Background
Rotator cuff injuries (RCIs) are among the most frequent causes of shoulder pain and functional limitations, often leading to considerable physical and emotional burden. These injuries can range from partial-thickness tears (PTTs) to full-thickness tears (FTTs), which differ in their degree of tendon damage and the associated clinical symptoms [1]. Understanding the nature of these tears is critical for devising appropriate treatment strategies. Studies have shown that supraspinatus tendon tears are the most common, often linked with age-related degeneration and repetitive overhead activities [2]. Accurate differentiation between PTTs and FTTs remains a significant diagnostic challenge, as their clinical presentations often overlap, requiring advanced imaging modalities for precise evaluation [3]. Magnetic resonance imaging (MRI) is a cornerstone in diagnosing RCIs due to its ability to provide high-resolution, non-invasive imaging of soft tissues, including tendons, muscles, and surrounding structures. MRI has demonstrated superior sensitivity and specificity in detecting FTTs compared to PTTs, with sensitivity exceeding 90% for FTTs [4]. However, the diagnostic performance for PTTs is less robust, with sensitivity levels ranging between 80-85%, attributed to the subtle signal changes seen in partial tears [5,6]. Furthermore, innovations in MRI protocols, such as 3.0T scanners and advanced sequences like T2-weighted imaging, have enhanced the modality’s ability to detect subtle tendon changes [7].
In addition to standard MRI, quantitative imaging techniques like Synthetic MRI (SyMRI) and IDEAL-IQ have emerged, offering detailed assessments of RCIs. These modalities enable the evaluation of parameters such as fat fraction (FF) and relaxation times (T1 and T2), which provide insights into the chronicity and severity of the tears. For instance, studies have highlighted significant correlations between increased FF in the supraspinatus muscle and higher grades of RCIs, demonstrating the potential of these tools in characterizing tear severity and guiding tailored treatment plans [7]. Moreover, advancements in technology have introduced deep learning models and compressed sensing MRI (CS-MRI), revolutionizing the diagnostic landscape of RCIs. Deep learning-based methods have shown diagnostic accuracy comparable to expert radiologists, particularly in identifying FTTs, while reducing the time and effort associated with manual interpretation [8,9]. Simultaneously, CS-MRI has emerged as a promising technique, providing high-quality imaging with reduced scan times, making it a viable option in clinical settings with high patient volumes [3]. These innovations underscore the evolving capabilities of imaging technologies in managing RCIs [2,9].
Despite the advantages of MRI, limitations persist, particularly in its sensitivity to partial tears and its reliance on operator expertise for accurate interpretation. Studies have emphasized that integrating MRI findings with clinical assessments enhances diagnostic precision and ensures comprehensive patient management [1,10]. This integrative approach is especially valuable in cases where imaging findings are equivocal or when the clinical impact of the injury needs further elucidation [1,3]. Another critical factor influencing RCI diagnosis is the comparison of MRI findings with surgical results, which are often considered the gold standard. Research has consistently shown that MRI excels in identifying FTTs, with sensitivities and specificities nearing 95-100% [4,5]. However, its performance in detecting PTTs is more variable, highlighting the need for cautious interpretation of MRI findings in this context [11]. Furthermore, the combination of MRI with arthroscopic evaluation has proven effective in cases where clinical and imaging findings do not align, ensuring accurate diagnosis and optimal treatment planning [10].
The introduction of artificial intelligence (AI) in RCI diagnostics has further expanded the potential applications of imaging. AIpowered algorithms, particularly those based on deep learning, can analyze large datasets of shoulder MRIs to identify patterns and anomalies indicative of RCIs. These models have achieved diagnostic accuracy levels similar to those of expert radiologists, emphasizing their potential role in augmenting clinical decisionmaking [9]. Additionally, the integration of AI with traditional imaging modalities can enhance the efficiency and accuracy of RCI evaluation, providing valuable insights into the characteristics and progression of tears [8]. As RCI management continues to evolve, the role of imaging in assessing tear morphology, chronicity, and associated structural changes becomes increasingly critical. Parameters such as the acromiohumeral distance and acromion morphology have been linked to the likelihood of tendon tears, particularly in cases involving degenerative changes [2]. These anatomical and biomechanical factors further emphasize the importance of comprehensive imaging evaluations in understanding the etiology and progression of RCIs [4,5,12].
The evolution of imaging technologies continues to refine the assessment of rotator cuff injuries (RCIs), addressing the limitations of traditional MRI. Advanced techniques such as SyMRI and IDEAL-IQ enhance the quantitative evaluation of soft tissue, offering detailed insights into parameters like fat fraction and relaxation times. These innovations enable clinicians to differentiate between acute and chronic injuries more effectively, providing crucial information for tailoring individualized treatment plans [4]. Furthermore, CS-MRI has emerged as a valuable alternative, reducing scan time while maintaining high diagnostic accuracy. This technique is particularly beneficial in clinical settings with a high patient load, ensuring rapid and reliable diagnosis without compromising image quality [3]. Artificial intelligence (AI) further amplifies the potential of imaging, allowing for the automated analysis of complex datasets and enhancing the precision of rotator cuff tear detection. AIdriven systems can highlight subtle patterns within imaging data, bridging gaps in human interpretation and streamlining diagnostic workflows [9].
The current research builds on the premise that surgical findings represent the gold standard for diagnosing rotator cuff injuries (RCIs), providing a direct and reliable method for evaluating the extent and type of tears. However, due to the invasive nature of surgery, MRI has become a cornerstone in initial evaluations. This study aims to analyze the diagnostic reliability of MRI by comparing its findings to those obtained through surgical interventions. Emphasizing surgical results as the gold standard is critical, as they offer a definitive assessment of tendon integrity, tear morphology, and associated pathologies [2,5]. While MRI exhibits high sensitivity and specificity for full-thickness tears, its performance in identifying partial-thickness tears remains variable, often necessitating corroboration through arthroscopy or open surgery [6]. By quantifying the concordance between MRI and surgical findings, this research seeks to determine the true diagnostic value of MRI and identify potential areas for improvement. Understanding these nuances will provide clinicians with actionable insights, ensuring the use of optimal diagnostic strategies and facilitating superior patient outcomes [10].
Methodology
A retrospective cohort study was conducted at EMMS Nazareth Hospital, focusing on patients who underwent rotator cuff tear repair surgery between 2020 and 2023. This study aimed to evaluate the diagnostic reliability of MRI compared to surgical findings, which served as the gold standard.
Study Population
The study included patients who:
i. Had undergone MRI due to suspected rotator cuff tears.
ii. Subsequently underwent rotator cuff repair surgery.
iii. Patients with prior shoulder surgeries, incomplete
records, or those who did not proceed to surgery after MRI
were excluded. The final sample comprised 100 patients, with a
mean age of 54.7 years (SD = 9.58, range: 22–75 years), balanced
between 51 males and 49 females.
Methods
A retrospective cohort study was conducted at EMMS Nazareth Hospital, focusing on patients who underwent MRI and subsequent rotator cuff repair surgery between January 2020 and December 2023. The study aimed to evaluate the diagnostic reliability of MRI in comparison to surgical findings, considered the gold standard for diagnosing rotator cuff injuries.
Inclusion Criteria:
Patients were included if they:
1. Had undergone an MRI scan due to clinical suspicion of
a rotator cuff tear.
2. Underwent arthroscopic or open rotator cuff repair
surgery within three months of the MRI.
3. Had complete medical records and imaging data
available for analysis.
Exclusion Criteria:
Patients were excluded if they:
1. Had a history of prior shoulder surgery or interventions
that could affect the MRI or surgical findings.
2. Presented with traumatic injuries unrelated to rotator
cuff pathology.
3. Had incomplete clinical, imaging, or surgical records.
4. Declined consent to use their medical data for research
purposes.
Procedure
MRI scans were performed using a 1.5T or 3.0T scanner, employing T2-weighted and fat-suppressed sequences to assess tendon integrity. Radiologists with at least five years of experience interpreted the images independently. Surgical findings, recorded during arthroscopic or open procedures, were documented by the attending surgeons. The presence and type of rotator cuff tears (partial or full-thickness) were compared between MRI results and surgical observations. Data were analyzed to calculate sensitivity, specificity, accuracy, and other performance metrics. This structured methodology ensures a robust comparison between MRI and surgical findings, providing valuable insights into the diagnostic reliability of MRI in clinical practice.
Data Collection
Patient data were retrieved from hospital records, including:
1. MRI reports, interpreted by certified radiologists.
2. Surgical findings, documented during arthroscopic or
open rotator cuff repair procedures.
3. Demographic data, such as age, sex, and relevant medical
history.
4. The focus was to compare the presence or absence of
rotator cuff tears in MRI and surgical findings, emphasizing both
full-thickness (FTT) and partial-thickness tears (PTT).
Performance Metrics and Statistical Analysis Performance Metrics and Statistical Analysis:
The diagnostic performance of MRI was evaluated using key metrics, including sensitivity, specificity, and accuracy. Sensitivity measured the proportion of true positives (TP) identified by MRI compared to surgical findings, while specificity assessed the proportion of true negatives (TN) where MRI accurately confirmed the absence of tears. Accuracy represented the overall agreement between MRI results and surgical findings. False positives (FP) and false negatives (FN) were recorded to identify discrepancies. A contingency table was constructed to compare MRI findings with surgical outcomes, and a Chi-square test was performed to assess the statistical significance of the relationship between the two diagnostic methods.
Ethical Considerations
The study received approval from the EMMS Nazareth Hospital ethics committee. Data collection adhered to strict confidentiality and ethical standards, ensuring compliance with international research guidelines.
Results
The study included a total of 100 patients who underwent MRI and subsequent rotator cuff repair surgery. The mean age of the participants was 54.7 years (SD = 9.58), with an age range spanning from 22 to 75 years. The interquartile range (IQR) indicates that 50% of the participants were between 49 and 63 years old, with the median age being 55 years. The sample demonstrated a balanced gender distribution, comprising 51 males and 49 females, ensuring a representative analysis across sexes. These statistics provide a demographic overview of the study population, crucial for understanding the study’s clinical relevance and generalizability. Furthermore, 91 cases where both MRI and surgery detected a tear are classified as true positives (TP). Additionally, 3 cases where MRI indicated a tear, but surgery found no evidence of one, are classified as false positives (FP). 4 cases where MRI did not detect a tear, but surgery confirmed its presence, are classified as false negatives (FN). Lastly, 2 cases where both MRI and surgery agreed on the absence of a tear are classified as true negatives (TN). This analysis highlights MRI’s strong sensitivity and accuracy in detecting rotator cuff tears while acknowledging some limitations in identifying true negative and false negative cases.
Moreover, these metrics establish MRI as a robust and reliable diagnostic tool for identifying rotator cuff injuries, with impressive accuracy in most cases, reflecting its ability to diagnose such injuries compared to surgery, which is considered the gold standard. Sensitivity measures the MRI’s ability to correctly identify tears when they actually exist. In this sample, sensitivity is 95.79%, indicating that MRI successfully identified almost all cases where surgery confirmed a tear. This high sensitivity underscores the MRI’s effectiveness in detecting rotator cuff injuries. Accuracy reflects the overall agreement between MRI results and surgical findings, encompassing both cases of tears and non-tears. In this sample, accuracy stands at 93.00%, demonstrating a strong alignment between the two diagnostic methods. These metrics establish MRI as a robust and reliable diagnostic tool for identifying rotator cuff injuries, with impressive accuracy in most cases. However, additional metrics, such as specificity, should also be considered to evaluate MRI’s ability to correctly identify cases where no tear is present.
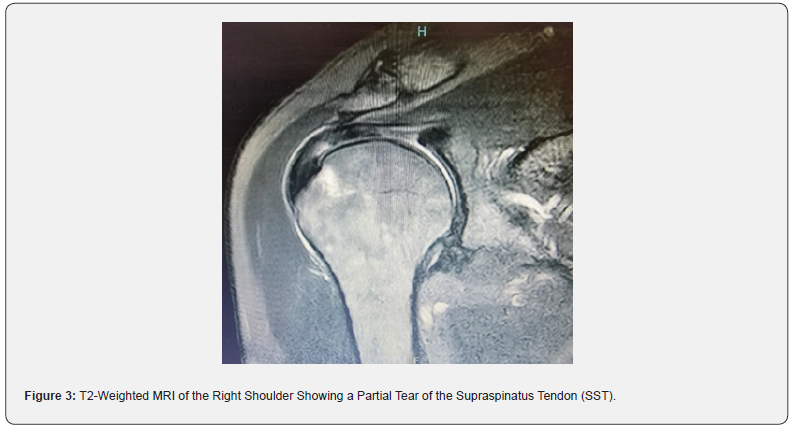
This section outlines the key performance metrics used to evaluate the accuracy of MRI in diagnosing rotator cuff injuries. True Positive (TP) refers to the number of cases where MRI correctly identified a tear, subsequently confirmed by surgery. In this sample, 91 cases were identified as true positives, demonstrating a high capability of MRI to detect tears accurately. A T2-weighted MRI scan of the right shoulder demonstrates a complete tear of the supraspinatus tendon (SST). The image highlights the disrupted tendon fibers and associated fluid signal, which are hallmark features of a full-thickness tear. T2-weighted sequences are particularly effective in visualizing soft tissue injuries due to their ability to emphasize fluid accumulation and inflammation. This finding aligns with the surgical confirmation of rotator cuff injuries, reinforcing the high sensitivity of MRI in detecting full-thickness tears and its critical role in pre-surgical planning and clinical decision-making (see Figure 2 in the Appendix). Additionally, another T2-weighted MRI scan shows a partial tear of the supraspinatus tendon (SST), emphasizing the limitations of MRI in detecting partial-thickness tears. The image reveals subtle disruptions in tendon fibers with less pronounced fluid signal compared to full-thickness tears. Such findings highlight the diagnostic challenge of differentiating between partial and complete tears in MRI (see Figure 3 in the Appendix).

Conversely, False Negative (FN) represents cases where MRI failed to detect a tear that was confirmed by surgery. Four such cases were identified, highlighting a limitation in MRI’s ability to identify all existing tears. False Positive (FP) refers to cases where MRI indicated a tear, but surgery did not confirm its presence. In this sample, three cases were false positives, suggesting a potential for some false alarms in diagnosis.
Finally, True Negative (TN) represents instances where both MRI and surgical findings agreed that no tear was present. In this sample, two cases were accurately identified as true negatives. These metrics provide a comprehensive understanding of MRI’s diagnostic performance, emphasizing its high accuracy while acknowledging areas for potential improvement.
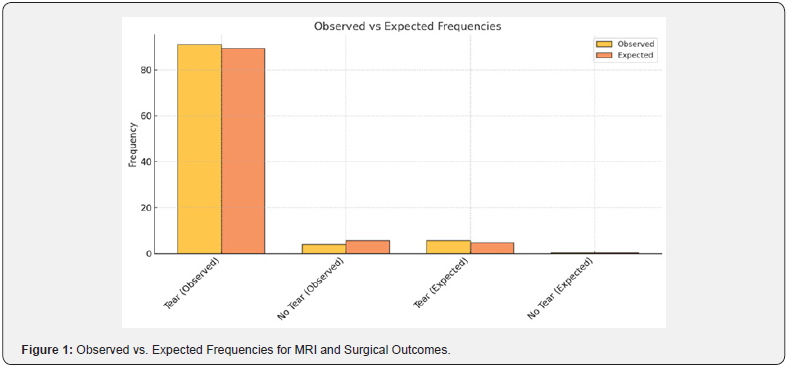
The results indicate a statistically significant association between MRI findings and surgical outcomes. The Chi-square test shows a strong correlation between the two diagnostic methods, with a value of χ² (1) = 10.87, p = 0.001 (p < 0.01). The MRI demonstrated high sensitivity (approximately 95.79%) and an overall accuracy of 93%, reinforcing its reliability in detecting rotator cuff injuries. However, the number of true negatives (TN) was relatively small, highlighting a limitation in specificity. This suggests that while MRI is highly effective in identifying tears, its ability to accurately confirm the absence of tears may require further optimization (see Table 1 in the Appendix). This suggests that while MRI is highly effective in identifying tears, its ability to accurately confirm the absence of tears may require further optimization (Figure 1).

This report evaluates the relationship between MRI findings and surgical outcomes for diagnosing rotator cuff injuries. The Chi-square test was conducted to assess the statistical significance of the association.
Discussion
The findings of this study emphasize MRI’s diagnostic reliability in identifying rotator cuff injuries, particularly fullthickness tears (FTTs), when compared to surgical findings as the gold standard. MRI successfully detected most of the tears confirmed during surgery, demonstrating its value as a primary diagnostic tool for such injuries. This aligns with existing literature, which highlights MRI’s ability to visualize soft tissue structures effectively, making it a reliable method for detecting FTTs [4,6]. The study also reveals that MRI is less effective in distinguishing no-tear outcomes accurately, as it occasionally identifies tears in cases where no tear exists. This limitation is consistent with prior findings that MRI may overestimate pathology due to overlapping signal intensities between degenerative changes and actual tears, particularly in cases of partial-thickness tears (PTTs) [10].
These results suggest the need for cautious interpretation of MRI findings, particularly in patients without evident symptoms. Moreover, this study supports the significant association between MRI findings and surgical outcomes, reinforcing its role as a non-invasive imaging modality for diagnosing rotator cuff injuries. However, the limitations observed in no-tear diagnoses underscore the necessity of supplementary approaches. Technologies like compressed sensing MRI (CS-MRI) and IDEALIQ imaging have shown potential in refining diagnostic accuracy and reducing false-positive results by incorporating advanced imaging techniques and quantitative data [3,7]. In clinical practice, MRI remains a critical tool for evaluating rotator cuff injuries, especially for symptomatic patients with suspected FTTs. Yet, to enhance accuracy and reduce unnecessary interventions, MRI results should be integrated with clinical assessments. This aligns with recommendations in the literature advocating for a multimodal diagnostic approach that combines imaging findings with clinical evaluations to provide a more comprehensive assessment of rotator cuff pathology [10].
Emerging advancements, such as deep learning-based diagnostic systems and synthetic MRI, offer promising solutions to address the limitations highlighted in this study. These technologies have demonstrated improved diagnostic accuracy by minimizing false negatives and enhancing tear classification [7,8]. Incorporating such innovations into routine practice may further solidify MRI’s role in diagnosing rotator cuff injuries while improving overall clinical outcomes. In conclusion, while MRI is a reliable tool for diagnosing rotator cuff injuries, particularly FTTs, its limitations in detecting no-tear outcomes highlight the importance of combining imaging findings with clinical data. Future efforts should focus on integrating advanced imaging technologies to optimize diagnostic precision and support more effective patient management [4,6,10].
While MRI demonstrated strong diagnostic performance, several limitations should be addressed to enhance its reliability and applicability. The relatively small sample size, while adequate for a pilot study, limits the generalizability of the findings. Future research should aim to include larger and more diverse populations to provide broader insights into the diagnostic capabilities of MRI. Additionally, variability in radiological interpretation and surgical techniques may have introduced potential biases, emphasizing the need for standardized protocols in both imaging and surgical documentation. The study also highlighted a limitation in specificity, as evidenced by the low number of true negative cases (n = 2). This finding suggests that MRI’s ability to accurately confirm the absence of rotator cuff tears may require further refinement. Incorporating advanced imaging technologies, such as quantitative MRI techniques and artificial intelligence-based diagnostic tools, could help address these challenges and improve diagnostic precision. Future research should explore these innovations in larger cohorts to validate their effectiveness and enhance the clinical utility of MRI in diagnosing rotator cuff injuries.
References
- Gafoor HF, Jose GA, Narayanan BM (2023) Role of magnetic resonance imaging (MRI) in the diagnosis of rotator cuff injuries and correlation with arthroscopy findings. Cureus 15(12): e50103.
- Koganti DV, Lamghare P, Parripati VK, Khandelwal R, Reddy AD (2022) Role of magnetic resonance imaging in the evaluation of rotator cuff tears. Cureus 14(1): e22873.
- Guo M, Wang W, Li M (2024) Compressed sensing magnetic resonance imaging (CS-MRI) diagnosis of rotator cuff tears. American Journal of Translational Research 16(1): 147-154.
- Li WF, Shakir TM, Zhao Y, Chen T, Niu C, et al. (2019) An evidence-based approach to assess the accuracy of MRI in diagnosing rotator cuff tears: A systematic review and meta-analysis. Iranian Journal of Radiology 16(2): e79079.
- Darai N, Pokhrel S, Shu R, Zhang X, Liu J, et al. (2016) Comparison with surgical findings for the accuracy of routine MRI in rotator cuff tears. Open Journal of Radiology 6(2): 73-83.
- Liu F, Dong J, Shen WJ, Kang Q, Zhou, D, et al. (2020) Detecting rotator cuff tears: A network meta-analysis of 144 diagnostic studies. Orthopaedic Journal of Sports Medicine 8(2): 2325967119900356.
- Tian Z, Ni Y, He H, Tian B, Gong Ret al. (2024) Quantitative assessment of rotator cuff injuries using synthetic MRI and IDEAL-IQ imaging techniques. Heliyon 10(17): e13920.
- Kim M, Park HM, Kim JY, Kim SH, Hoeke S, et al. (2020) MRI-based diagnosis of rotator cuff tears using deep learning and weighted linear combinations. In Machine Learning for Healthcare Conference pp: 292-308.
- Lin DJ, Schwier M, Geiger B, Raithel E, Von Busch H, et al. (2023) Deep learning diagnosis and classification of rotator cuff tears on shoulder MRI. Investigative Radiology 58(6): 405-412.
- Thiagarajan A, Nagaraj R, Marathe K (2021) Correlation between clinical diagnosis, MRI, and arthroscopy in diagnosing shoulder pathology. Cureus 13(12): e20654.
- Liu F, Cheng X, Dong J, Zhou D, Han S, Yang Y (2020) Comparison of MRI and MRA for the diagnosis of rotator cuff tears: A meta-analysis. Medicine 99(12): e19579.
- Zhang X, Gu X, Zhao L (2021) Comparative analysis of real‐time dynamic ultrasound and magnetic resonance imaging in the diagnosis of rotator cuff tear injury. Evidence‐Based Complementary and Alternative Medicine 2021(1): 2107693.






























