Guided Tissue Regeneration using an Equine Bio-absorbable Collagen Membrane with or without Equine Bone Graft in the Treatment of Intrabony Defects in Patients with Aggressive Periodontitis Results of 18 month.
*Mahmoud Helmy Belal
Damanhour University, Egypt
Submission: May 04, 2016; Published:June 24, 2016
*Corresponding author: Mahmoud Helmy Belal, Department of Oral Medicine, Periodontology, Oral Diagnosis & Radiology, Faculty of Dentistry,Damanhour University, Damanhour, Al-Gomhouria Street, Egypt, Tel: 2-010-6571-656; Email:mahmoud_672000@yahoo.com
How to cite this article: Mahmoud H B. Guided Tissue Regeneration using an Equine Bio-absorbable Collagen Membrane with or without Equine Bone Graft in the Treatment of Intrabony Defects in Patients with Aggressive Periodontitis Results of 18 month. Adv Dent & Oral Health. 2016; 2(1): 555578.DOI: 10.19080/ADOH.2016.02.555578
Abstract
Background:Successful periodontal regeneration is considered a gold standard for periodontists. Several GTR materials and bone grafts have been attempted but showed variable success rates.
Objective:The present randomized clinical and radiographic study was undertaken to compare the effectiveness of guided tissue regeneration (GTR) by using equine bioabsorbable collagen membrane with or without equine bone graft in the treatment of periodontal intrabony defects affected by aggressive periodontitis.
Materials and Methods: Ten systemically healthy patients with 20 periodontal intrabony defects were enrolled as a split mouth design. These defects were affected with aggressive periodontitis. The recorded measurements included plaque index, gingival bleeding index, gingival recession, PPD, clinical attachment level, radiographic defect depth and radiographic density. The defects were randomly distributed either as a control group (equine bioabsorbable collagen membrane alone) or a test group (equine bioabsorbable collagen membrane combined with equine bone graft).
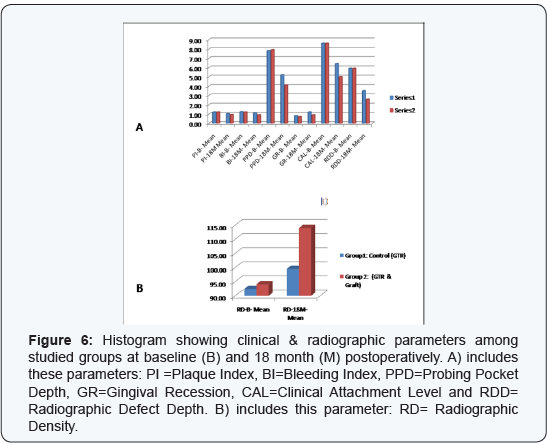
Results: The inter- & intra-group comparison showed no significant differences between studied groups nor within each group for these clinical parameters (PI, BI & GR), except only gingival recession within group 1. On contrary, the inter- & intra-group comparison showed significant differences between studied groups and within each one for these parameters (PPD, CAL, RDD & RD).
At 18-month examination, PPD reduction was significantly greater in GTR + bone graft group (3.80±1.33 mm) compared with GTR group (2.60±1.57 mm), and clinical attachment level gain were 3.60±1.15 and 2.20±1.26 respectively. Radiographic DD reduction was similarly greater in GTR + bone graft group (3.30 ± 0.84 mm) compared with GTR group (2.40±1.09 mm). Also, the change in the radiographic density indicated a significant greater gain of mean gray level as (19.90 ± 16.00) in group 2 whereas 7.10±10.65 in group 1.
Conclusion: Use of GTR bioresorbable membrane with bone graft showed significant improved outcomes when compared to use of bioresorbable membrane in treating aggressive periodontitis. However, the studied groups showed significant improvement within each group when baseline & 18 month data were compared.
Keywords: Aggressive Periodontitis; Bone Graft; Guided Tissue Regeneration; Intrabony Defect
Abbreviations: AP: Aggressive Periodontitis; GTR: Guided Tissue Regeneration; CAL: Clinical Attachment Level; PPD: Probing Pocket Depth; GR: Gingival Recession; BI: Bleeding Index; PI: Plaque Index; RD: Radiographic Density; RDD: Radiographic Defect Depth; CBR: Crestal Bone Resorption; AC: Alveolar Crest; CEJ: Cementoenamel Junction; BD: Base of the Defect
Introduction
The aim of successful periodontal therapy is a trial to arrest inflammatory process, suppress microbial growth, control infection and attempt to restore the tissues destroyed due to periodontal disease. Different regenerative techniques may be used for such purposes, but the treatment or elimination of the infection should be the most important goal especially in patients having aggressive periodontitis [1,2].
Aggressive periodontitis (AP) is characterized by severe periodontal destruction within a relatively short period of time. It has some etiologic agents capable of causing clinically detectable diseased levels that may negatively hazard oral healthy condition and alter daily life style of such patients. AP has less occurrence among periodontitis patients and few studies have evaluated some treatment protocols [3].
The predictable complete periodontal regeneration remains a major goal in the planned therapy. Despite several procedures such as usage of guided tissue regeneration (GTR), grafting materials, growth factors and/or host modulating agents have been attempted, the outcomes are not always predictable [4-6]. However, there is a great variation caused by many factors, for example; type of periodontitis, patient characteristics, anatomy of defect site and the surgical intervention [7]. The treatment of aggressive type of periodontitis has a great challenge to many clinicians.
In general, the most successful documentation of periodontal regeneration is GTR since it acts as an effective principal therapy for the treatment of different anatomic defects associated with periodontitis [5]. Some earlier animal [8,9] and human studies [10,11] indicated a predictable reconstruction of the periodontium by using either non-bioabsorbable or bioabsorbable membranes [12]. However, bioabsorbable GTR membranes were developed to avoid the second surgery needed to retrieve the non-resorbable barrier [13-16]. These bioabsorbable devices have two main products, natural (collagen membrane) and synthetic (copolymers) like Guidor, Vicryl periodontal mesh, Resolut and Atrisorb GTR barriers.
Use of GTR through the use of equine barrier and equine bone graft material showed a favorable clinical outcome and an effective periodontal therapy in the regenerative treatment of intrabony defects [17]. Also, these equine collagen membranes and equine bone acts as an effective therapy for guided bone regeneration in the treatment of bone defect consequent to removal of periapical cyst in clinical & histological report [18].
Some previous literature reports [13-16] were found, in which the efficacy of bioabsorbable membranes alone or combined with graft materials were evaluated and compared for regenerative purposes. However, to our knowledge, there are no available studies comparing the efficacy of using an equine bioabsorbable collagen barrier (Biocollagen®) alone or combined with equine graft (Bio-Gen®), in treating intrabony defects of aggressive periodontitis.
Subjects and Methods
Inclusion criteria
- Aggressive periodontitis.
- Intrabony periodontal defect sites with probing pocket depth > 5mm, as assessed by clinical and radiographic evaluation.
- Radiographic evidence of vertical/angular bone loss.
- Age ranged from 17 to 37 years.
- Good general health.
Exclusion criteria
- Periodontal treatment received during the last 6 months at least.
- Hopeless teeth or evident grade-III mobile teeth.
- Any relevant systemic diseases.
- Smokers and/or alcoholics.
- Pregnancy and/or lactation for female patients.
- Hypersensitivity to any of the tested research materials.
Study Design
Ten patients (seven males & three females) were selected to be enrolled in this study and gathered from the out-patient clinic of the Department of Oral Medicine, Periodontology, Oral Diagnosis & Radiology. Verbal and written informed consent forms were obtained from all subjects and an ethical clearance was also get from the institution.
Ten patients with bilateral intrabony periodontal defects were selected. Thus, a total of twenty affected sites were chosen as noticed primarily on the radiographs and confirmed clinically as well as within the reconstructive surgical intervention. These defects were distributed into two groups as follows:-
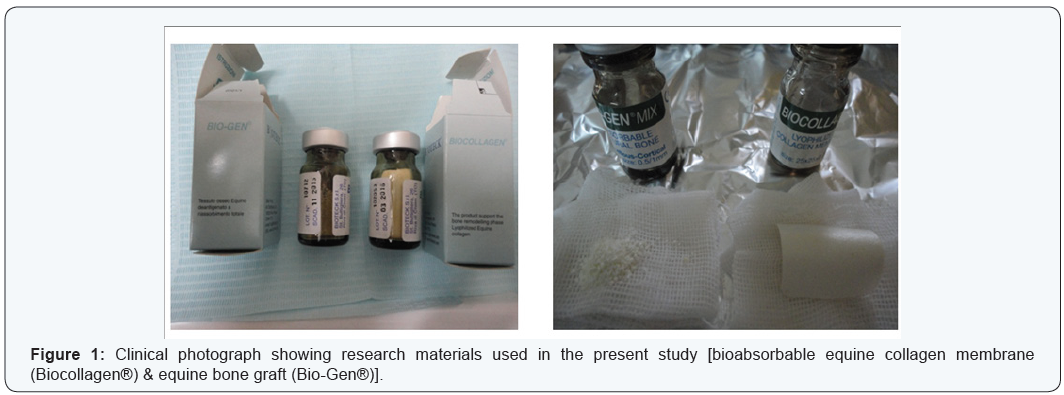
- Group 1 (the control group): Ten sites received flap debridement followed by the application of bioabsorbable equine collagen membrane* (Biocollagen®).
- Group 2 (the test group): Ten sites received flap debridement followed by the application of the same bioabsorbable collagen membrane but combined with equine bone graft material as xenograft† (Bio-Gen®).
Primary Assessment and Patient’s Preparation
Patients were subjected to pre-surgical, clinical and radiographic interpretation. The patients completed a thorough plaque control regimen and a strict oral hygiene instruction. Full-mouth phase I therapy was done using periodontal Gracey curettes# and an ultrasonic apparatus$. The reevaluation period was determined according to each individual response, with an average period of about 6 weeks. Thereafter, a treatment plan was defined and an additional non-surgical therapy and/or dental extractions were done whenever needed. However, the surgical intervention were started when the subject’s plaque and gingival index had achieved at least 20% levels, according to instructions of some previous reports [19-21].
Clinical Measurements
Plaque index (PI), gingival bleeding index (BI), gingival recession (GR); probing pocket depth (PPD) and clinical attachment level (CAL) were recorded. An acrylic stent with reference points was used to localize the measurement sites at baseline and 18 months postoperatively. The periodontal measurements were recorded using a graduated William’s periodontal probe‡. Tooth mobility was also graded [22], scored and evaluated.
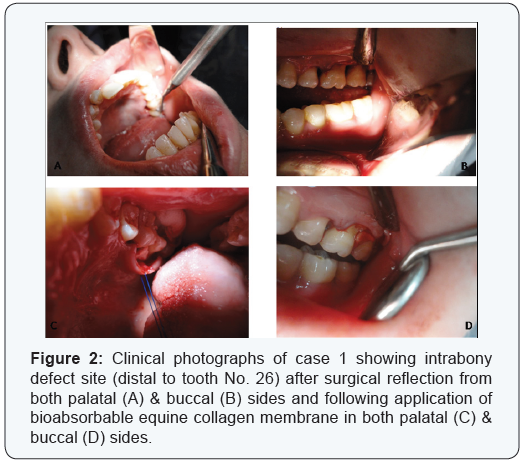
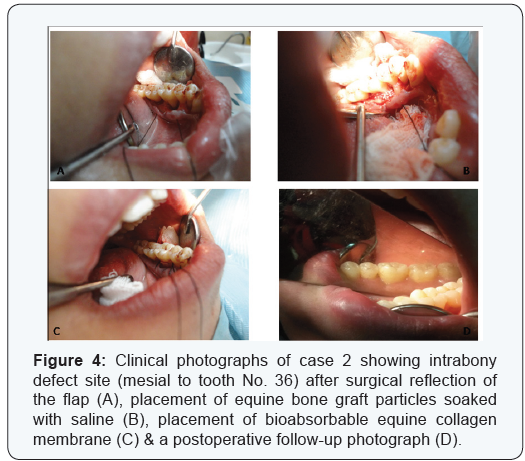
Surgical Procedures
Access to the defects were done using full-thickness flaps and sulcular incisions through the bottom of the crevice, extending mesial and distal to the adjacent teeth and including the flap papillae. No releasing incisions needed on either sides of the flap. Granulomatous tissues were curetted and thorough root planning was performed. EDTA with a concentration of 24%, at neutral pH, was used then washed with saline irrigation.
Randomly, using a coin, one defect treated with equine bioabsorbable collagen membrane as a control group whereas the other defect was treated with the same collagen membrane but combined with equine bone graft (the test group). Graft material was soaked with sterile saline and condensed gently in the defects to the adjacent crestal walls. The collagen membrane was adapted to obtain precise application to the interproximal area of the affected site. The membrane was then adjusted to completely cover the defect, overlapping at least 2-3 mm of the residual bone and sutured adequately with bioabsorbable sutures. Flaps were repositioned coronally during wound suturing, if required. The surgical site was covered with a noneugenol periodontal dressing% on the buccal and lingual aspects.
Post Operative Care
Chlorhexidine digluconate mouth rinse (0.12%) was used as two times daily for one month postoperatively. Amoxicillin trihydrate 875 mg/clavulanic acid as potassium salt 125 mg (Hibiotic 1gm film coated tablets, Amoun Pharmaceutical Co. SAE., El-Obour city, Cairo, Egypt), was prescribed as two times daily for 10 days. Also, a non-steroidal anti-inflammatory drug (Ibuprofen 600 mg, “Brufen granules”, effervescent sachets, Kahira Pharm. & Chem. Ind. Co. under license of Abbott Laboratories-USA) was also prescribed twice per day, for 7 days. In addition, antiprotozoal drug (Secnidazole 1gm, Nitroimidazole derivative, Cipazole forte, SIGMA Pharmaceutical Industries-Egypt, with cooperation of Queen Pharm international) was prescribed two tablets (each tablet contains Secnidazole 1gm) as a single dose (one day treatment) during meal.
Postoperative care was performed weekly in the first month, monthly up to six months and then every 3 months. In cases of membrane exposure, Doxycycline 100 mg was prescribed 2 times per one day then once for 5-7 days, and the surgical sites were carefully cleaned with a cotton swab soaked with 0.12% chlorhexidine digluconate two times daily.
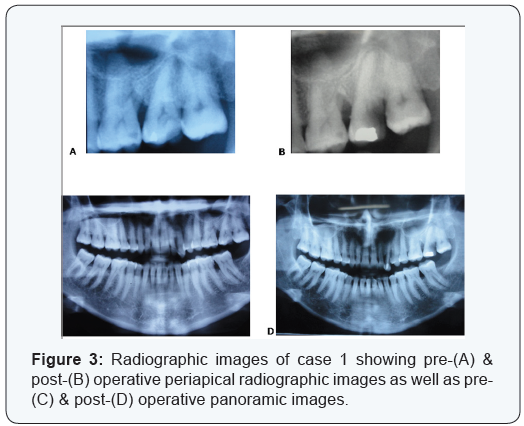
Assessment of radiographic parameters and radiographic interpretation
Standardized intra-oral periapical radiographs (Kodak X-ray film, USA) were obtained at baseline and 18 months postoperatively. These radiographs were taken using long cone/ extension cone paralleling technique with a positioning device mounted on a roentgen machine, operating at 70 Kilo Voltage Power.
Radiographs were scanned using a digital scanner at an input of 300 dpi and 100% scale, then they were analyzed using a software@. The images had 768 × 512 pixels and 256 gray scale level. The alignment of images, in the pairs of radiographs, was applied to correct small geometric misalignments. Gray level was then calibrated to indicate changes in the radiographic density (RD).
In addition, the following measurements were obtained in millimeters: distance from cementoenamel junction (CEJ) to base of the defect (BD) and from CEJ to alveolar crest (AC). The differences between baseline and 18-month postoperative values for CEJ–BD indicated the change in the radiographic defect depth (RDD), whereas the differences for CEJ–AC suggested the possible occurrence of crestal bone resorption (CBR).
Statistical Analysis
The present study had parametric variables. Thus, student’s paired t-test was used to compare the changes in the data from baseline up to 18 months postoperatively within each treatment group. On the other hand, the intergroup comparison was accomplished by independent sample t-test. A ‘P’ value of 0.05 or less was considered statistically significant.
Results
Using student’s paired t-test, the intra-group comparison showed comparable outcomes in the experimental groups regarding plaque index, gingival bleeding index as well as gingival recession, when comparing baseline scores to 18 months postoperative data. This is because there were no statistically significant differences noticed for these parameters, except only gingival recession within group 1 where P value recorded as 0.04. In addition, using independent sample t-test for intergroup comparison there were no statistically significant differences found between the two groups for these clinical parameters (PI, BI & GR). (Table 1).
On the other hand, by using student’s paired t-test, statistically significant differences were found when comparison was done from baseline up to 18 month postoperatively within both groups (1 & 2) regarding PPD, CAL, RDD & RD. Furthermore, using independent sample t-test for intergroup comparison there were also statistically significant differences found between the two groups for these clinical and radiographic parameters (PPD,CAL, RDD & RD) (Table 1).

The probing depth is reduced from (7.80±1.75 mm) at baseline to (5.20±1.40 mm) at 18 month with a mean difference of (2.60±1.57 mm) in group 1, whereas from (7.90±1.66 mm) to (4.10±.99 mm) with a mean difference of (3.80±1.33 mm) in group 2. This was statistically significant (P = 0.000). The intergroup comparison indicated that the difference was statistically significant with a P value of 0.05 (Table 1).
The clinical attachment level is changed from (8.60±1.26 mm) at baseline to (6.40±1.26 mm) at 18 month postoperative with a mean CAL gain of (2.20±1.26 mm) in group 1, whereas from (8.60±1.35 mm) to (5.00±.94 mm) with a mean CAL gain of (3.60±1.15 mm) in group 2. This was statistically significant (P = 0.000). The intergroup comparison indicated that the difference was statistically significant with a P value of 0.01 (Table 1).
The radiographic defect depth was reduced from (5.90±1.10 mm) at baseline to (3.50±1.08 mm) at 18 month postoperative with a mean difference of (2.40±1.09 mm) in group 1, whereas from (5.90±.99 mm) to (2.60±.70 mm) with a mean difference of (3.30±0.84 mm) in group 2. This was statistically significant (P = 0.000).
The radiographic density was changed from (92.40±12.38) at baseline to (99.50±10.91) at 18 month postoperative with a mean difference of (7.10±10.65) in group 1, whereas from (94.10±14.32) to (114±17.68) with a mean gain of (19.90±16.00) in group 2. This was statistically significant (P = 0.000 & 0.03 respectively). In addition, the intergroup comparison regarding both RDD and RD showed that the difference between the studied groups was statistically significant with a P value of 0.04 (Table 1).
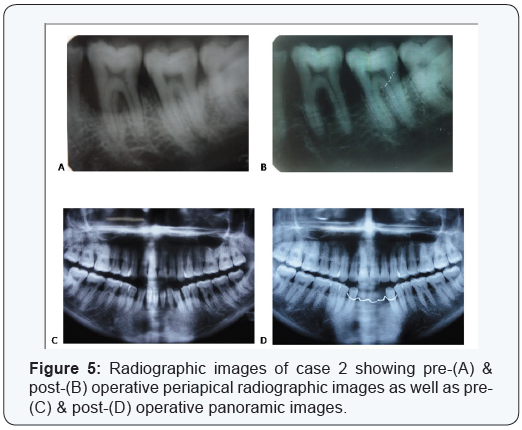
Two cases are presented in figures from 2 to 5 with clinical photographs during surgical intervention and pre-& postoperative radiographic images. Case 1 is presented in figures ( 1 & 3) and was treated by using bio absorbable equine collagen membrane, for covering and treatment of selected intrabony defect site between teeth No. 26 & 27 as mainly distal to tooth No. 26. Case 2 is presented in ( figures 4 & 5 ) and was treated by the application of the same bio absorbable collagen membrane but in combination with equine bone as xenograft material, for covering and treatment of selected intrabony defect site between teeth No. 35 & 36 as mainly mesial to tooth No. 36.
Discussion
It has been established in the previous literature [10,23] that the exclusion of epithelial and gingival connective tissue cells by using GTR barriers is important for periodontal wound healing, in order to achieve regeneration of the attachment apparatus. However, the non-restorable barriers have some disadvantages, such as higher cost, membrane exposure, need of a second intervention for their retrieval, complexity and bacterial accumulation [24,25]. Several restorable barriers are therefore developed to decrease such drawbacks. These are preferable and widely used for guided tissue and/or bone regeneration [26,27].
Collagen membranes are selected frequently as restorable barriers, especially they possess some advantageous properties. These are a low toxicity due to a low immune response, the ability of collagen to reconstitute into the natural tissues and to enhance cell growth and attachment [28,29]. In addition, collagen membranes are absorbed quickly to provide the needed integrity during regenerative process.
Bone grafts are used to treat different types of alveolar bone defects. They have a function to act with osteoconductive or osteoinductive properties. They can maintain a space and play an evident role by preventing membrane from collapse in the bone defect [30,31]. They can also support the flap, facilitate the wound stability process and enhance the regenerative procedure [32]. Equine bone graft showed a favorable clinical and histological outcomes and an effective therapy for periodontal guided tissue and bone regeneration of intrabony defects, especially when combined with equine resorbable membranes [17,18].
Regeneration of aggressive periodontal defects is considered as a real challenge. Some earlier studies [33-36,13] used different graft materials and barrier membranes, either alone or in combination, to achieve periodontal regeneration. However, the treatment outcome showed the combination therapy (GTR membrane + bone graft) as more effective than using GTR membrane or graft alone. Most of these studies showed a combination of GTR membrane with either allograft (DFDBA), xenograft (Bio-Oss), hydroxyapatite, or enamel matrix proteins. However, in recent years, some evidence [17,18] suggested that equine bone graft and equine membrane are also capable of supporting the periodontal regenerative healing capacity. The present study was therefore planned to evaluate and compare the efficacy of using equine bio absorbable barrier, either alone or combined with equine graft, in treating intrabony defects of aggressive periodontitis.
It has been noticed that the clinical measurements have a critical role in evaluating regenerative process since they can provide reliable information regarding probing depth reduction and clinical attachment level gain. The studied groups of the present study showed significant improvement of PPD & CAL parameters when comparing baseline with 18 month post-operative data (Table 1) & (Figure 6), thus signifying the regenerative role of GTR materials. In this context, Garrett in (1996) [37] stated that use of GTR membrane enhanced successfully re-growth of the destroyed periodontium; however, there are some variations in the clinical predictability, degree of efficacy, and even the histological outcomes as postulated by Bartold et al. [38]. In addition, the intergroup comparison showed more probing depth reduction and greater attachment level gain in group 2 (the combined therapy) over group 1 (GTR alone) (Table 1) & (Figure 6), since statistically significant differences were found at 18 months post-operatively. This means that the attachment gain complied with the findings obtained in the previous studies [33-36,12-14]. However, there was a statistically significant difference found within group 1 when comparing gingival recession parameter from baseline up to 18 month denoting some gingival recession increase occurred in this group, whereas no significant difference noticed within group 2. On the other hand, the comparison between the two groups did not notice significant difference for gingival recession (Table 1). In addition, the membrane exposure was occurred in only one defect site per each group, but controlled with a careful post-operative care without complication.
The radiographic analysis is one of the valid methods to demonstrate the effectiveness of regenerative therapies, since it plays a certain role in determining treatment outcome through offering a non-invasive method of evaluating the hard tissue response to therapy. The radiographic analysis of the present study included linear measurements and bone density assessment using gray level. The results showed significant defect resolutions through an evident improvement in defect depth as well as a gain in bone density in both studied groups, when comparing baseline data with results of 18 month. Also, the intergroup comparison showed statistically significant differences favoring the results of the combined therapy (GTR + graft) over using GTR alone (Table 1) & (Figure 6). On the other hand, the changes in alveolar crest height were comparable in both groups. These results are consistent with the obtained findings of some previous reports [34-36,13-16,39].
The significant improvement of the combined therapy in the present study may be explained by the use of bone graft as defect filler. In this context, some studies [14,40] suggested that treatment of periodontal intrabony defects with graft materials lead to significantly greater gain in clinical attachment level and better defect fill, by promoting osteogenesis and allowing rapid and quick formation of new bone. Also, it appears that the graft material has a critical role in preventing collapse of the membrane and/or flap during initial healing periods, thus can potentiate regeneration [32].
Regarding the positive findings obtained in the present study and as a significant point of view, it has been noticed that the ten involved cases were selected carefully with a complete patient desire to treat the affected defects, to strictly follow instructions to maintain oral hygiene and to attend needed follow up visits in due times with almost a complete compliance. The subjects had comparable bilateral intrabony defects. Their ages were below thirty in seven subjects and above thirty in only three patients. Mobility did not has any worsening in their grades throughout the whole study interval. Regarding pocket depth reduction, the number of defects that showed a successful resolution were four in Group 1 (GTR alone) and seven in group 2 (combined therapy), whereas the remaining defects (six in group 1 and three in group 2) still had a severe probing periodontal pocket depths. These remaining defects ranged in their depths from 5 to 8 mm in group 1 but from 5 to 6 mm in group 2. Regarding radiographic defect depth resolution and radiographic density gain, group 2 showed favored significant results, but no defects showed complete fill radiographically.
Conclusion
In final conclusion, although the present split-mouth clinical study had some given constraints, the combined therapy of using graft material (equine bone, Bio-Gen®) with GTR bio absorbable membrane (equine collagen, Biocollagen®) showed enhanced and significant clinical outcomes (PPD & CAL) over using GTR alone. Also, the radiographic assessment that evaluated defect fill (RDD) and bone density (RD) showed significantly greater results of the combined therapy. However, the studied groups showed significant improvement of these parameters when comparing baseline data with results of 18 month postoperatively within each group.
Meanwhile, we are planning to make further future long-term follow up (3 & 5 years) of results of the present study. However, further studies with larger sample size and different evaluation methods such as histological assessment may be recommended.
Acknowledgement
The author would like to thank Mss. Afaf El-Ewaidy for her helpful assistance during the preparation of this manuscript. The author would also like to forward sincere regards & gratefulness for the kind great efforts that is done in the radiographic analysis needed for this research by Dr. Hisashi Watanabe, Associate Professor, Section of Periodontology, Department of Hard Tissue Engineering, Graduate School, Tokyo Medical and Dental University, Tokyo, Japan.
Foot Notes
- *Biocollagen®, the product support bone remodelling phase, Lyophilized Equine bioabsorbable collagen membrane, 25 x 25 x 0.2 mm, Bioteck, Torino, Italy.
- †Bio-Gen®, bone tissue of animal Equine origin “xenograft”, deantigenized for total reabsorption, Bio-Gen Mix, Cortical-Spongy, GR. 0.5 size 0.5 – 1 mm, Bioteck, Torino, Italy.
- #Hu-Friedy, Chicago, IL, USA.
- $Cavitron, Dentsply, NY, USA.
- ‡Florida probe, Florida Probe Corporation, Gaineswille, FL, USA.
- %Coe-pak, GC America.
- @Emago Dental Software, Oral Diagnostics Dental Systems, Amsterdam, The Netherlands.
References
- Joly JC, Palioto DB, de Lima AF, Mota LF, Caffesse R (2002) Clinical and radiographic evaluation of periodontal intrabony defects treated with guided tissue regeneration. A pilot study. J Periodontol 73(4): 353-359.
- Zucchelli G, Bernardi F, Montebugnoli L, De SM (2002) Enamel matrix proteins and guided tissue regeneration with titanium-reinforced expanded polytetrafluoroethylene membranes in the treatment of infrabony defects: a comparative controlled clinical trial. J Periodontol 73(1): 3-12.
- int. Rapp GE, Pineda Trujillo N, McQuillin A, Tonetti M (2010) Genetic power of a Brazilian three-generation family with generalized aggressive periodontitis. Braz Dent J 21:137-141.
- Murphy KG, Gunsolley JC (2003) Guided tissue regeneration for the treatment of periodontal intrabony and furcation defects. A systematic review. Ann Periodontol 8(1): 266-302.
- Wang HL, Cooke J (2005) Periodontal regeneration techniques for treatment of periodontal diseases. Dent Clin North Am 49(3): 637-659.
- Bottino MC, Thomas V, Schmidt G, Vohra YK, Chu TM, et al. (2012) Recent advances in the development of GTR/GBR membranes for periodontal regeneration – a materials perspective. Dent Mater 28(7): 703-721.
- Ribeiro FV, Nociti FH, Sallum EA, Sallum AW, Casati MZ (2010) Use of enamel matrix protein derivative with minimally invasive surgical approach in intra-bony periodontal defects: clinical and patientcentered outcomes. Braz Dent J 21(1): 60-67.
- Nyman S, Gottlow J, Karring T, Lindhe J (1982) The regeneration potential of the periodontal ligament. An experimental studies in monkeys. J Clin Periodontol 9(3): 257-265.
- Aukhil I, Pettersson E, Suggs C (1986) Guided tissue regeneration. An experimental procedure in beagle dogs. J Periodontol 57(12): 727-734.
- Nyman S, Lindhe J, Karring T, Rylander H (1982) New attachment following surgical treatment of human periodontal disease. J Clin Periodontol 9(4): 290-296.
- Gottlow J, Nyman S, Lindhe J, Karring T, Wennstrom J (1986) New attachment in human periodontium by guided tissue regeneration. J Clin Periodontol 13(6): 604-616.
- Nygaard ostby P, Bakke V, Nesdal O, Susin C, Wikesjo UM (2010) Periodontal healing following reconstructive surgery effect of guided tissue regeneration using a bioresorbable barrier device when combined with autogenous bone grafting: A randomized controlled trial. 10 year follow-up. J Clin Periodontol 37(4): 366-373.
- Becker W, Becker BE, Mellonig J, Caffesse RG, Warrer K, et al. (1996) A prospective multi-center study evaluating periodontal regeneration for Class II furcation invasions and intrabony defects after treatment with a bioabsorbable barrier membrane: 1 year results. J Periodontol 67(7): 641-649.
- Mengel R, Soffner M, Flores de Jacoby L (2003) Bioabsorbable membrane and bioactive glass in the treatment of intrabony defects in patients with generalized aggressive periodontitis – Results of a 12 month clinical and radiological study. J Periodontol 74(6): 899-908.
- Gaffaney TE (2004) Guided tissue regeneration using a bioabsorbable membrane: A 21 – case series. J Periodontol 75(12): 1728-1733.
- Pretzl B, Kim TS, Steinbrenner H, Dorfer C, Himmer K, et al. (2009) Guided tissue regeneration with bioabsorbable barriers. III 10 years results in infrabony defects. J Clin Periodontol 36(4): 349-356.
- Dogan GE, Demir T, Orbak R (2014) Effect of low-level laser on guided tissue regeneration performed with equine bone and membrane in the treatment of intrabony defects: a clinical study. Photomed Laser Surg 32(4): 226-231.
- Di Stefano DA, Andreasi Bassi M, Cinci L, Pieri L, Ammirabile G (2012) Treatment of a bone defect consequent to the removal of a periapical cyst with equine bone and equine membranes: clinical and histological outcome. Minerva Stomatol 61(11-12): 477-490.
- Loe H & Silness J (1963) Periodontal disease in pregnancy (I) prevalence and severity. Acta Odontol Scand 21: 533-551.
- Loe H (1967) The gingival index, the plaque index and the retention index systems. J Periodontol 38(6) Suppl: 610-616.
- O Leary TJ, Drake RB, Naylor JE (1972) The plaque control record. J Periodontol 43(1): 38.
- Lindhe J (1983) Reattachment-new attachment. Text book of Clin Periodontol (2nd edn) Munksgaard, Copenhagen, Europe pp. 410.
- Stahl SS, Froum S, Tarnow D (1990) Human histologic responses to guided tissue regenerative techniques in intrabony lesions. Case reports on 9 sites. J Clin Periodontol 17(3): 191-198.
- Cortellini P, Pini Prato G, Tonetti MS (1996) Periodontal regeneration of human intrabony defects with bioresorbable membranes. A controlled clinical trial. J Periodontol 67(3): 217-23.
- Wang HL, Yuan K, Burgett F, Shyr Y, Syed S (1994) Adherence of oral microorganisms to guided tissue membranes: an in vitro study. J Periodontol 65(3): 211-215.
- Black BS, Gher ME, Sandifer JB, Fucini SE, Richardson AC (1994) Comparative study of collagen and expanded polytetrafluoroethylene membranes in the treatment of human class II furcation defects. J Periodontol 65(6): 598-604.
- Robert PM, Frank RM (1994) Periodontal guided tissue regeneration with a new resorbable polylactic acid membrane. J Periodontol 65(5): 414-422.
- Chvapil M, Viidik A, Vuust J (1980) Biology of collagen. Academic Press, London, UK, pp. 313-325.
- Rao KP, Joseph T, Collagen (1988) Biotechnology. (Volume III). Nimni MEBoca Raton, CRC Press Inc., Florida, USA, pp. 63-86.
- Moghaddas H, Ghasemi N (1997) Efficacy of connective tissue graft as a membrane with and without hydroxyapatite in treatment of vertical bony defects. Beheshti Univ Dent J 17: 60-68.
- Carranza F, Newman M, Takei, HH, Klokkevold (2006) PR Carranza’s Clinical Periodontology (11th edn) Saunders Elsevier, St. Louis, USA, p. 28,67: 452-466; 968-991.
- Tatakis DN, Promsudthi A, Wikesjo UM (1999) Devices for periodontal regeneration. Periodontol 2000 19: 59-73.
- Caffesse RG, Mota LF, Quinones CR, Morrison EC (1997) Clinical comparison of resorbable and non-resorbable barriers for guided periodontal tissue regeneration. J Clin Periodontol 24(10): 747-752.
- Christgau M, Schmalz G, Rreich E, Wenzel A (1998) Clinical and radiographic split–mouth study on resorbable versus non-resorbable GTR membranes. J Clin Periodontol 22(4): 306-315.
- Teparaat T, Solt CW, Clamen LJ, Beck FM (1998) Clinical comparison of bioabsorbable barriers with non-resorbable barriers in guided tissue regeneration in the treatment of human intrabony defects. J Periodontol 69(6): 632-641.
- Pretzl B, Kim TS, Holle R, Eickholz P (2008) Long term results of guided tissue regeneration therapy with non-resorbable and bioabsorbable barriers I.V. A case series of infrabony defects after 10 years. J Periodontol 79(8): 1491-1499.
- Garrett S (1996) Periodontal regeneration around natural teeth. Ann Periodontol 1(1): 621-666.
- Bartold PM, McCulloch CA, Narayanan AS, Pitaru S (2000) Tissue engineering: A new paradigm for periodontal regeneration based on molecular and cell biology. Periodontol 2000 24: 253-269.
- Trejo PM, Weltman R, Caffesse RG (1998) Effects of expanded polytetrafluoroethylene and polylactic acid barriers on healthy sites. J Periodontol 69(1): 14-18.
- Aichelmann-Reidy ME, Yukna RA (1998) Bone replacement grafts. The bone substitutes. Dent Clin North Am 42(3): 491-503.






























