9 years' experience. J Craniomaxillofacial Surgery 38(7): 511-516.
- Theologie Lygidakis N, Chatzidimitriou K, Tzerbos F, Gouzioti A, Iatrou I (2016) Nonsurgical management of condylar fractures in children: A 15-year clinical retrospective study. J Cranio- Maxillofacial Surgery 44(2): 85-93.
- Anyanechi CE (2015) Temporomandibular joint ankylosis caused by condylar fractures: a retrospective analysis of cases at an urban teaching hospital in Nigeria. Int J Oral Maxillofac Surg 44(8): 102733.
- Ludlow JB, Ivanovic M (2008) Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surgery Oral Medicine Oral Pathology Oral Radiology and Endodontology 106(1): 106-114.
- Maclennan WD (1952) Consideration of 180 cases of typical fractures of the mandibular condylar process. British Journal of Plastic Surgery 5(2): 122-128.
- Bagheri SC, Dierks EJ, Kademani D, Holmgren E, Bell RB, et al. (2006) Application of a facial injury severity scale in craniomaxillofacial trauma. J Oral Maxillofac Surg 64(3): 408-414.
- Loukota RA, Eckelt U, De Bont L, Rasse M (2005) Subclassification of fractures of the condylar process of the mandible. British Journal of Oral & Maxillofacial Surgery 43(1): 72-73.
- Hlawitschka M, Loukota R, Eckelt U (2005) Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. International Journal of Oral and Maxillofacial Surgery 34(6): 597-604.
- Eckelt U (2006) Commentary regarding the publication Fractures of the mandibular condyle - A review of 466 cases. Literature review, reflections on treatment and proposals” by N. ZACHARIADES et al. Journal of Cranio-Maxillofacial Surgery 34(7): 433-434.
- Allred LJ, Crantford JC, Reynolds MF, David LR (2015) Analysis of Pediatric Maxillofacial Fractures Requiring Operative Treatment: Characteristics, Management, and Outcomes. J Craniofac Surg 26(8): 2368-2374.
- Chrcanovic BR (2012) Open versus closed reduction: diacapitular fractures of the mandibular condyle. Oral and maxillofacial surgery 16(3): 257-265.






























