Solitary Bone Plasmacytoma in the Bones of the Hand - Case Report
Lázaro Martín Martínez E1, Leonardo Martínez A2, Lázaro Martínez A2, Ramón Delgado C3, Lumey Hernández N4 and Claribel Plain Pazos5*
1Doctor in Medical Sciences, II Degree Specialist in Orthopedics and Traumatology, Full Professor, University General Hospital Mártires del 9 de Abril. Villa Clara. Cuba
2Specialist in Orthopedics and Traumatology, Instructor Professor, University General Hospital Mártires del 9 de Abril. Villa Clara. Cuba
3I and II Degree Specialist in Orthopedics and Traumatology, Assistant Professor, University General Hospital Milián Castro. Villa Clara. Cuba
4Pathological Anatomy Specialist, Assistant teacher. Researcher. Hospital “Mártires del 9 de Abril” Sagua la Grande, Villa Clara, Cuba
5I and II Degree Specialist in Comprehensive General Medicine, Faculty of Medical Sciences of Sagua la Grande, Cuba
Submission: June 06, 2024; Published: July 26, 2024
*Corresponding author: Claribel Plain Pazos, Faculty of Medical Sciences of Sagua la Grande, Villa Clara, Cuba
How to cite this article: Lázaro Martín Martínez E, Leonardo Martínez A, Lázaro Martínez A, Ramón Delgado C, Lumey Hernández N, et al. Solitary Bone Plasmacytoma in the Bones of the Hand - Case Report. Ortho & Rheum Open Access J. 2024; 23(4): 556119. DOI: 10.19080/OROAJ.2024.23.556119
Summary
Although hand injuries are common, bone tumors are not. Solitary bone plasmacytoma is a low-frequency disease, even more so in the bones of the hand. It is characterized by one or two bone lesions without disseminated disease, although it has been associated with multiple myeloma.
Case presentation: A 55-year-old male patient, with a medical history, a manual worker, who came to the clinic due to pain in his hand. Radiological and histological diagnosis is made. Surgical treatment and radiotherapy are performed. It evolves well in five years.
Conclusion: Treatment and annual follow-up are carried out and the patient progresses adequately.
Keywords: Solitary plasmacytoma; Rib; Multiple myeloma; Positive diagnosis; Radiotherapy
Introduction
Solitary bone plasmacytoma (POS) is a neoplasm characterized by monoclonal proliferation of plasma cells without involving bone marrow disorder. It represents between 2 and 10% of plasma cell neoplasms [1,2]. It is classified by the WHO into: Solitary plasmacytoma of bone and Solitary extra-medullary plasmacytoma, the latter affecting the upper airway in up to 90% of cases [3]. It has a predilection for the male sex, with a 2.4:1 ratio; In particular, with respect to extramedullary plasmacytoma, the ratio could even be 3:1.8 The average age of manifestation is 55 years, whether it is extramedullary plasmacytoma or solitary bone plasmacytoma. This age is 10 years younger compared to the usual manifestation of multiple myeloma. It mainly affects the red marrow contained in the axial skeleton. The spine is affected in 34 to 72% of cases, the thoracic level is the most affected. The ribs, sternum, clavicle or scapula are affected in 20% of cases. The bones of the hand are rarely affected [4]. Due to the rarity of the type of tumor and its rarer location in the bones of the hand, it was decided to present this patient.
Presentation of the Case
White male patient, named AEE, who has been coming to the clinic with pain in his hands for several months. He is a manual worker in a food processing industry (cow milk). He has no family or personal history of chronic diseases. Several months ago, he began to have pain in his hands, after which he presented deformities in some joints of both hands, he had difficulty performing significant physical effort with his hands but it did not disable him from carrying out daily life and his work. It was interpreted in a first evaluation at another institution as rheumatoid arthritis.
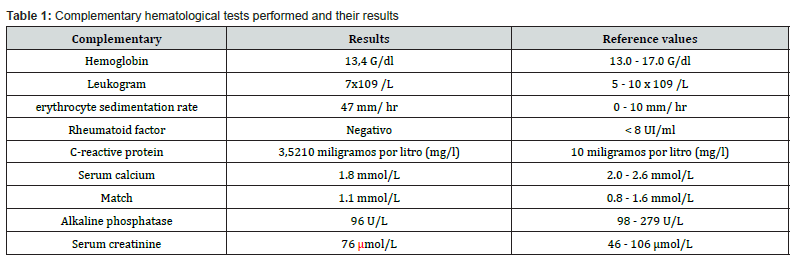
We perform a general and special interrogation and physical examination of both hands. We found no conditions in the general physical examination, but in the special examination of the hands, there are visible and palpable tumors in the right hand, the most striking in the head of the third metatarsal, although they also exist in the distal phalanx of the same finger (Figure 1). We perform complementary hematological and radiological examinations (Table 1). A bone marrow aspiration biopsy was performed, looking for MM, a test that was negative, as was the protein electrophoresis. We performed surgery to excise the lesion and sample for biopsy. Biopsy number B-231.22 at the Mártires del 9 de Abril Hospital and number IHQ-938.22 at the Hermanos Amejeiras national hospital. Biopsy of the bones of the hand - head of the third metacarpal - with clinical diagnosis of bone tumor, immunohistochemical tests are performed.
i. PAN CK- Negative.
ii. CD 99- Negative.
iii. VIVENTINA- Negative.
iv. CD 79a- Positive.
v. DC 20- Negative.
vi. MUM 1- Positive.
vii. KI67- 50%.
Diagnosis. Plasmocytoma. Infiltration by plasma cells.

Discussion of the Case
Plasmacytomas are rare neoplastic tumors, located outside the bone marrow, more frequent in the upper respiratory tract and with a very low frequency retroperitoneal. Between 1905 and 1997 patients between the fourth and seventh decade of life were found; Of 714 cases, 17.8% consisted of extramedullary plasmacytomas [5]. Solitary bone plasmacytoma is a rare plasma cell tumor that has been observed as a precursor to multiple myeloma; It is located mainly in the spine, causing pain at the thoracic and/or lumbar level. Solitary bone plasmacytoma is located mainly in the spine (50% of cases) or in the peripheral long bones. More unusual presentations have been described, such as the coxofemoral joint, chest wall, maxillary sinus, or skull [6]. To make a positive diagnosis of POS requires a series of criteria, firstly histological evidence of a neoplastic mass of plasma cells in a bone. In the case presented, a bone tumor was found that destroyed part of the head of the third metacarpal. In radiological studies carried out in other portions of the body, there are no lytic lesions.
In the case presented, despite also performing bone marrow aspiration biopsy, no criteria for Multiple Myeloma were found. There is no anemia, hypercalcemia or renal failure. Nor do immunoelectrophoresis in blood and urine present a monoclonal peak for a possible diagnosis of multiple myeloma. All of these approaches are positive diagnostic criteria [3]. The definitive diagnosis is currently based on biopsy and histological and immunohistochemical confirmation of homogeneous infiltrate of plasma cells, which typically express CD138, CD38 or both [7]. The differential diagnosis of this type of tumors includes primary neoplasms, benign neoplasms and metastases in rare cases, being a diagnostic and therapeutic challenge, due to its low incidence in this location.
Treatment includes surgical excision for histological diagnosis and local radiotherapy is the treatment of choice, with a response greater than 90%. The recurrence rate is higher in the elderly and in those subjects with involvement of the axial skeleton. The predictive factors for progression to MM are: tumor size, the presence of osteopenia and the non-reduction of the monoclonal peak after treatment [8]. Solitary bone plasmacytoma has a progression rate to multiple myeloma of 65 to 84% in 10 years and 65 to 100% in 15 years. The average onset of conversion to multiple myeloma is two to five years. According to Kyle, three patterns of treatment failure are considered: appearance of multiple myeloma in 54%, local recurrence in 11%, and appearance of new bone lesions in the absence of multiple myeloma in 2% [9].
References
- Dermatomyositis (2019) Hopkinsmedicine.org.
- Qudsiya Z, Waseem M (2024) Dermatomyositis In: StatPearls [Internet]. Treasure Island (FL): StatPearls.
- Dermatomyositis (2024) Mayo Clinic.
- Marvi U, Chung L, Fiorentino DF (2012) Clinical presentation and evaluation of dermatomyositis. Indian J Dermatol 57(5): 375-381.
- Chu LL, Rohekar G (2019) Dermatomyositis. Canadian Medical Association J 191(12): E340-E340.
- Bolender CM, Jimenez A, Clarke JT, Willson TM, Stevens VW, et al. (2022) Incidence of dermatomyositis in a nationwide cohort study of US veterans. JAMA Dermatol 158(11): 1321-13232.
- Fiorillo L, Meroni PL, Parodi A (2020) Dermatomyositis and polymyositis. Autoimmunity Rev 19(7): 102668.
- Koler RA, Montemarano A (2001) Dermatomyositis. American Family Physician 64(9): 1565-1572.
- Vleugels RA, Callen JP, Fiorentino DF (2021) Dermatomyositis: Clinical features and pathogenesis. JAMA Dermatol 157(2): 128-139.
- Marie I, Hatron PY, Dominique S (2020) Epidemiology of inflammatory myopathies in a nationwide registry: Incidence and mortality in a long-term perspective. Autoimmunity Rev 19(7): 102668.
- Rothwell S, Chinoy H, Lamb JA (2021) Genetics of idiopathic inflammatory myopathies: Insights into disease pathology. Nature Rev Rheumatol 17(10): 622-634.
- Khunsriraksakul C, Li Q, Markus H, Patrick MT, Sauteraud R, et al. (2023) Multi-ancestry and multi-trait genome-wide association meta-analyses inform clinical risk prediction for systemic lupus erythematosus. Nature Communic 14(1): 668.
- Dalakas MC (1991) Polymyositis, dermatomyositis, and inclusion-body myositis. New England J Med 325(21): 1487-1498.
- Mastaglia FL, Phillips BA (2002) Idiopathic inflammatory myopathies: epidemiology, classification, and diagnostic criteria. Rheumatic Dis Clin North America 28(4): 723-741.
- Callen JP (2000) Dermatomyositis. Lancet 355(9197): 53-57.
- Sontheimer RD (1999) Cutaneous features of classic dermatomyositis and amyopathic dermatomyositis. Curr Opin Rheumatol 11(6): 475-482.
- Marie I, Hachulla E (2002) Pulmonary involvement in polymyositis and dermatomyositis. Curr Opin Rheumatol 14(6): 663-668.
- Lundberg IE (2006) The heart in dermatomyositis and polymyositis. Rheumatol 45(Suppl_4): 18-21.
- Marie I, Guillevin L (2001) Gastrointestinal involvement in polymyositis and dermatomyositis. Rheumatol 40(8): 741-744.
- Tansley SL, Betteridge ZE (2013) The diagnostic utility of autoantibodies in adult and juvenile myositis. Curr Opin Rheumatol 26(6): 772-777.
- Mammen AL (2010) Autoantibodies in dermatomyositis. Curr Rheumatol Rep 12(4): 192-198.
- Greenberg SA (2010) Dermatomyositis and type 1 interferons. Curr Rheumatol Rep 12(3): 198-203.
- Dalakas MC (2011) Inflammatory muscle diseases. New Engl J Med 364(18): 1734-1747.
- Miller FW, Rider LG (1996) Genetics and environmental aspects of inflammatory muscle diseases. Rheumatic Disease Clinics of North America 22(4): 757-773.
- Fujimoto M, Watanabe R (2014) Environmental factors and autoimmunity. Immunology and Allergy Clinics of North America 34(1): 35-48.
- Bohan A, Peter JB (1975) Polymyositis and dermatomyositis (first of two parts). New England J Med 292(7): 344-347.
- Hoogendijk JE, Amato AA (2004) 119th ENMC International Workshop: trial design in adult idiopathic inflammatory myopathies, with the exception of inclusion body myositis, 10-12 October 2003, Naarden, The Netherlands. Neuromuscular Disorders, 14(5): 337-345.
- Moxley RT, Griggs RC (1977) Polymyositis and dermatomyositis. Evaluation and treatment. Arch Dermatol 113(10): 1435-1442.
- Chinoy H, Oddis CV (2011) The diagnostic utility of myositis autoantibody testing. Curr Opin Rheumatol 23(6): 658-664.
- Dimachkie MM, Barohn RJ (2014) Idiopathic inflammatory myopathies. Seminars Neurol 34(3): 225-236.
- Dalakas MC (2015) Inflammatory muscle diseases. New England J Med 372(18): 1734-1747.
- Sontheimer RD (2002) Dermatomyositis: an overview of recent progress with emphasis on dermatologic aspects. Dermatol Clin 20(3): 387-408.
- Qudsiya Z, Waseem M (2024) Dermatomyositis. [Updated 2023 Aug 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls.
- Chung MP, Paik JJ (2022) Past, Present, and Future in Dermatomyositis Therapeutics. Curr Treatm Opt Rheumatol 8(4): 71-90.
- Sevim E, Kobrin D, Casal-Dominguez M, Pinal-Fernandez I (2024) A comprehensive review of dermatomyositis treatments - from rediscovered classics to promising horizons. Expert Rev Clin Immunol 20(2): 197-209.
- Pinal-Fernandez I, Casal-Dominguez M, Mammen AL (2018) Immune-mediated necrotizing myopathy. Curr Rheumatol Rep 20(4): 21.
- Lilleker JB, Vencovsky J, Wang G, Wedderburn LR, Diederichsen LP, et al. (2018) The idiopathic inflammatory myopathies: spectrum of diseases, diagnosis and management. Rheumatology (Oxford) 57(suppl_2): vii32-vii42.
- Schmidt J (2018) Current classification and management of inflammatory myopathies. J Neuromuscul Dis 5(2): 109-129.
- Mariampillai K, Granger B, Amelin D (2017) Development of a clinical risk score for cancer in patients with dermatomyositis. JAMA Dermatol 153(7): 1-9.
- Oldroyd A, Lilleker JB, Chinoy H (2021) Idiopathic inflammatory myopathies: diagnostic mimics and differential diagnosis. Rheumatology (Oxford) 60(Suppl_2): 114-124.
- Rider LG, Lachenbruch PA, Monroe JB (2016) Damage extent and predictors in adult and juvenile dermatomyositis and polymyositis using the Myositis Damage Index. Arthritis Rheumatol 68(8): 1865-1876.
- Sultan SM, Ioannou Y, Moss K, Isenberg DA (2002) Outcome in patients with idiopathic inflammatory myositis: morbidity and mortality. Rheumatology (Oxford) 41(1): 22-26.
- Shah M, Mamyrova G, Targoff IN, Adam MH, James DM, et al. (2013) The clinical phenotypes of the juvenile idiopathic inflammatory myopathies. Medicine (Baltimore) 92(1): 25-41.
- Huber AM, Lang B, LeBlanc CM, Birdi N, Bolaria RK, et al. (2000) Medium- and long-term functional outcomes in a multicenter cohort of children with juvenile dermatomyositis. Arthritis Rheum 43(3): 541-549.
- Ortiz RA, Díaz LA, Casanova Seuma JM (2011) Dermatomyositis. Piel (Barc) 26(7): 330-340.
- Martiarena A, Aldamiz-Echebarria M, Martínez C, García JJ (2014) Actualización en el tratamiento de la dermatomiositis; a propósito de un caso. Farm Hosp 38(6): 486-497.
- Aguayo R, Martínez C, García JJ (2011) Pathophysiological Mechanisms and Treatment of Dermatomyositis and Immune Mediated Necrotizing Myopathies: A Focused Review. Int J Mol Sci 23(8): 4301.






























