- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
A Concept Using a Staged and Standardized Ortho biologic Therapy for Cartilage Degeneration and Associated Inflammation of the Knee – The Avancell Joint Repair - Algorithm
Patrick Weninger*, Angelika Reich and Murat Özcelik
Avancell Medical, Liechtensteinstrasse 96, 1090 Vienna, Austria
Submission: January 09, 2024; Published: January 17, 2024
*Corresponding author: Patrick Weninger, Avancell Medical, Liechtensteinstrasse 96, 1090 Vienna, Austria
How to cite this article: Patrick Weninger*, Angelika Reich and Murat Özcelik. A Concept Using a Staged and Standardized Ortho biologic Therapy for Cartilage Degeneration and Associated Inflammation of the Knee – The Avancell Joint Repair - Algorithm. Ortho & Rheum Open Access J. 2024; 22(5): 556096. DOI: 10.19080/OROAJ.2024.22.556096
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Abstract
Osteoarthritis (OA) is a frequent and disabling disease. It causes pain, swelling and impaired joint function. All of this is caused by chronic inflammation of the joints affected. During the last decade, sophisticated minimally-invasive Ortho biologic strategies have emerged to treat patients with severe cartilage damage and OA. These strategies include intra-articular administration of platelet-rich plasma (PRP), injection of adipose-derived or bone-marrow derived stem cells and /or their supernatants and pain reduction by using selective denervation around the joint. All the mentioned techniques seem promising but so far, no treatment standards are available based upon results or experience. Based upon our experience and because of specializing in the field of joint preservation, we here present a standardized and staged algorithm for treating patients with cartilage damage and OA.
Keywords: Pain therapy; Cartilage defects; Chondrotoxic cytokines; Bone Marrow edema; Adipose-derived Stem Cells
Abbreviations: OA: Osteoarthritis; PRP: Platelet-Rich Plasma; MRI: Magnetic Resonance Imaging; ACS: Autologous Conditioned Serum; PDE: Platelet-derived exosomes; HA: hyaluronic acid; PDE: Platelet-Derived Exosomes; SVF: Stromal Vascular Fraction; BMSC: Bone Marrow derived Stem Cells; RF: Radio Frequency
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Introduction
The normal ageing process is associated with tissue degeneration and loss of tissue texture due to cell death, loss of water and loss of interstitial tissue such as collagen or elastic tissue components [1]. These tissue ageing processes also happen in joints where the cartilage is the most exposed and vulnerable component [2]. Not only normal ageing but also trauma, metabolic or auto-immune diseases or nutritional factors may contribute to cartilage tear and wear and associated osteoarthritis (OA) [3,4]. OA is the most common orthopedic reason for knee and hip pain but also affects other joints [5]. OA is associated with pain, joint swelling and limited range of motion leading to impaired joint function [6]. It is commonly accepted that OA starts a cascade of cellular and non-cellular reactions ending in a pathway of inflammation and joint destruction [7]. Cartilage damage can be treated operatively or non-operatively. Non-operative treatment includes analgetic medication, intra-articular injections, physical therapy, physiotherapy, chiropractic or osteopathy and others, all of them reducing pain symptoms associated with inflammatory response to cartilage damage [8-10]. Operative treatment includes arthroscopic cartilage surgery, such as autologous matrix-associated cartilage transplantation, microfractures, mosaicplasty or recently described single-stage cartilage transfers [11-13]. Also, osteotomies are possible procedures if the alignment needs correction in the lower extremities [14]. In cases of severe high-grade OA, joint replacement is the generally recommended surgical method [15]. Alone in the United States, annually more than 1.2 million joint replacements are performed, and numbers are expected to further rise [16]. As with every surgical method, arthroplasty also has its own risk profile. This includes surgical site infection, nerve damage, bleeding or thrombo-embolic complications, complications related to anesthesia, periprosthetic fractures or loosening of hardware components [17-19]. All in all, joint replacement is a relatively invasive operation with a high-risk profile for severe complications and unfavorable outcomes. During the last decade, sophisticated minimally-invasive Ortho biologic strategies have emerged to treat patients with severe cartilage damage and OA. These strategies include intra-articular administration of plateletrich plasma (PRP), injection of adipose-derived or bone-marrow derived stem cells and /or their supernatants and pain reduction by using selective denervation around the joint [20-23]. All the mentioned techniques seem promising but so far, no treatment standards are available based upon results or experience. Recently, the technique of joint preservation by using stem cellrich fat and radiofrequency ablation was described by Weninger et al. [24]. Based upon our experience and because of specializing in the field of joint preservation, we here present a standardized and staged algorithm for treating patients with cartilage damage and OA.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Stages of Cartilage Damage and Treatment Protocol
Cartilage damage was assessed by magnetic resonance imaging (MRI) and clinical examination of our patients. In every patient an MRI not older than six months was assessed. We staged cartilage damage according to the following criteria:
i) Subjective pain (Visual Analogue Scale, VAS).
ii) Kellgren-Lawrence Grade I-IV.
iii) Presence / Absence of bone marrow edema.
iv) Presence / Absence of synovitis.
v) Presence / Absence of locking.
vi) Presence / Absence of meniscus tears.
vii) Presence / Absence of loose cartilage fragments.
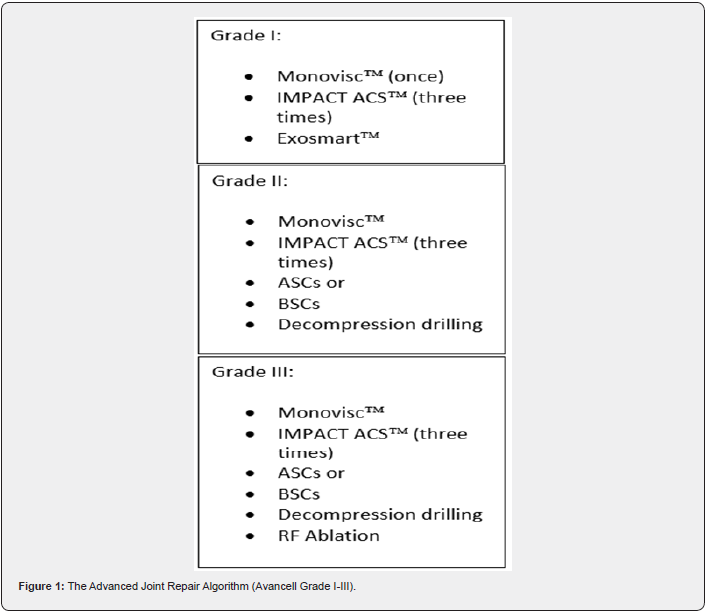
Based upon these examinations patients were allocated to our algorithm for joint preservation. First task was to identify patients needing arthroscopic surgery. Arthroscopy was performed in patients with locking, verified meniscus tears or loose cartilage fragments. These patients as well as patients who did not require arthroscopic surgery were further allocated to one of the three groups:
a. Avancell Grade I: Mild cartilage damage (Grade I/II) / mild effusion / mild synovitis, inflammation / VAS 0-3 / no or mild bone marrow edema.
b. Avancell Grade II: Moderate cartilage damage (Grade III) / moderate effusion / moderate synovitis, inflammation / VAS 4-6 / moderate bone marrow edema.
c. Avancell Grade III: Severe cartilage damage (Grade IV) / severe effusion / severe synovitis, inflammation / VAS > 6 / severe bone marrow edema.
For treatment options we used the spectrum of hyaluronic acid (HA) injections, platelet-rich-plasma (PRP), autologous conditioned plasma (ACS), bone marrow derived stem cells (BMSC), adipose-derived stem cells (ASCs) and radiofrequency (RF) ablation and minimally-invasive bone marrow edema decompression drilling.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Hyaluronic acid (HA)
In all patients, the damaged knee was prepared with one injection of 4mL hyaluronic acid (Monovisc) to reduce the inflammatory reaction. This is a high molecular weight hyaluronan visco-supplement that is used for single-shot administration.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Autologous Conditioned Serum (ACS)
After HA administration, 10mL whole blood were drawn from the cubital vein with a standard syringe using the IMPACT system (IMPACT , Haemo Concept, Austria). The syringe is filled with glass agglutinizing balls to start the coagulation process and to expand the surface. With this technique, the blood growth factors are activated mechanically even before centrifugation and release of anti-inflammatory cytokines from monocytes is initiated. In the next step, the sample was connected to another empty 10mL syringe and adjusted to the centrifuge. Then, the sample was centrifuged for another twenty minutes with 2,500 rounds to obtain the cell-free serum with the anti-inflammatory cytokines. The procedure was repeated three times, once a week.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Platelet-rich-plasma (PRP)
This was manufactured after the centrifuging process to obtain the BMSCs. By centrifuging 60mL bone marrow aspirate, 20mL PRP were processed and were available for injection.
We injected the PRP fraction immediately after injection of BMSCs.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Platelet-derived Exosomes (PDE)
40 mL whole blood were drawn from the cubital vein. Then, by using the Exosmart system, 10 mL of platelet-derived exosomes were produced by ultrafiltration through a microporous filtration membrane. The product was then isolated and transferred into a 10 mL syringe and injected into the knee under ultrasound guidance.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Bone Marrow-derived Stem Cells (BMSCs)
BMSCs were routinely used in relatively young patients aged under 70 years of age. To harvest the BMSCs we used a singleuse device for bone marrow aspiration under sterile conditions (SMART M-CELLÔ, Miracell, South Korea). The patient was placed in a prone position. Then, 20mL of Xylocaine 2% with Suprarenine 1:10,000 was used to numb the area of the spina iliaca posterior superior (soft tissues and periosteum). Then, the hollow aspiration cannula was advanced through the cortex into the cancellous bone. 60mL of bone marrow aspirate were harvested for further preparation. The bone marrow aspirate was centrifuged for seventeen minutes to process BMSCs and 20mL PRP out of it. Both components were then injected into the knee joint under ultrasound guidance.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Adipose-derived Stem Cells (ASCs)
ASCs were used in relatively older patients, aged over 70 years. The technique to harvest stem cell-rich fat graft was recently described by Weninger et al. [25]. After processing the stem cell-rich fat graft, 10 mL of it were injected into the knee joint under ultrasound guidance.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Radiofrequency (RF) Ablation
This procedure was performed by using cooled radiofrequency electrodes (Coolief Avanos, United States). The technique and the results were published recently by Weninger et al. [24]. With this technique, the genicular nerve branches around the knee are selectively denervated. The procedure was performed in local anesthesia (Xylocaine 2% with Suprarenine 1:10,000, 10mL at each of the genicular nerves) and all four genicular nerves were blocked.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Bone Marrow Edema drilling
In case of moderate and severe bone marrow edema, this edema was treated by retrograde drilling. The region of the bone marrow edema was identified on the MRI scan before and then was anesthetized (Xylocaine 2% with Suprarenine 1:10,000, 5mL). Then, a 1.6 mm drill pin was used on a universal power machine (Synthes, Switzerland) and the bone marrow edema was perforated according to the anatomic landmarks. Figure 1 shows the Advanced Joint Repair - Algorithm in detail.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Preliminary Results
With the here described protocol we treated 67 patients (41 of them female) within the past 12 months. 13 of them were allocated to Group I, 24 to Group II and 30 to Group III. Mean age was 57 years (range 46-87 years). 64 patients responded with pain relief within two weeks after the procedure. The other 3 individuals reported pain relief after more than two weeks. Mean VAS was reduced from 8.6 to 2.2 after a mean period of 15 days (range 1-36 days). All patients reported markable pain relief after four weeks. No patient reported pain increase or persisting pain level. Satisfaction rate was 100%. Every patient said, “I should have it done again” and “I should have done it earlier”. There were no serious adverse effects. 2 patients reported transient hematoma after fat graft or BSCs harvesting at the surgical site which dissolved after one week. Transient swelling of the knee occurred in 37 patients. There were no infections or bleeding complications. One patient had mild nausea after local anesthesia that also happened previously after dental treatment.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Discussion
It is generally accepted that OA of the knee causes a proinflammatory synovial environment and starts a release of chondrotoxic cytokines that further compromise the cartilage metabolism causing a vicious circle of chondrocyte damage [26]. Therefore, the aim of every regenerative approach to preserve the own cartilage and to reduce pain in OA must be to shift proinflammation to anti-inflammation. Cartilage regeneration and joint preservation with autologous material and Ortho biologic methods has emerged within the last decade. Besides HA, more biologic injectables have gained wide attention and became attractive therapeutic options. PRP was the first ortho biologic drug that gained attention in cartilage damage and OA treatment. In a recent meta-analysis, Filardo et al. found PRP to be superior to other injectables in terms of pain management and functional improvement in patients with knee OA [27]. The same results were reported by Tang et al. and Belk et al. who found superior results in patients undergoing treatment with PRP compared to HA alone [28,29]. ACS was introduced in the 1990-ies when the medical community was searching for a disease-modifying approach more than a symptom-treating one. Since then, it is known that ACS shifts the pro-inflammatory intra-articular surrounding to an anti-inflammatory. This shift is established through monocyte activation and release of various anti-inflammatory cytokines such as IL-1 receptor antagonist, IL-10 and TGF-B1 (which is elevated 7.9, 3 and 14.9 folds, respectively, in comparison to nonconditioned serum) [30-33].
The efficacy of ACS has been shown in different recent studies and meta-analyses. Recently, Coskun et al. found ACS to be more effective regarding pain reduction and outcome scores when compared to PRP [34]. In an animal model, Baykara et al. found ACS to increase fat viability more than PRP [35]. We therefore used ACS as a method to “prepare” the chronically irritated and inflammated knee (OA-associated synovitis) for further treatment with stem cell-rich fat graft or bone marrow aspirate. Exosomes are extracellular vehicles, approximately 30-150 nm in diameter and essential for cell-to-cell communication. They are secreted into the extracellular space and contain a diverse array of biological molecules, including nucleic acids, proteins, lipids and do not possess replicative capacity. These vehicles play a crucial role in various physiological processes, including tissue repair and inflammation [36]. In 2020 Kim et al. published a review article to report about the possibility to use mesenchymal stem cell-derived exosomes for cartilage repair in patients with OA [37]. In the present protocol, the administration of plateletderived exosomes (PDE) was chosen based upon their expected efficacy after in-vitro and in-vivo studies [38-40]. Zhang et al. showed that exosomes derived from PRP can enhance stem cell migration, promote chondrocyte regeneration and facilitate cartilage protection in mice with induced OA [39]. Same findings were reported by He et al, who concluded that bone marrowderived exosomes can effectively repair cartilage defects [41]. This is also in accordance with Ng et al. who described exosomes as a potent cell-free therapy to alleviate OA and osteochondral defects [42]. The use of adipose-derived stem cells from lipoaspirate has been described in numerous studies [43-45]. For our protocol we used a technique that was described recently [24,25]. Also, bone marrow aspirates as a source for mesenchymal stem cells and is used with promising results [46]. In a recent systematic review and meta-analysis, Bolia et al. compared stromal vascular fraction (SVF) and bone marrow aspirate injections about clinical and radiological improvement [47]. They found improved knee function after the one or the other. Nevertheless, they also highlighted the importance of a standardized protocol. They also reported a more than 50% complication rate in each group, a number that we cannot verify in our patients. For us, it was quite surprising that all the patients indicated decreased pain after the intervention and that satisfaction rate was 100%. That might be associated with the use of RF ablation in patients with severe OA. All the studies dealing with the topic of RF ablation for knee pain found significant pain reduction after the procedure. This is also in accordance with our results in patients with severe OA who underwent genicular nerve block with RF ablation. Most of our patients were allocated to Group III and had severe OA. Even in this subpopulation, a 100 % satisfaction rate was documented after the intervention. In our opinion also the decision to decompress bone marrow edema by retrograde core drilling is an important factor which is supported by current literature [48]. This is a simple and cheap pain-relieving treatment option that can be safely performed as an in-office procedure in local anesthesia.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
Conclusion
This is the first time, a standardized and staged protocol for cartilage regeneration and pain therapy is provided for patients with cartilage defects and OA of the knee. The herein described protocol seems to be safe and effective. Larger studies and longterm outcome measurements are needed to provide sufficient and reliable data in this context.
- Research Article
- Abstract
- Introduction
- Stages of Cartilage Damage and Treatment Protocol
- Hyaluronic acid (HA)
- Autologous Conditioned Serum (ACS)
- Platelet-rich-plasma (PRP)
- Platelet-derived Exosomes (PDE)
- Bone Marrow-derived Stem Cells (BMSCs)
- Adipose-derived Stem Cells (ASCs)
- Radiofrequency (RF) Ablation
- Bone Marrow Edema drilling
- Preliminary Results
- Discussion
- Conclusion
- References
References
- Palmer AK, Jensen MD (2022) Metabolic changes in aging humans: current evidence and therapeutic strategies. J Clin Invest 132(16): e158451.
- Sacitharan PK (2019) Ageing and osteoarthritis. Subcell Biochem 91: 123-159.
- Barnett R (2018) Osteoarthritis. Lancet 391(10134): 1985.
- Dieppe PA, Lohmander LS (2005) Pathogenesis and management of pain in osteoarthritis. Lancet 365(9463): 965-973.
- Long H, Liu Q, Yin H, Wang K, Naicheng D, et al. (2022) Prevalence trends of site-specific osteoarthritis from 1990 to 2019: Findings from the global burden of disease study 2019. Arthritis Rheumatol 74(7): 1172-1183.
- Glyn-Jones S, Palmer AJ, Agricola R, Price AJ, Vincent TL, et al. (2015) Osteoarthritis. Lancet 386(9991): 376-387.
- Sanchez-Lopez E, Coras R, Torres A, Nancy EL, Monica G (2022) Synovial inflammation in osteoarthritis progression. Naat Ver Rheumatol18(5): 258-275.
- Zhang Y, Yang H, He F (2022) Intra-articular injection choice for osteoarthritis: making sense of cell source – an updated systematic review and dual network meta-analysis. Arthritis Res Ther 24: 260.
- Migliorini F, Driessen A, Quack V, Nadja S, Brian C, et al. (2021) Comparison between intra-articular infiltrations of placebo, steroids, hyaluronic and PRP for knee osteoarthritis: a Bayesian network meta-analysis. Arch Orthop Trauma Surg 141(9): 1473-1490.
- Atalay SG, Durmus A, Gezginaslan Ö (2021) The effect of acupuncture and physiotherapy on patients with knee osteoarthritis: a randomized controlled study. Pain Physician 24(3): E269-E278.
- Richter DL, Schenck RC Jr, Wascher DC, Gehron T (2016) Knee articular cartilage repair and restoration techniques: a review of the literature. Sports Health 8(2): 153-160.
- Redondo ML, Naveen NB, Liu JN, Tracy MT, Taylor MS, et al. (2018) Preservation of knee articular cartilage. Sports Med Arthrosc Rev 26(4): e23-e30.
- Redondo ML, Beer AJ, Yanke AB (2018) Cartilage restoration: microfracture and osteochondral autograft transplantation. J Knee Surg 31(3): 231-238.
- Arner JW, Sherman SL, Strauss EJ, Armando FV, Rachel MF (2021) Joint preservation techniques for the knee in 2020: the utility of biologics, osteotomies, and cartilage restoration procedures. Instr Course Lect 70: 319-336.
- Gademan MG, Hofstede SN, Vliet Vlieland TP, Rob GHH Nelissen, Perla JM (2016) Indication criteria for total hip or knee arthroplasty in osteoarthritis: a state-of-the-science overview. BMC Musculoskeletal Disord 17(1): 463.
- Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005-2030. J Bone Joint Surg Am 89(4): 780-785.
- Healy WL, Della Valle CJ, Iorio R, Keith RB, Fred DC, et al. (2013) Complications of total knee arthroplasty: a standardized list and definitions of the Knee Society. Clin Orthop Relat Res 471(1): 215-220.
- Cheuy VA, Foran JRH, Paxton RJ et al. (2017) Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty 32(8): 2604-2611.
- Ji JH, Park SE, Song IS, Hanvit K, Ji Yoon Ha, et al. (2014) Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg 6(4): 365-372.
- Zhao J, Huang H, Liang G, Ling-Feng Z, Weiyi Y, et al. (2020) Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: a systematic review and meta-analysis. BMC Muskuloskelet Disord 21(1): 224.
- Ma Q, Liao J, Cai X (2018) Different sources of stem cells and their application in cartilage tissue engineering. Curr Stem Cell Res Ther 13(7): 568-575.
- Huang K, Li Q, Li Y, Zhihao Y, Daowen L, et al. (2018) Cartilage Tissue Regeneration: The roles of cells, stimulating factors and scaffolds. Curr Stem Cell Res Ther 13(7): 547-567.
- Conger A, Gililland J, Anderson L, Christiopher E Pelt, Christopher P, et al. (2021) Genicular nerve radiofrequency ablation for the treatment of painful knee osteoarthritis: current evidence and future directions. Pain Med 22(Suppl 1): S20-S23.
- Weninger P (2023) Joint preservation in patients with grade-IV osteo-arthritis of the knee - 12-months results after a multimodal approach using radiofrequency ablation and platelet-rich plasma supercharged stem cell-rich fat graft in 42 consecutive patients. J Surg 8: 1914.
- Weninger P, Feichtinger X, Steffel C, Celina K, Dominik D (2023) Arthroscopy with lipoaspirate and plasma infiltration using adipose-derived stem cells plus platelet-rich plasma: harvesting and injection for arthroscopic treatment of cartilage defects of the knee. Arthroscopy Techniques 12(12): e2265-e2271.
- Mathiessen A, Conaghan PG (2017) Synovitis in osteoarthritis: current understanding with therapeutic implications. Arthritis Res Ther 19(1): 18.
- Filardo G, Previtali D, Napoli F, Christian C, Stefano Z, et al. (2021) PRP injections for the treatment of knee osteoarthritis: a meta-analysis of randomized controlled trials. Cartilage 13(Suppl 1): 364S-375S.
- Tang JZ, Nie MJ, Zhao JZ, Guang Cheng Z, Qing Z, et al. (2020) Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. J Orthop Surg Res 15(1): 403.
- Belk JW, Kraeutler MJ, Houck DA, Darby AH, Jesse AG, et al. (2021) Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Am J Sports Med 49(1): 249-260.
- Raeissadat SA, Rayegani SM, Jafarian N, Mina H (2022) Autologous conditioned serum applications in the treatment of musculoskeletal diseases: a narrative review. Future Sci OA 8(2): FSO776.
- Rutgers M, Saris DB, Dhert WJ, Laura BC (2010) Cytokine profile of autologous conditioned serum for treatment of osteoarthritis, in vitro effects on cartilage metabolism and intra-articular levels after injection. Arthritis Res Ther 12(3): R114.
- Wehling P, Moser C, Frisbie D, Wayne MC, Christopher EK, et al. (2007) Autologous conditioned serum in the treatment of orthopedic diseases: orthokine therapy. BioDrugs 21(5): 323-332.
- Baltzer AW, Moser C, Jansen SA (2009) Autologous conditioned serum (Orthokine) is an effective treatment for knee osteoarthritis. Osteoarthritis Cartilage 17(2): 152-160.
- Coskun HS, Yurtbay A, Say F (2022) Platelet rich plasma versus autologous conditioned serum in osteoarthritis of the knee: clinical results in a five-year retrospective study. Cureus 14(4): e24500.
- Baykara G, Sungur N, Ozur K, Oguz A, Muzaffer C, et al. (2022) Autologous conditioned serum increases fat graft viability more than platelet-rich plasma in a controlled rat model. Plast Reconstr Surg 149(5): 1123-1136.
- Hade MD, Suire CN, Suo Z (2021) Mesenchymal stem cell-derived exosomes: applications in regenerative medicine. Cells 10: 1959.
- Kim YG, Choi J, Kim K (2020) Mesenchymal stem cell-derived exosomes for effective cartilage tissue repair and treatment of osteoarthritis. Biotechnol J 15(12): e2000082.
- Zhao H, Zhao Z, Li D, Wang X, Dehao D, et al. (2023) Effect study of exosomes derived from platelet-rich plasma in the treatment of knee cartilage defects in rats. J Orthop Surg Res 18(1): 160.
- Zhang Y, Wang X, Chen J, Dingfei Q, Peng G, et al. (2022) Exosomes derived from platelet-rich plasma administration in site mediate cartilage protection in subtalar osteoarthritis. J Nanobiotechnology 20(1): 56.
- Xu C, Mi Z, Dong Z, Xiaobo C, Gang Ji, et al. (2023) Platelet-derived exosomes alleviate knee osteoarthritis by attenuating cartilage degeneration and subchondral bone loss. Am J Sports Med 51(11): 2975-2985.
- He L, He T, Xing J, Qing Z, Lei F, et al. (2020) Bone marrow mesenchymal stem cell-derived exosomes protect cartilage damage and relieve knee osteoarthritis pain in a rat model of osteoarthritis. Stem Cell Res Ther 11: 276.
- Ng CY, Chai JY, Foo JB, Nor Hamdan MY, Ying Y, et al. (2021) Potential of exosomes as cell-free therapy in articular cartilage regeneration: A review. Int J Nanomedicine 16: 6749-6781.
- Romano IR, D’Angeli F, Vicario N, Cristina R, Carlo G, et al. (2023) Adipose-derived mesenchymal stromal cells: a tool for bone and cartilage repair. Biomedicines 11(7): 1781.
- Bielli A, Scioli MG, Gentile P, Valerio C, Augusto O (2016) Adipose-derived stem cells in cartilage regeneration: current perspectives. Regen Med 11(7): 693-703.
- Rahman G, Frazier TP, Gimble JM, Omair AM (2022) The emerging use of ASC/scaffold composites for the regeneration of osteochondral defects. Front Bioeng Biotechnol 10: 893992.
- Ding N, Lie E, Ouyang X, Jin G, Wei B (2021) The therapeutic potential of bone marrow mesenchymal stem cells for articular cartilage regeneration in osteoarthritis. Curr Stem Cell Res Ther 16(7): 840-847.
- Bolia IK, Bougioukli S, Hill WJ, Nicholas AT, Frank AP, et al. (2022) Clinical efficacy of bone marrow aspirate concentrate versus stromal vascular fraction injection in patients with knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med 50(5): 1451-1461.
- Littman J, Gil H, Aaron R (2023) Spontaneous bone marrow edema: perfusion abnormalities and treatment with surgical decompression. Int J Mol Sci 24(7): 6761.






























