A Single Injection of Autologous, Peripheral Stem Cells Combined with Stem-Cell Derived Exosomes Significantly Improves Symptoms in Patients with Severe Grade-IV Osteoarthritis of the Knee
Patrick Weninger*, Angelika Reich and Murat Özcelik
Avancell Medical GmbH, Liechtensteinstrasse, Vienna, Austria
Submission: June 12, 2024; Published: June 19, 2024
*Corresponding author: Patrick Weninger, Avancell Medical, Liechtensteinstrasse 96 1090 Vienna, Austria, Email: office@avancell-joint.com
How to cite this article: Patrick W, Angelika R, Murat Ö. A Single Injection of Autologous, Peripheral Stem Cells Combined with Stem-Cell Derived Exosomes Significantly Improves Symptoms in Patients with Severe Grade-IV Osteoarthritis of the Knee. Ortho & Rheum Open Access J. 2024; 23(3): 556114. DOI: 10.19080/OROAJ.2024.23.556114
Abstract
Introduction: Osteoarthritis (OA) is a disabling joint disease with more than 654.1 million affected patients worldwide in 2020. There are different strategies to treat cartilage defects or OA of the knee. In general, conservative or surgical options are available. In this manuscript we describe a technique using peripheral stem cells from patient peripheral blood combined with stem cell-derived exosomes to treat patients with grade IV OA of the knee. We further present the effect of such treatment on outcome parameters six months after the intervention.
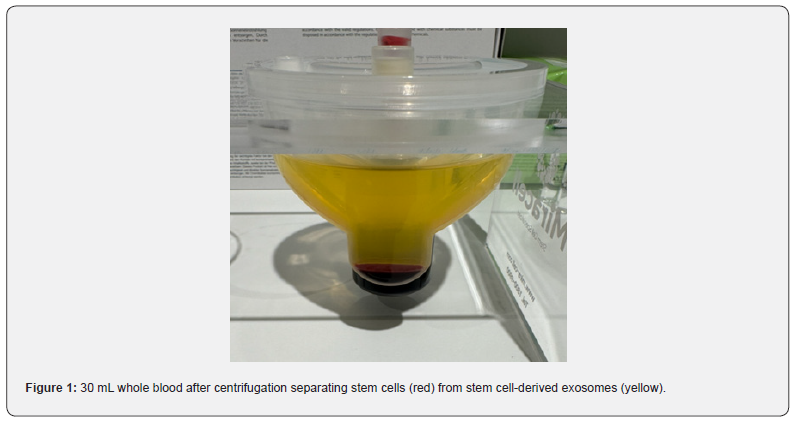
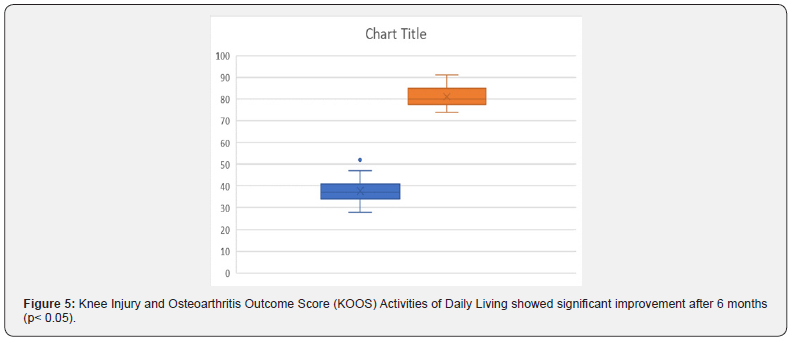
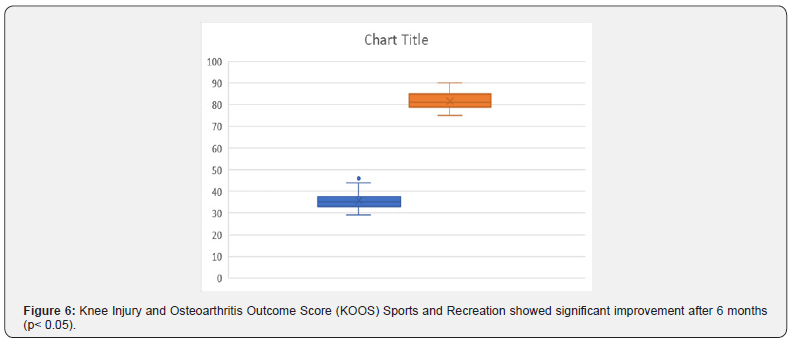
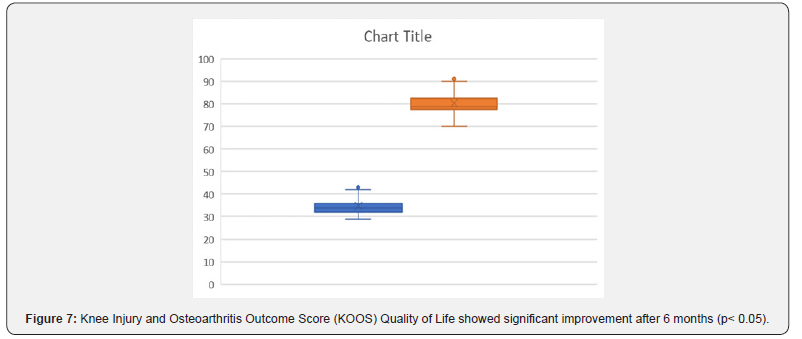
Material and Methods: Between March and December 2023 39 individuals (45 knees) were treated with grade IV OA of the knee (45 knees) in one or more compartments (medial, lateral, retropatellar). In each patient, 30mL venous blood were centrifuged by using a special centrifuge for stem cell isolation (SMART Cell BSC, Miracell, South Korea) for 17 minutes with 2,500 round per minute in a process that separates peripheral stem cells and their exosomes from the erythrocyte fraction. After the centrifugation process, the stem cells and the stem cell-derived exosomes were mixed and injected with a 15 mL syringe into the affected knee joint. Before and six months after the intervention, we analyzed visual analogue scale (VAS) and the Knee Injury and Osteoarthritis Outcome Score (KOOS).
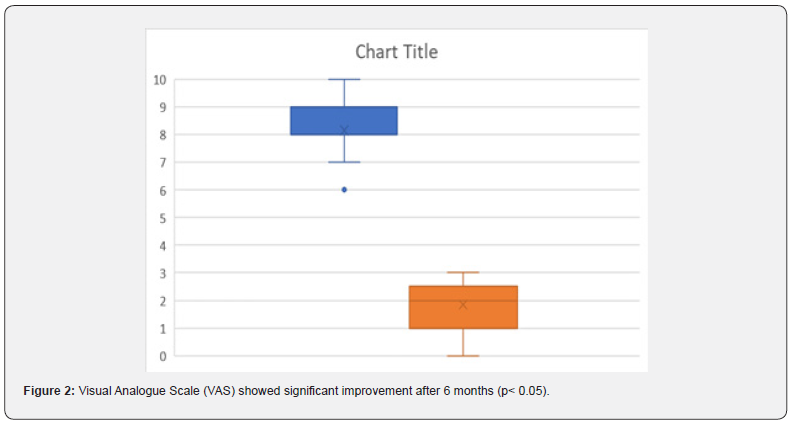
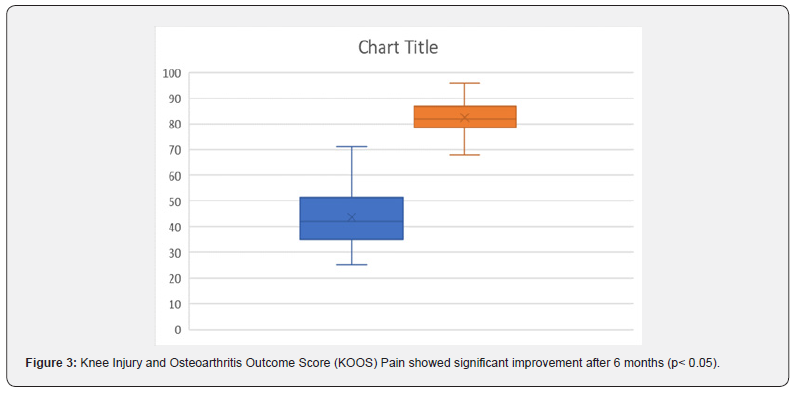
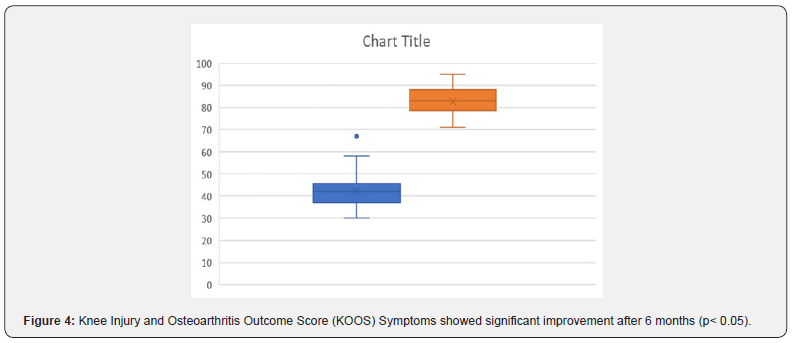
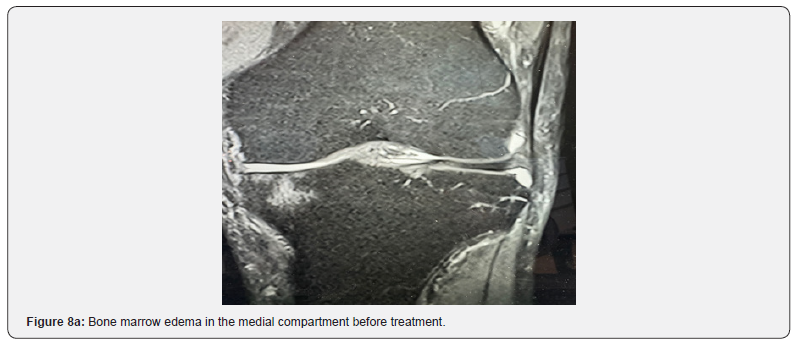
Results: In all patients, OA symptoms improved after one single injection of 10 mL stem cells combined with their exosomes. There were no adverse effects related to the injection. VAS significantly improved in all patients six months after the intervention (p< 0.05). Also, KOOS values showed significant improvement after six months in all patients (p< 0.05). All patients stated they are satisfied and also stated they should have undergone the procedure earlier. In 11 patient magnetic resonance imaging (MRI) scans showed successful treatment of bone marrow edema after 6 weeks despite full weight bearing.
Discussion: The here described treatment seems to be a safe and effective method to significantly and reproducibly improve symptoms in patients suffering from severe OA of the knee after six months. Before the intervention, all patients were advised to undergo total knee arthroplasty (TKA) but they refused and consulted our institution for second opinion. Considering major surgery and possible complications of TKA, the here described method seems to be an alternative to treat symptoms non-operatively without associated risks before undergoing joint replacement. Further research and larger clinical studies are necessary to allow interpretation of outcome also for the long-term course.
Keywords: Osteoarthritis; Erythrocyte fraction; Magnetic resonance imaging; Pain medications or physiotherapy; Cartilage transplantation
Abbreviations: OA: Osteoarthritis; VAS: Visual Analogue Scale; KOOS: Knee Injury and Osteoarthritis Outcome Score; MRI: Magnetic Resonance Imaging; TKA: Total Knee Arthroplasty
Introduction
Osteoarthritis (OA) is a disabling joint disease with more than 654.1 million affected patients worldwide in 2020. By 2025, the number of individuals suffering from OA is expected to rise above 700 million. The global incidence of OA of the knee was 203 per 10,000 person-years (95% CI, 106-331) in individuals aged 20 and over. There were around 86.7 million individuals with incident knee OA in 2020 [1-4]. The main risk factors to develop OA are age, overweight, rheumatic diseases, traumatic injuries and metabolic disorders [5]. It is generally accepted that the cartilage tissue has no blood perfusion and once damaged does not regenerate [6]. There are different strategies to treat cartilage defects or OA of the knee. In general, conservative or surgical options are available. Conservative treatment includes visco-supplementation, corticoid injections, pain medications or physiotherapy [7-9]. Joint preserving surgical treatment incudes arthroscopic or (mini-) open procedures such as mosaicplasty, matrix-associated cartilage transplantation, strategies involving minced cartilage transfer or bone marrow stimulating operations with or without alignment correction [10-12].
In case of severe OA of the knee, partial or total knee joint replacement is often recommended in case of severe pain and impaired life quality. As every surgical procedure, knee replacement can be associated with significant complications, namely infection, thrombo-embolic events, periprosthetic fractures, nerve damage, arthrofibrosis and side effects or complications related to anesthesia [13-17]. One also has to consider a limited life expectancy of hardware and the need for reoperation. Also, if complications occur, revision surgery is needed in most cases what has major impact on socio-economic structures [18,19]. Within the past decade ortho-biologic treatment options have emerged also for patients with cartilage damage. These include platelet-rich plasma, autologous stem cells or cell-derived exosomes [20-23]. Recent studies showed encouraging results when using such strategies. In this manuscript we describe a technique using peripheral stem cells from patient peripheral blood combined with stem cell-derived exosomes to treat patients with grade IV OA of the knee. We further present the effect of such treatment on outcome parameters six months after the intervention.
Material and Methods
Between March and December 2023 39 individuals (45 knees) were treated with grade IV OA of the knee (45 knees) in one or more compartments (medial, lateral, retropatellar). There were 31 male and 18 female patients. In each knee, we used 30 mL of peripheral venous blood to harvest the cells and to produce the stem cell-derived exosomes. Blood samples were centrifuged by using a special centrifuge for stem cell isolation (SMART Cell BSC, Miracell, South Korea) for 17 minutes with 2,500 round per minute in a process that separates peripheral stem cells and their exosomes from the erythrocyte fraction. Figure 1 shows the product after centrifugation with separated stem cells and their exosomes (Figure 1). After the centrifugation process, the stem cells and the stem cell-derived exosomes were mixed and injected with a 15 mL syringe into the affected knee joint with a 20-G needle under ultrasound guidance (Clarius, Canada) as a single-shot procedure. Patients were advised to bear full weight and to move the knee as tolerated. We advised not to do running or jumping sports for 8 weeks. Before and six months after the intervention, we analyzed visual analogue scale and the Knee Injury and Osteoarthritis Outcome Score (KOOS). For statistical analysis SPSS was used (SPSS, USA). Level of statistical significance was set at p < 0.05.
Results
In all patients, OA symptoms improved after one single injection of 10 mL stem cells combined with their exosomes. There were no adverse effects related to the injection. No patients reported worse or equal symptoms at six months follow-up. Eight patients had slightly increased pain associated to knee swelling during the first three days after treatment which was treated using ice packs and a non-steroidal antiphlogistic drug (Paracetamol 500 mg). VAS significantly improved in all patients six months after the intervention. Also, KOOS values showed significant improvement after six months in all patients. All patients stated they are satisfied and also stated they should have undergone the procedure earlier. The results are presented in Figures 2-7. In 11 patient magnetic resonance imaging (MRI) scans showed successful treatment of bone marrow edema after 6 weeks despite full weight bearing. Figure 8 shows the MRI scan of a 79-years old male patient before and after the intervention.
Discussion
The use of stem cells as possible approach to treat cartilage defects has been recently described. In this context, it has to be mentioned that different authors report on different sources of stem cells and stem cell-rich tissue, namely three major sources: fat, bone marrow and blood [21-25]. Whereas using bone marrow aspirated and bone marrow stem-cells is more common, harvesting stem cell-rich fat is a relatively new practice. Recently, encouraging results were reported using the so called stromal vascular fraction and adipose-derived stem cells in patients with OA [26,27]. It has to be pointed out that current regulatories in the European Union consider the transfer of fat from the abdomen to the knee as non-homologous use. Therefore, its routine use must be questioned and needs further authorization. Current practice is to inject abdominal fat tissue into the Hoffa-fat pad (“fat to fat”) [28]. This also means the use of fat grafts for other joints (e.g. hip, shoulder, ankle) is problematic as they do not have fat tissue. In our opinion, the fat tissue is an active tissue and contains numerous cells of different origin that are actively producing secretomes. So actually, transferring such cells and their components from one tissue to another in the same individual is transferring cells from on cell-containing tissue to another (homologous use). Nevertheless, the use of peripheral stem cells from autologous blood can be a promising treatment options in terms of reproducibility and is easier approachable than fat tissue (liposuction needed) or bone marrow (bone marrow puncture and aspiration needed). To isolate peripheral stem cells, a simple venous puncture is needed, which makes it easier for both, the patient and the healthcare provider. The use of peripheral stem cells for treating cartilage damage was described recently by Zhu et al. [29].
In a systematic review the authors found that stem cells derived from peripheral blood can repair cartilage and are an important resource to treat cartilage injuries. Also, the role of exosomes has been highlighted repeatedly in recent past. Wu et al described that exosomes can rewire the cartilage microenvironment in patients with OA and pointed out their role for cartilage repair in future [30]. This was also mentioned by He et al who found that exosomes are able to reduce pain and cartilage defects in a rat model of OA. The role of exosomes on the reduction of proinflammatory cytokines was also emphasized by He et al. [31]. Also, in our patients we found pain reduction at very early stages (first follow-up after three days) that might be attributed to the shift from pro- to anti-inflammation. It was surprising, though, that also bone marrow edema disappeared as visualized on MRI per- and post-intervention.
To the best of our knowledge, this is the first report providing reliable data on the efficacy and safety of peripheral stem cells and their exosomes in patients with grade IV knee OA. The here described treatment seems to be a safe and effective method to significantly and reproducibly improve symptoms in patients suffering from severe OA of the knee after six months. Before the intervention, all patients were advised to undergo total knee arthroplasty (TKA) but they refused and consulted our institution for second opinion. Considering major surgery and possible complications of TKA, the here described method seems to be an alternative to treat symptoms non-operatively without associated risks before undergoing joint replacement. Further research and larger clinical studies are necessary to allow interpretation of outcome also for the long-term course.
References
- Pereira D, Peleteiro B, Araujo J, Branco J, Santos RA, et al. (2011) The effect of osteoarthritis definition on prevalence and incidence estimates: a systematic review. Osteoarthritis Cartilage 19(11): 1279-1285.
- Mahmoudian A, Lohmander LS, Mobasheri A, Martin E, Frank PL (2021) Early-stage symptomatic osteoarthritis of the knee - time for action. Nat Rev Rheumatol 17(10): 621-632.
- Sharma L (2021) Osteoarthritis of the knee. N Engl J Med 384(1): 51-59.
- Hunter DJ, Schofield D, Callander E (2014) The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol. 10(7): 437-441.
- Palazzo C, Nguyen C, Levefre-Colau MM, François R, Serge P (2016) Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med 59(3): 134-138.
- Suri P, Morgenroth DC, Hunter DJ (2012) Epidemiology of osteoarthritis and associated comorbidities. PM R 4(Suppl): S10-19.
- MacFarlane LA, Mass H, Collins JE, Elena L, Jeffrey NK, et al. (2023) Response to intra-articular cortisone injections in knee osteoarthritis patients with and without effusion on ultrasound: a pilot study. Osteoarthr Cartil Open 5(2): 100361.
- Anil U, Markus DH, Hurley ET, Amit KM, Michael JA, et al. (2021) The efficacy of intra-articular injections in the treatment of knee osteoarthritis: A network meta-analysis of randomized controlled trials. Knee 32: 173-182.
- Singh H, Knapik DM, Polce EM, Carlo KE, Amanda HB, et al. (2022) Relative efficacy of intra-articular injections in the treatment of knee osteoarthritis: a systematic review and network meta-analysis. Am J Sports Med 50(11): 3140-3148.
- Dekker TJ, Aman ZS, De Phillippo NN, Jonathan FD, Adam WA, et al. (2021) Chondral lesions of the knee: an evidence-based approach. J Bone Joint Surg (Br) 103(7): 629-645.
- Calcei JG, Ray T, Sherman SL, Jack FR (2020) Management of large focal chondral and osteochondral defects of the knee. J Knee Surg 33(12): 1187-1200.
- Trofa DP, Hong IS, Lopez CD, Allison JR, Ziqing Y, et al. (2023) Isolated osteochondral autograft versus allograft transplantation fort the treatment of symptomatic cartilage lesions of the knee: a systematic review and meta-analysis. Am J Sports Med 51(3): 812-824.
- Healy WL, Della Valle CJ, Iorio R, et al. (2013) Complications after total knee arthroplasty: standardized list and definitions of the Knee Society. Clin Orthop Rel Res 471(1): 215-220.
- Ma LL, Yu XR, Weng XS, Jin J, Wenwen Q, et al. (2022) Possible risk factors for severe complications occurring after primary total knee arthroplasty. Chin Med Sci J 37(4): 303-308.
- Carter J, Springer B, Curtin BM (2019) Early complications of revision total knee arthroplasty in morbidly obese patients. Eur J Orthop Surg Traumatol 29(5): 1101-1104.
- Cheuy VA, Foran JRH, Paxton RJ, Michael JB, Joseph AZ, et al. (2017) Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty 32(8): 2604-2611.
- Abdul N, Dixon D, Walker A, Joanna H, Nick S, et al. (2015) Fibrosis is a common outcome following total knee arthroplasty. Sci Rep 5: 16469.
- Marsh J, Joshi I, Somerville L, Edward V, Brent L (2022) Health care costs after total knee arthroplasty for satisfied and dissatisfied patients. Can J Surg 65(5): E562-E566.
- Fang CJ, Shaker JM, Ward DM, Andrew J, David AM, Eric LS, et al. (2021) Financial burden of revision hip and knee arthroplasty at an orthopedic specialty hospital: higher costs and unequal reimbursements. J Arthroplasty 36(8): 2680-2684.
- Gilad R, Haunschild ED, Knapik DM, Aghogho E, Kevin CP, et al. (2021) Hyaluronic acid and platelet-rich plasma for the management of knee osteoarthritis. Int Orthop 45(2): 345-354.
- Jo CH, Lee YG, Shin WH, Hyang K, Jee WC, et al. (2014) Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells 32(5): 1254-1266.
- Lee WS, Kim HJ, Kim KI, Beom GK, Wook J (2019) Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med 8(6): 504-511.
- Zhou Q, Cai Y, Jiang Y, Xiangjin L (2020) Exosomes in osteoarthritis and cartilage injury: advanced development and potential therapeutic strategies. Int J Biol Sci 16(11): 1811-1820.
- Pabinger C, Lothaller H, Kobinia GS (2024) Intra-articular injection of bone marrow aspirate concentrate (mesenchymal stem cells) in KL grade III and IV knee osteoarthritis: 4 years results of 37 knees. Sci Rep 14(1): 2665.
- Wu Y, Li J, Zeng Y, Wenchen P, Xiaoyu M, et al. (2022) Exosomes rewire the cartilage microenvironment in osteoarthritis: from inter cellular communication to therapeutic strategies. Int J Oral Sci 14: 40.
- Vargel i, Tuncel A, Baysal N, İrem Hartuç-Ç, Feza K (2022) Autologous adipose-derived tissue stromal vascular fraction (AD-tSVF) for knee osteoarthritis. Int J Mol Sci 23(21): 13517.
- Anil U, Markus DH, Hurley ET, Amit KM, Michael JA, et al. (2021) The efficacy of intra-articular injections in the treatment of knee osteoarthritis: A network meta-analysis of randomized controlled trials. Knee 32: 173-182.
- Labarre KW, Zimmermann G (2022) Infiltration of the Hoffa’s fat pad with stromal vascular fraction in patients with osteoarthritis of the knee - Results after one year of follow-up. Bone Rep 16: 101168.
- Zhu Y, Fu W (2022) Peripheral blood-derived stem cells for the treatment of cartilage injuries: a systematic review. Front Bioeng Biotechnol 10: 956614.
- Wu Y, Li J, Zeng Y, Wenchen P, Xiaoyu M, et al. (2022) Exosomes rewire the cartilage microenvironment in osteoarthritis: from inter cellular communication to therapeutic strategies. Int J Oral Sci 14(1): 40.
- He L, He T, Xing J, Qing Z, Lei F, et al. (2020) Bone marrow mesenchymal stem cell-derives exosomes protect cartilage damage and relieve knee osteoarthritis pain in a rat model of osteoarthritis. Stem Cell Res Ther 11(1): 276.






























