Root Amputation: A Prudent Alternative to Tooth Extraction
Jamal Aqrabawi*
Department of Dentistry, University of Jordan, Jordan
Submission: June 15, 2016;s Published: July 14, 2016
*Corresponding author: Jamal Aqrabawi DDS, DMD, DSc, Diplomate of the American Board of Endodontists, Professor of Endodontics, Faculty of Dentistry, University of Jordan, Amman, Jordan, Tel:00 962 79 55 35 600 ; Email:jamal58@go.com.jo
How to cite this article: Jamal A. Root Amputation: A Prudent Alternative to Tooth Extraction. Adv Dent & Oral Health. 2016; 2(2): 555582. DOI: 10.19080/ADOH.2016.02.555582
Abstract
Compromised teeth often pose a significant challenge to the clinician, complicating the treatment plan and compromising long term prognosis. Upper molar teeth showing periodontal attachment loss, caries or fractures involving the furcation area are prime examples of such challenges. Treatment option for affected teeth can be roughly divided into maintenance of the tooth through root resection therapy, or extraction and replacement. Root resection therapy involves removal of the diseased root along with its coronal portion while retaining the relatively healthy parts.
The indication, contra-indications and technique of root resection therapy are described in this case report of an upper molar in which combined resection, endodontic and prosthetic management resulted in a successful outcome.
Keywords: Root resection; Endodontic and prosthetic management; Oral hygiene; Mesiobuccal root amputation
Introduction
Root resection is a technique for maintaining a portion of a diseased or injured molar by removal of one or more of its roots [1]. In lower molars, root resection can be achieved by hemi sectioning the whole tooth in half and removing the diseased root along with its crown part. However, in upper molars root resection is mostly carried out by removal of the diseased root alone (root amputation) with rounding of the crown.
Root resection therapy outcome was investigated in a few studies showing a variable “success rate” or survival of resected teeth depending on the study. Langer et al. [2] showed in a randomized retrospective study that resected molars tend to have an acceptable success rate albeit non-lasting, with lower molars more frequently failing due to root fracture while uppers failed due to periodontal breakdown progression. They concluded that at least a 10 year recall should be implemented in outcome studies to get a meaningful outcome as failure tended to happen between the 5th or 7th year postoperatively. About 38% of these teeth failed during the 10 year observation period [2]. A relatively similar survival rate was reported by a different study showing 83% survival rate at 5 years dropping to 68% at 10 year recall time [3]. The authors concluded that the resection itself may remove the diseased root but may also create another nidus for new aggravating factors such as overhanging restorations [3]. On the other hand; Carnevale et al. [4] reported a survival rate about 93% over a 10 year follow up, which was corroborated by the results reported in a more recent study [5]. The disparity in the reported survival rates was attributed to the technique sensitivity, case selection, patient compliance with oral hygiene instructions and proper restorative treatment [4].
Due to this disparity in reported outcome and perceived high outcome or success rate of dental implants, the clinician is often faced by the dilemma of choice between root resection therapy and implant replacement. As one may devise, it is extremely difficult to directly compare the two treatment modalities. Unfortunately, studies comparing the two treatment modalities’ outcome are very few. In a private practice retrospective study the survival rate of 701 resected molars was compared to that of 1472 implants in molar areas after more than 15 years of function [6]. No significant difference could be demonstrated between the cumulative success rate of the two treatment modalities (root resection therapy =96.8%; implants= 97%). The highest failure rate was noted in resected molars or implants that were lone standing (terminal abutments) [6].
As a result of the lack of more evidence, the clinician is increasingly confronted by the pressure of choosing the treatment modality for managing a compromised molar with furcation involvement. Case selection for root resection therapy should take into consideration the skills and expertise of the clinician [4,7]. The indications and limitations of root resection therapy were discussed in a comprehensive literature review [8] and some guidelines were suggested in a recent review [7]. The acceptable indications of root resection therapy from an Endodontic point of view are [1,8].
- Severe vertical root fracture involving one root.
- Undermined furcation areas due to caries, or perforations.
- Perforation of one of the roots of a molar not allowing adequate access to the original root canal hindering canal disinfection procedures.
- Failure of one of the abutments within a fixed partial denture because of periodontal disease, if the remaining abutments support is adequate.
- Inability to manage endodontic obstructions or complications in one root of a molar tooth.
While root resection therapy would be contra-indicated if root separation is difficult due to fusion of the roots, in-operable endodontic complication or obstruction in the root to be retained, presence of a strong and good adjacent abutments for a bridge as an alternative [1]. Of course, should the clinician lack the expertise needed for proper surgical management and subsequent restoration, root resection should not be carried out.
In this case report, an upper molar with endodontically complicated mesiobuccal root canals was managed using root resection therapy in a keen and compliant patient.
Case report
A 54year old female reported to my office with the chief complaint of pain on the upper left quadrant. On clinical exam tooth #14(UL6) has already prepared as an abutment for 3 unit bridge, percussion test 0n #14(UL6) revealed tenderness and discomfort.
On radiographic examination, tooth 14(UL6) has a RCT with short fill and stripping of the mesiobuccal root (Figure 1). The root canal on the destobuccal root and the palatal one seems to be satisfying. Probing around tooth 14(UL6) was within normal limit.

Upon further investigation we came to conclude that the mesiobuccal root is the source of the patient pain.
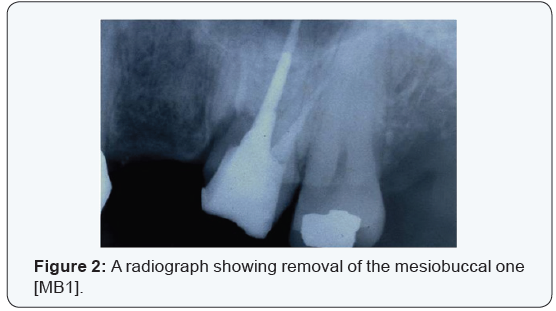
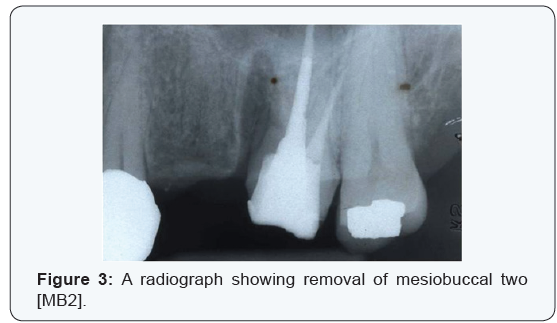
The treatment plan was presented to the patients who include removal of the whole mesiobuccal root (MB root amputation) and keeping the palatal and the destobuccal roots. Upon agreement,the treatment started by giving the patient local anesthesia. A long shank tapered fissure diamond bur was used to make vertical cut toward the furcation. A fine probe was passed through the cut to ensure separation which was confirmed on the radiograph (Figure 2). The furcation area was trimmed to ensure that no spicules were present. The mesiobuccal root was removed in 2 pieces (Figure 3).
2months later after complete healing of the socket an impression was taken and 3 unit bridge was fabricated and since then the patient has no complaint. Five years later a radiograph was taken and showed no sign of problem (Figure 4).

Discussion
The main aim of root resection therapy is to maintain a diseased tooth as an alternative to extraction and replacement. Dental implants, extensive bridgework and custom-made tooth replacement can be expensive and time-consuming. Generally, root resection and the necessary crown work are less expensive and can be completed in 1-3 short visits.
Case selection affects the outcome of root resection as a treatment of choice where endodontic complications affecting one root of multi-rooted tooth. Factors such as occlusal forces, tooth restorability, and the value of the remaining roots must be examined before treatment [9]. Success of root resection procedures depends significantly on proper case selection and definite treatment plan discussed together with the endodontist, periodontist and the restorative dentist. Unfortunately, as mentioned earlier, a restoration can contribute to periodontal destruction, if the margins are defective or if non-occlusal surfaces do not have physiologic form. Also, an improper shaped occlusal contact area may convert acceptable forces into destructive forces and predispose the tooth trauma from occlusion and ultimate failure of root amputation [10].
References
- Vijay Mantri, Rahul Maria, Sharad Kamat, Ambar W Raut (2013) Root Amputation: Case reports and review. Endodontology 25(2): 89-96.
- Langer B, Stein SD, Wagenberg B (1981) An Evaluation of Root Resections: A Ten–Year Study. J Periodontol 52(12): 719-722.
- Blomlof L, Jansson L, Appelgren R, Ehnevid H, Lindskog S (1997) Prognosis and mortality of root-resected molars. Int J Periodontics Restorative Dent 17(2): 190-201.
- Carnevale G, Pontoriero R, di Febo G (1998) Long-term effects of rootresection therapy in furcation-involved molars. A10-year longitudinal study. J Clin Periodontol 25(3): 209-214.
- Yuh DY, Cheng GL, Chien WC, Chung CH, Lin FG, et al. (2013) Factors affecting treatment decisions and outcomes of root-resected molars: a nationwide study. J Periodontol 84(11): 1528-1535.
- Fugazzotto PA (2001) A comparison of the success of root resected molars and molar position implants in function in a private practice: results of up to 15-plus years. J Periodontol 72(8): 1113-1123.
- Kasaj A (2014) Root resection procedures vs implant therapy in the management of furcation-involved molars. Quintessence Int 45(6): 521-529.
- Kinsel RP, Lamb RE, Ho D (1998) The treatment dilemma of the furcated molar: root resection versus single-tooth implant restoration. A literature review. Int J Oral Maxillofac Implants 13(3): 322-332.
- Green EN (1986) Hemisection and root amputation. J Am Dent Assoc 112(4): 511-518.
- Mehmet Dalkiz, Altug Cilingir, Bedri Beydemir (2008) Bicuspidization : A Case report OLGU SUNUMU Gulhane Med J 50(1): 42-45.






























