Pain Management: A Psychological Clinical Case in Hospital Care of CBT-Brief Therapy
Tatiana Leal, Marla Vieira and Luísa Soares*
Faculty of Arts and Humanities, Department of Psychology, University of Madeira, Portugal
Submission: May 30, 2024; Published: June 14, 2024
*Corresponding author: Luisa Soares, Faculty of Arts and Humanities, Department of Psychology, University of Madeira, Portugal
How to cite this article: Leal T, Vieira M, Soares L. Pain Management: A Psychological Clinical Case in Hospital Care of CBT-Brief Therapy. Ortho & Rheum Open Access J. 2024; 23(3): 556113. DOI: 10.19080/OROAJ.2024.23.556113
Abstract
This work presents a clinical case of Mrs. T., a 48-year-old female patient referred by the family doctor at the health center in her area of residence for control of right tibiotarsal pain. She fractured her right fibula and tibia, resulting in a plate and screws being placed in her foot. As a result of this fracture, he presented intense complaints to his family doctor, especially during his mobilization, who turned to Pain Medicine to help control the pain. Eight weekly sessions were held. Research shows that CBT-brief therapy is more effective in a hospital context and Mrs T. had CBT-brief therapy. Pre and post psychological assessment were used, and the results show a significantly clinical improvement in depression and anxiety scales as well as in coping pain strategies.
Chronic pain is characterized by persistent or recurrent pain that lasts three or more months [1]. Some constraints that chronic pain causes in an individual's life are recognized, namely: (a) changes in sleep and appetite, (b) emotional variations, (c) concentration difficulties, (d) lack of motivation, (e) inactivity, among others and also for public health, especially with the effective increase in medical costs for patient intervention and the possibility of removal from work [2]. The worsening of these conditions tends to occur due to the accumulation of failed attempts to control pain, which leads most individuals to express feelings of hopelessness and consider giving up. Consequently, we are witnessing the development of comorbidities, particularly with depressive and anxious conditions, which promote the adoption of dysfunctional coping strategies such as avoidance and escape. In cases of chronic pain, it is not uncommon to identify possibilities for patients to seek secondary gains from pain, usually associated with time off work or receiving extra attention from their close circle [1] (Hanson & Gerber, 1990).
Keywords: Cognitive Behavioral Therapy; Depression and anxiety; Lack of motivation; Physical symptoms; Severe pain
Chronic Pain in Adulthood
Although the definition is variable, according to Papalia & Feldman [3], the stage of intermediate adult life corresponds to the period between 40 and 65 years old. During this period, the first limitations in health begin to appear, especially after 45 years. After the age of 50, people move towards reducing their sensitivity to pain, a trend that is combined with muscle loss, creating obstacles to individual well-being since pain is often a consequence of chronic diseases that arise at this age. phase [3]. Lifestyle habits adopted throughout life, such as physical exercise, diet, and consumption (i.e., tobacco, alcohol or drugs) continue to play an important role in health, directly affecting the symptomatic manifestation and development of pathologies [3]. States of anxiety, hopelessness and depression lead to the development of poor health, while in contrast, emotions associated with happiness and hope positively influence individual health, contributing to well-being and quality of life [3,4]. As the nervous system acts under biological systems, these mental states have a direct impact on physical symptoms, contributing to the impairment or good functioning of the immune system and, consequently, to the way in which subjects respond to the manifestations of their diseases [4,5].
The Cognitive-Behavioral Therapy (CBT) intervention model for chronic pain
In psychological intervention in chronic pain, CBT is a comprehensive approach to the biopsychosocial conception of pain, working with patients' cognitions and behavioral responses to it. The aim is to achieve changes in the way patients cognitively represent and react to pain, maximizing their functioning [1,6]. Always collaboratively, the aim is for individuals to reach alternative and positive perspectives on the pain situation with an internal locus of control necessary for its implementation in order to obtain a reduction in pain and greater well-being [1].
Most patients with chronic pain manifest depressive symptoms combined with uncontrollability that leads them to adopt maladaptive and passive coping strategies [1]. It is important to consider the process of self-focus on pain, which directs focus and contributes to a greater perception of its intensity. It is also essential, in this intervention model, to demonstrate that self-surveillance is a relevant strategy but that, in excess, it prevents the decentering of pain, reinforcing the initial representations. Considering that such representations end up leading to behaviors of avoidance, inactivity and demotivation that distance individuals from interpersonal relationships, work and pleasure activities, it is necessary to intervene psychologically to change how to cope with pain [1].
Clinical Case of Mrs. T.
A 48-year-old female patient was referred by the family doctor at the health center in her area of residence for control of right tibiotarsal pain. The patient is married and has two children. About a year ago, she fractured her right fibula and tibia, resulting in a plate and screws being placed in her foot. As a result of this fracture, he presented intense complaints to his family doctor, especially during his mobilization, who turned to Pain Medicine to help control the pain.
Clinical Assessment - Formal and Informal Psychological
Eight weekly sessions were held for 50 minutes each. We will name our patient as Mrs. T. in order to safeguard any clinical and confidential information. Research shows that, in particular, CBT-brief therapy is more effective in a hospital context [7,8]. In this sense, the understanding and intervention of the case was carried out in light of this model. An initial formal and informal psychological assessment, CBT intervention and a post-intervention assessment were carried out. The strategies and techniques used were (a) psychoeducation, (b) alternative thinking training, (c) problem-solving training, (d) self-monitoring strategies, (e) homework assignments (TPC), (f) provision of information, (g) programming of daily tasks, (h) sequential thinking training and (i) diaphragmatic breathing. Given the patient's reason for referral, an informal/formal assessment was carried out through a semi-structured interview that covered (a) physiological aspects of pain, (b) cognitive representations, (c) emotional aspects, (d) environmental factors and (e) behavioral aspects. In addition, clinical behavioral observation was used as well as the following psychometric formal assessment instruments: (a) the HADS; (b) the Mini-Mult (shortened version of the MMPI); (c) the Beck Depression Scale-II (BDI-II); (d) the Beck Suicidal Ideation Inventory (Portuguese adaptation of the BSI); (e) the Beck Hopelessness Scale (Portuguese version of the BHS) and (f) the Pain Coping Questionnaire (Portuguese version of the Cuestionario de Afrontamiento del Pain - Reducido (CAD-R). The Pain Scale was occasionally used to assess Mrs. T's clinical situation.
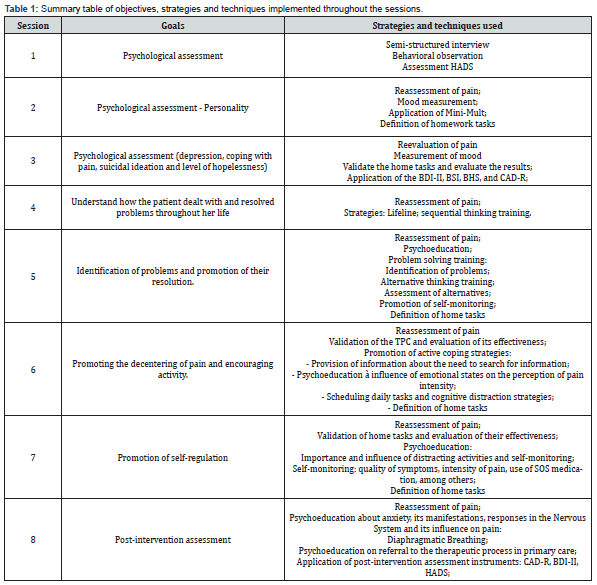
The patient signed an informed consent, declaring that she understood and authorized the use of her case to carry out a case study. Table 1 systematically presents the organization of the sessions, indicating their objective, as well as the strategies and techniques used. The main intervention objective was to promote active coping strategies, defining, therefore, specific objectives to develop (a) the understanding of cognitive representations for the maintenance of pain, (b) problem-solving, (c) the search for information and (d) the decentering of pain.
Results of Psychological Assessment and Intervention CBT - Mrs. T
Psychological Assessment
The psychological assessment process took place over three sessions, the first being for the clinical interview and the following two for the application of the previously mentioned formal instruments. Through the data collected through the interview, the patient presented complaints of pain in her left foot, which she classified as very strong pain that had lasted for around 1 year and classified on the Pain Scale as an 8 (severe pain). She had previously been medicated with Pregabalin and Dolocalma for SOS, and it was found that due to a lack of information/explanation, the patient did not comply with the SOS dosage in the appropriate way for her case.
When we learn about her clinical history, we also know the indication of two new diagnoses, namely Epilepsy with some past convulsive episodes and a psychodiagnosis of Chronic Depression, for which the patient has been medicated with Escitalopram for several years. The clinical history also includes three previous suicide attempts without consequent psychiatric hospitalizations. In view of these results, an evaluation was requested by the CMM Dor psychiatry - Dr. Rui Silva and the BSI and BHS were applied in order to assess the presence of suicidal ideation and current hopelessness.
In the cognitive/emotional domain, she presents discomfort related to the pain that seems to cause her to maintain her self-perception as a "poor thing," given the limitations that the pain causes. In the emotional dimension, the results indicate a state of lability, mostly characterized by depression, irritability and moments of anxiety and impatience. These states often intensify the pain felt and lead to the adoption of coping strategies such as escape and avoidance (e.g., avoiding going to the cafe because someone looks at her as a "poor thing," and consequently, the patient becomes irritated by this).
Additionally, it was also possible to learn that the patient is unemployed and receives only income from insertion. At the family level, there is a secure family support network. In the behavioral domain, Mrs. T. indicated the suspension of professional activities due to the emergence of pain and the tendency not to verbalize the pain. With regard to sleep hygiene and nutrition, restful nights and a normal diet were mentioned. In addition to the interview, the data collected through behavioral observation validated the pain picture, as she walked with some limitations and was accompanied by a crutch. The patient's expectations regarding psychological intervention were determined, and she revealed confidence in the process and hope for improvement. Understanding her expectations was essential because, in patients with chronic pain, it is common to create expectations that are either very high or very low, which in practice constitute obstacles to intervention. Expectations must be adjusted, clarifying that the objectives of intervention are not the total elimination of pain but the patient's adjustment to their pain, helping them to deal with it and face it (Hanson & Gerber, 1990), [1]. The formal results of the evaluation are presented in Table 2 & Figure 1.

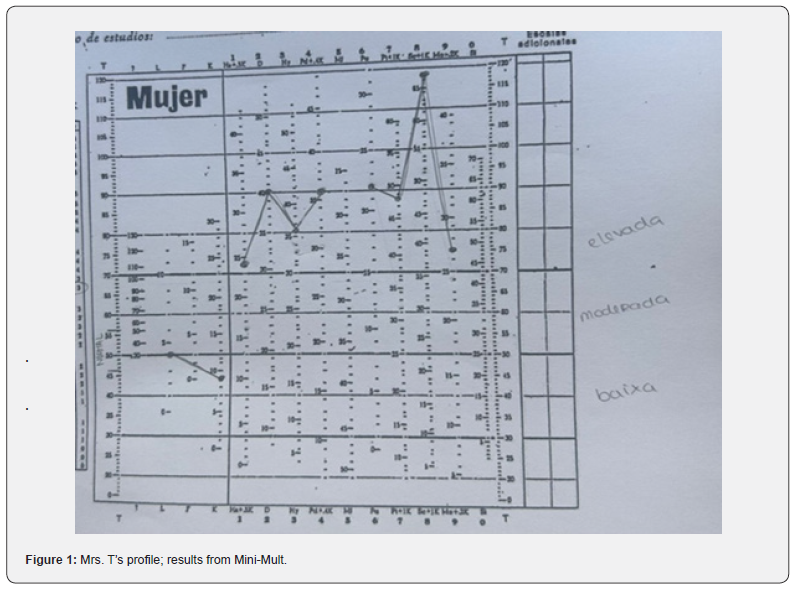
The results obtained from the applied instruments indicate a significant depressive condition that validates the psychodiagnosis and reveals a clinically significant dimension based on the HADS (13) and BDI-II (40) values [16] (Pais-Ribeiro et al., 2001; Silva et al., 2006). The BHS and BSI instruments were intended to measure the patient's suicidal ideation. Despite its existence, there seems to be no intentionality since there are no prepared plans, a chosen method or future measures in the face of its absence [14]. In turn, the Mini-Mult provided relevant data regarding patient T.'s personality, creating an above-average profile in all parameters. Of these, the dimensions of depression, paranoia and schizophrenia stand out. Patients with this profile are normally characterized as pessimistic people, with feelings of worthlessness and a lack of confidence, adopting behaviors closely linked to emotions and which consequently imply dependence due to little confidence in themselves [18]. Finally, the Pain Coping Questionnaire highlights a tendency to invest in passive coping strategies that result in the patient not obtaining significant results in managing their pain [12].
The Intervention - TCC
The psychological intervention took place in five sessions, based on the needs observed and presented by the patient and the results of the Pain Coping Questionnaire, considering the patient's abilities and priorities for pain management.
In the fourth session, the objective was to strengthen the therapeutic relationship with the patient and better understand her life story. We sought to understand how Mrs. T. dealt with stressful events throughout her life, collecting information about her adaptive response patterns and family history through lifeline strategies and thinking training. Sequential. Seven moments reported by the patient can be highlighted, and the significant moments identified concern Mrs. T.'s marriage and the birth of her children. On the other hand, the most difficult moments reported concern a history of abuse by the father and neglect by the mother throughout childhood and adolescence. She also reports experiences of physical violence (e.g., being attacked with canes, belts and hoses) and psychological violence (e.g., being told that the devil would take her). An equally remarkable episode described was the rape by the father and the onset of depression and subsequent suicide attempts. In the face of stressful events, the patient identifies feelings such as anger, hatred, hurt and revolt accompanied by escape and avoidance behaviors. Currently, the patient identifies that when faced with stressful situations, she tends to react anxiously and impulsively in an attempt to prevent problems from progressing. At the end of this session, we were asked to identify personal skills that Mrs. T. considered herself to have and which she stood out as hope and motivation for change. Based on the influences of Positive Psychology, it is understood that the focus on positive characteristics of individuals, of which hope, and optimism are highlighted, allows them to recognize positive experiences that favor their well-being and seek to adaptively face the problems algic conditions [22].
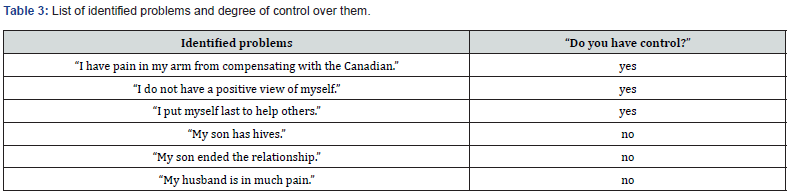
In the fifth session, the main objective was to promote problem-solving. When measuring the patient's mood at the beginning of the session, a state of agitation was observed, identified as a consequence of the worsening of her pain and a set of problems that were disturbing her. Given the problem presented to her, the intervention began with a psychoeducational moment on the cognitive model of CBT and the concepts of the cognitive triad. Through the information provided, the patient understood how maintaining dysfunctional thoughts and beliefs influences emotional and behavioral responses to pain. Framing the problem presented by the patient, a problem-solving training exercise was carried out, where she listed the problems that were troubling her at the moment (Table 3). Of these, each problem was evaluated in relation to its priority, probability of occurrence and level of control. Hence, Mrs. T. recognized as a priority the problems associated with her painful condition (e.g., "I have a strong and persistent pain in my arm because of the crutch”) since these were the most stressful and under his control. For the chosen problem, the patient reflected on possible alternatives and listed them, and TPC was defined as evaluating the proposed alternatives and choosing one of them to apply.
Additionally, she should replicate this process to other problems. The importance of patient self-monitoring was also reinforced, trying to be aware of the intensity of this new pain and its quality over time. We sought to help the patient identify problems and understand them as solvable, allowing her to find alternative solutions and put them into practice [1]. By internalizing this process, it was intended that the patient would be able to replicate it in the face of problematic situations arising from the pain, moving away from behavioral reactions such as escape, hopelessness and anxiety [1]. Problem-solving training is useful for Mrs. T. as she tends to fall into depressive and anxious states when faced with worsening pain and the problems that arise, whether or not resulting from it (e.g., inactivity, daily changes, emotional reactions), which often intensify the pain felt. "Learning to deal with illness and pain often requires learning to accept changes, which implies de-problematizing and looking for appropriate ways of thinking and acting on these situations and events that initially cause stress” (Rocha and Nunes, 1994), cited in [1], p.38).
The main objective of the sixth session was to promote the decentering of pain and encourage physical activity. When validating the TPC and measuring its effectiveness, the patient reported positive results, stating that it helped her identify aspects to improve, as well as presenting some examples of applied solutions, such as using the second crutch to relieve pain in her arm and distance herself from problems. Her husband and children, thus creating space for them to take responsibility and for her to be able to dedicate more time to herself. In view of the positive results, information was provided, namely about the importance of seeking medical help in the face of acute pain, such as going to the emergency room, as the patient tends not to seek medical information and endure the pain. The aim was to motivate the patient to act autonomously to face her situation, seeking greater well-being and quality of life through personal initiatives [23].
The session also included a psychoeducational moment on the influence of emotional states on the perception of pain and how it changes in the face of distracting stimuli. Thus, a brief explanation was made about how attentional processes and somatic perception work and how we can control it if we are aware of it. Between the different sessions, it was suggested to maintain the initially defined TPC, namely walking for at least 10 minutes on a floor that is comfortable for the patient, aiming to encourage her physical activity as a pleasurable task and allowing her to focus on her symptoms. Algic. Given the positive reports of a feeling of pain relief and increased well-being in relation to this task, a plan of daily tasks to be carried out was collaboratively drawn up (Table 4). The plan was defined considering activities that were pleasurable for the patient (e.g., going to the cafe, taking care of flowers, doing household chores, walking, reading and watching television and going swimming) and that represented activities that promoted a sense of individual capacity and returned some internal locus of control to it. These tasks would be carried out at times favorable to the patient and with flexibility for changes.
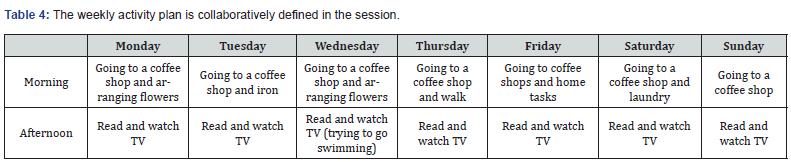
Note: The table presents the daily task plan created collaboratively with the patient, including pleasurable activities scheduled at times favorable to the patient.
For this specific case, programming daily activities represents an intervention strategy for the deconditioning presented in the psychological assessment, namely the loss of activity and inability to carry out pleasurable daily tasks, resulting in feelings of uselessness and lack of motivation to face the pain. This strategy that facilitates the individual's functionality intervenes in the quality of the behaviors adopted and aims to identify obstacles and face them in order to maintain active and adaptive behavior to the pain situation [1]. The flexibility of changing the schedule also allows the patient to manage individually and autonomously to carry out tasks according to their pain experience. Cognitive distraction strategies are combined with this activity since the patient's involvement in pleasurable activities redirects her attention. Through these activities, the patient redirects her attention to herself and moves away from unpleasant stimuli, reducing the perception of pain (Hanson & Gerberm 1990, cited in [1]. As a way of understanding the changes resulting from carrying out the task, the patient was asked as a TPC to follow the plan and record her thoughts and feelings afterward.
In the seventh session, clinical observation shows positive results, namely the patient's arrival in a good mood and without the assistance of the Canadian for mobilization. Through validating the TPC and measuring its effectiveness, it was understood that the tasks positively reinforced the patient, reassigning her some activity and sense of capacity, effectively diverting attention from pain symptoms during activities. Additionally, she has put forward efforts and plans to add swimming to the plan, with the belief that it will be beneficial for the pain. However, the patient reported that she did not reflect on her thoughts and feelings regarding the activity, justifying that writing takes her back to physical punishment during her childhood when she made spelling mistakes and that the consequent activation of memories triggered negative emotional states. Exercises that involve writing can be extremely beneficial for some individuals, facilitating the meaning and representation of situations through the promotion of insight, but for individuals with a tendency to ruminate thoughts, this exercise, especially if connected to a stressful event, leads to exacerbation of this tendency and the inhibition of adaptive coping (Cameron & Nicholls, 1998) cited in [24].
As a result, we suspended the writing exercises, as they do not constitute a therapeutic means for patient T. The focus of this session was the promotion of the patient's self-regulation, aiming to promote a more active attitude in managing her pain. It began with a psychoeducational moment, showing the relevance of self-monitoring and its consequences in pain intervention, namely greater self-knowledge in individual management, identification and response to pain symptoms and cooperation with the hospital team that accompanies her. To better understand the task, an exercise was carried out during the session, in which the patient was asked to classify the quality of her pain (e.g., if it was an acute pain without burning, grinding), its intensity and the number of times she used SOS medication per day, so that Mrs. T. understood which aspects needed to be more attentive in order to gain self-knowledge and better regularization.
The patient collaborated in the pre-and post-intervention reflective exercise, identifying an initial intensity of 8 and a current intensity of 4. Thus, it was established as TPC that the patient continued to perform distraction tasks and carried out self-monitoring. We sought to encourage their self-regulation, requiring them to carry out self-observation and supervision regarding behaviors associated with their health and, consequently, with stimuli and cognitive representations that influence pain conditions. It is expected that the patient will come to understand her body and mind as well as the way in which her behaviors and cognitions enhance or mitigate pain symptoms [1,23].
In the 8th and final session, the patient expressed some issues associated with anxiety that was clarified through a psychoeducational approach to the topic, namely with the framing of the symptoms presented (i.e., tightness in the chest and difficulty in breathing) in the manifestation of anxiety in the face of motor situation of this reaction. It was explained about the influence of stressful situations and the development of anxious reactions to the behavioral response emitted by the human central nervous system and, consequently, on the pain experience. Diaphragmatic breathing training was also carried out several times in a training format with Mrs T., with the aim of using it herself in similar situations outside the therapeutic space. The objective of this session was to clarify doubts about medication and pain control and carry out the post-intervention psychological assessment. Instruments such as the HADS, the Pain Coping Questionnaire and the BDI-II were applied again. The results obtained are compared with the initial (pre) values in Table 5, and a clear improvement is observed in several aspects.
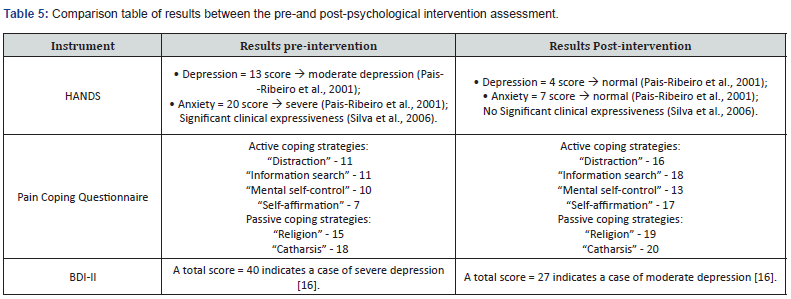
Note: The table presents the results obtained from the application of the HADS instruments, Pain Coping Questionnaire and BDI-II, in the preand post-psychological intervention phases
Psychometric results reveal a decrease in signs of anxiety and depression associated with pain, with a reduction in the HADS score. Similarly, the BDI-II reveals a lower score compared to that obtained in the initial assessment, indicating that the patient has achieved an improvement associated with her depressive condition. The Pain Coping Questionnaire provides data that shows an increase in the adoption of active strategies, especially distraction, information seeking and self-affirmation. Although most of the data measured by the instrument shows an increase, the most significant differences are found in active strategies, with the exception of mental self-control.
To conclude the intervention, it was suggested that the patient request psychological support at the health center in her parish, presenting her with the possibility of working on themes linked to past events and other relevant issues to obtain a greater quality of life and well-being, if she sees it as being better for her. To this end, the necessary steps were explained, and a positive response was obtained. Despite the psychological intervention ending, the patient committed to maintaining the strategies learned and seeking psychological support at CMM Dor - Dr. Rui Silva if necessary.
Discussion & Conclusion
Considering the objectives established for psychological intervention in this case, benefits and aspects to consider in the future are highlighted. The results obtained from the initial interview and the psychological assessment instruments directed the intervention towards promoting active coping strategies that Mrs. T. tended to avoid, such as distraction, information seeking and mental self-control. Although self-affirmation is one of the strategies least punctuated and validated in sessions, the intervention faced some obstacles. For this reason, maintaining investment in distracting tasks, searching for information, and self-monitoring exercises combined with promoting the ability to identify and manage problems were assumed to be beneficial objectives and strategies for the patient. Consider that, initially, the patient described pain that was strongly influenced by problems/situations in her family and by her focus on pain, limiting her day-to-day life in order to avoid acute pain. In this way, endowed with a greater capacity to respond to problems; to decentralize them and the symptoms, the patient reduces the perception of pain intensity and regains some functioning and control in her life.
However, it should be noted that throughout the intervention, it was understood that Mrs. T. had difficulty carrying out reflective and writing exercises, verifying the association with childhood trauma. Due to this factor, the exercises proposed in this context could have been more successful. Therefore, it was suggested that the patient undergo psychotherapeutic follow-up at the health center in her home, where she could work on these aspects. It is believed that, in its follow-up, better conditions will be met, that is, a greater capacity and openness of the patient to carry out cognitive tasks, such as cognitive restructuring exercises, which are considered to be relevant to her.
Even so, considering the limitations presented, the patient revealed motivation and adopted a collaborative stance, and the results obtained from the post-intervention evaluation reveal a considerable increase in the investment of active coping strategies, as intended, and a decrease in depressive and anxiety visible through the HADS and BDI-II. Considering the cognitive scope of this intervention, the use of psychoeducation on the cognitive processes behind each task has been relevant, as well as framing the results obtained from the TPC. Faced with this, Mrs. T. maintained a collaborative attitude and integrated the information, seeking to understand and get involved in the proposed behavioral tasks.
References
- Gomes A (2008) Abordagem psicológica no controlo da dor. Permanyer Portugal.
- Kreling MCGD, Cruz D de ALM da, Pimenta CA de M (2006) Prevalência de dor crônica em adultos. Revista Brasileira de Enfermagem 59(4): 509-513.
- Papalia DE, Feldman RD (2013) Desenvolvimento Humano (12th) AMGH Editora Ltda.
- Ray O (2004) How the mind hurts and heals the body. American Psychologist 59(1): 29-40.
- Richman LS, Kubzansky L, Maselko J, Kawachi I, Choo P, et al. (2005) Positive emotion and health: Going beyond the negative. Health Psychol 24(4): 422-429.
- Jensen MP, Turner JA, Romano JM (2001) Changes in beliefs, catastrophizing, and coping are associated with improvement in multidisciplinary pain treatment. J Consulting Clin Psychol 69(4): 655-662.
- Feliciano MFC, Parra CR (2011) Aliança terapêutica e resultados: Estudos de caso clínico em psicoterapia cognitivo comportamental.
- Poisk CC, Ramos DF, Amaral E (2023) Pressupostos básicos da terapia cognitivo-comportamental na prática clí In Psicologia Contemporânea: Práticas e abordagens clínicas em pesquisa. Editora Científica Digital p. 64-75.
- Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6): 361-370.
- Pais-Ribeiro J, Silva I, Ferreira T, Martins A, Meneses R, et al. (2007) Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol Health Med 12(2): 225-237.
- Soriano J, Monsalve V (2002) CAD: Cuestionario de Afrontamiento ante el Dolor Cró Revista de La Sociedad Espanhola Del Dolor 9(1): 13-22.
- Dias ARP (2006) Coping e qualidade de vida na dor crónica [Dissertação de Mestrado, Universidade de Valencia].
- Beck A, Kovacs M, Weissman A (1979) Assessment of suicidal intention: The Scale for Suicidal Ideation. J Consulting Clin Psychol 47(2): 343-352.
- Cunha JA (2001/2016) Manual da versão em português das Escalas Beck. Casa do Psicó
- Beck AT, Steer RA, Brown GK (1996) Manual for the Beck Depression Inventory-II. Psychological Corporation.
- Martins A (2000) As manifestações clínicas da depressão na adolescência [Clinical manifestations of fepression in adolescence] [Dissertação de mestrado, Universidade do Porto].
- Kincannon JC (1968) Prediction of the standard MMPI scale scores from 71 items: The Mini-Mult. J Consulting and Clin Psychol 32(3): 319-325.
- Cunha JA (2007) Psicodiagnóstico-V (5th edn). Artmed.
- Beck A, Weissman A, Lester D, Trexler L (1974) The measurement of pessimism: the hopelessness scale. J Consulting and Clin Psychol 42(6): 861-865.
- Klonsky E, Kotov R, Bakst S, Rabinowitz J, Bromet E (2012) Hopelessness as a predictor of attempted suicide among first admission patients with psychosis: A 10-year cohort study. Suicide Life Threat Behav 42(1): 1-10.
- Cruz JP (2000) Terapia cognitiva de los intentos de cuicidio - Cambiando historias de muerte por historias de vida. [Tese de Doutoramento não publicada, Faculdade de Psicologia de Sevilla].
- Scorsolini-Comin F (2017) Aconselhamento psicológico e psicologia positiva na saúde pública: Escuta como produção de saú Barbarói 2(50): 280-295.
- Joyce-Moniz L, Barros L (2005) Psicologia da doença para cuidados de saú Edições Asa.
- Figueiras MJ, Marcelino D (2012) Escrita terapêutica em contexto de saúde: Uma breve revisã Análise Psicológica 26(2): 327-334.






























