How to Avoid knee Arthroplasty in Patients with Grade Iv Osteoarthritis – Combination of Adipose-Derived Stem Cells and Radiofrequency Ablation. A Case Series of 30 Consecutive Patients with 12-Months Follow-up
Patrick Weninger*
Avancell Medical, Liechtensteinstrasse 96 1090 Vienna, Austria
Submission: October 25, 2023; Published: November 06, 2023
*Corresponding author: Patrick Weninger, Avancell Medical, Liechtensteinstrasse 96 1090 Vienna, Austria
How to cite this article: Patrick Weninger*. How to Avoid knee Arthroplasty in Patients with Grade Iv Osteoarthritis – Combination of Adipose-Derived Stem Cells and Radiofrequency Ablation. A Case Series of 30 Consecutive Patients with 12-Months Follow-up. Ortho & Rheum Open Access J. 2023; 22(3): 556089. DOI: 10.19080/OROAJ.2023.22.556089
Abstract
Introduction: OA of the knee is a progressive disease that, to the best of our knowledge, cannot be stopped. There are conservative or operative treatment options for knee OA including intraarticular injections of cortisone, hyaluronic acid or platelet-rich-plasma (PRP). Joint replacement is the most common surgical procedure in patients with grade IV OA of the knee. As with every surgical procedure, KA has a risk profile of possible complications. In the present study, we report on thirty consecutive patients with grade IV knee OA who underwent treatment with stem-cell rich fat graft combined with radiofrequency (RF) ablation.
Material and Methods: We enrolled thirty consecutive individuals (mean age 64.5; range 57-92) with grade IV OA of the knee. There were 11 female and 19 male patients. All patients were treated between January and June 2022. Patients were consented for liposuction and knee liparthroplasty and for selective RF ablation (Coolief, Avanos Medical, USA) of the sensory branches of the genicular nerves. At follow-up, VAS, range of motion (ROM) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) were assessed. Furthermore, we assessed patients’ subjective satisfaction. Level of statistical significance was set at p < 0.05.
Results: At follow-up, no patient converted to KA. All patients attested they would have the procedure done again if necessary. VAS was significantly improved (p< 0.05) in all the patients. No patient had worse or equal VAS at follow-up. The Median ROM before the intervention was 0-2-130. Median ROM was 2-0-145 at follow-up. No patient showed worse ROM at follow-up. In all KOOS categories, significant improvement was shown at follow-up (p< 0.05). No patients showed worse or equal KOOS values at follow-up.
Conclusion: To the best of our knowledge, this is the first study reporting on ASC in combination with RF ablation in a population of patients with severe OA of the knee who already were scheduled for KA. According to our results, the herein described treatment regime appears to be safe and effective at twelve months follow-up.
Introduction
Worldwide, around 654.1 million (CI 565.6-745.6) individuals (forty years or older) suffered from osteoarthritis of the knee in the year 2020 [1,2]. People suffering from knee OA report pain, swelling, stiffness and limited range of motion [3,4]. Accordingly, OA of the knee is also a major burden for socio-economic structures of a system as it leads to loss of productivity of the population. The reasons for knee OA include normal cartilage ageing, knee trauma, joint infection, or metabolic disorders [5]. OA of the knee is a progressive disease that, to the best of our knowledge, cannot be stopped. There are conservative or operative treatment options for knee OA including intraarticular injections of cortisone, hyaluronic acid or platelet-rich-plasma (PRP) [6,7]. Operative options include arthroscopic debridement, microfractures, mosaicplasty, chondrocyte transplantation or partial or total knee arthroplasty (KA) [8-10]. Joint replacement is the most common surgical procedure in patients with grade IV OA of the knee. As with every surgical procedure, KA has a risk profile of possible complications. These include perioperative complications such as bleeding, nerve lesions or thromboembolic complications as well as postoperative complications such as infection, limited range of motion or persisting pain [11-13]. Recently, more regenerative strategies have been reported to be effective including the administration of adipose-derived stem cells (ACS) or bone-marrow stem cells (BMSC) for cartilage repair [14,15]. Radiofrequency (RF) ablation of the genicular nerves around the knee is a viable options for minimally invasive pain management and has been highlighted in various studies [16-18]. In the present study, we report on thirty consecutive patients with grade IV knee OA that were scheduled for KA before consulting our practice.
Material and Methods
We enrolled thirty consecutive individuals (mean age 64.5; range 57-92) with grade IV OA of the knee who were told that joint preservation would not be possible and who were scheduled for KA accordingly by other facilities. There were 11 female and 19 male patients. All patients were treated between January and June 2022. Patients were included if they had grade IV OA in at least two compartments of the knee (medial, lateral, patella-femoral). All patients had unilateral treatment.
Treatment protocol
Patients were consented for liposuction and knee liparthroplasty [19] and for selective RF ablation (Coolief, Avanos Medical, USA) of the sensory branches of the genicular nerves.
Radiofrequency Ablation
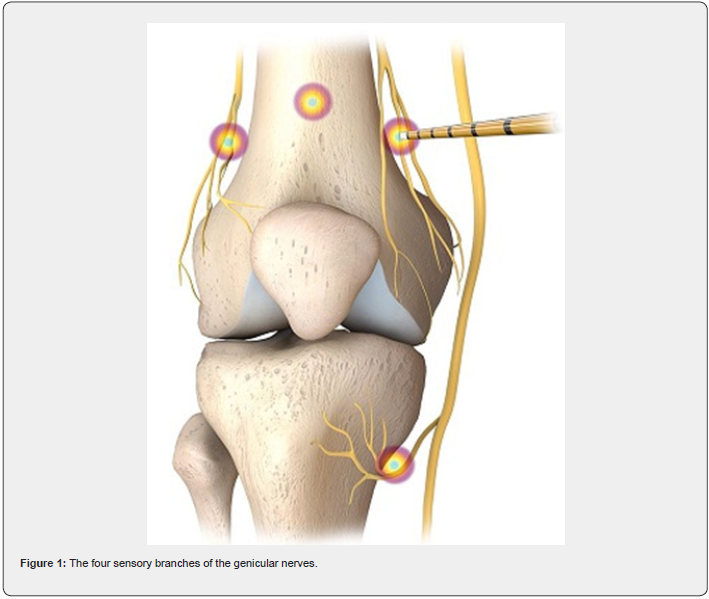
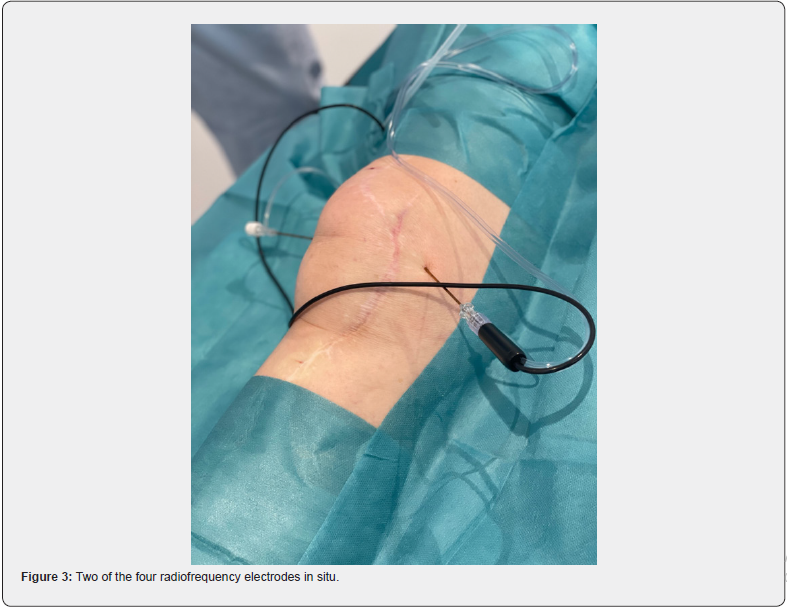
Patients were placed and prepared in supine position. Then, 10mL Lidocaine 2% with epinephrine 1:10.000 were injected at each of the four genicular nerve locations (Figure 1). After waiting for some minutes, ultrasound (Clarius HD, Canada) was used to identify the branches of the four genicular nerves. Then, the RF electrodes were placed on the four sensory branch locations (Figure 2). Then, the nerve branches were ablated by cooled RF ablation (maximum 63° Celsius, 100 Ohm impedance and 7 Watt for) for two minutes and thirty seconds in each location.
Adipose-derived stem cells
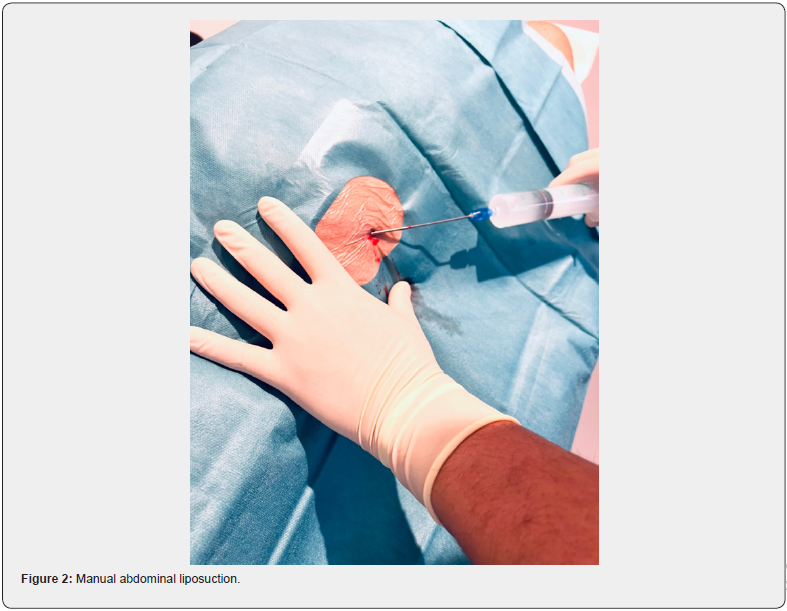
After RF ablation, the left abdominal region was prepared and draped for liposuction. Local anesthesia (1% lidocaine with epinephrine 1:10.000) was used to numb the area. A tumescent solution (250 mL of saline solution, 1 mL of 1:200,000 adrenalin, and 600 mg of lidocaine, 8.4% sodium-bicarbonate) was inserted over a little incision with a 100mL syringe. After some minutes of waiting, a manual liposuction was performed with a 20mL syringe and a 3mm liposuction cannula (Tulip Medical, USA) (Figure 3). We routinely used four 20mL syringes with fat-aspirate for further processing.
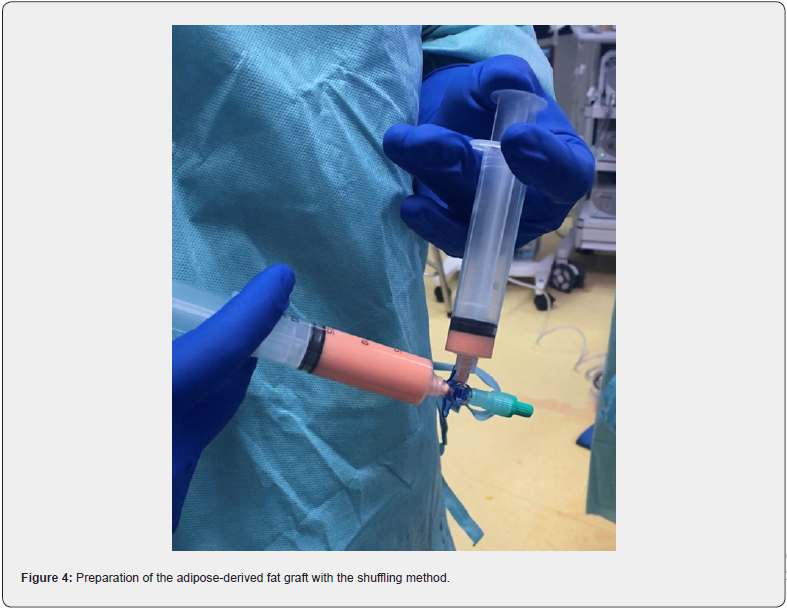
The fat fraction in each of the syringes was isolated and separated from the fluid and oil fraction by using the so-called decanting method without centrifuging the fat aspirate. This technique was described recently in past studies [20,21]. Then, we used the so-called shuffling method to mechanically shift the fat graft between two syringes. For this, a three-way-valve was used. By using this method, the membranes of the fat cells are ruptured manually, and the then more refined fat graft gets easier injectable (Figure 4). By an assistant 15mL venous whole blood was drawn from a cubital vein into a double chamber syringe (Arthrex, Naples, US). This double syringe and the whole-blood sample were subsequently centrifuged in a standard centrifuge (Rotofix 32 A, Hettich, Germany) with 1500 rounds for 5 minutes. By centrifugation, 5mL of PRP fraction was isolated and was then inserted into the syringe with the fat graft. The supercharged fat graft was then inserted into the knee joint by a single-use 20-gauge needle and by using the ultrasound-scanner to avoid insertion into Hoffa’s fat pad. Wounds were covered with plasters and patients were advised to fully bear weight as tolerated by pain. All patients were followed-up after six weeks in our office.
Study follow-up
All thirty individuals were followed-up after twelve months at least (12.0-14.2 months). At follow-up, VAS, range of motion (ROM) and the Knee Injury and Osteoarthritis Outcome Score (KOOS) were assessed. Furthermore, we assessed patients’ subjective satisfaction. For statistical analysis SPSS was used (SPSS, USA). Level of statistical significance was set at p < 0.05.
Results
We did not record any complications or any adverse effects after manual liposuction, fat injection or radiofrequency ablation. Three patients had mild hematoma at the liposuction site. One patient had quadriceps weakness that resolved the next day. Twenty-one patients had minimal or mild effusion of the knee. At follow-up, no patient has converted to KA. All patients attested they would have the procedure done again if necessary.
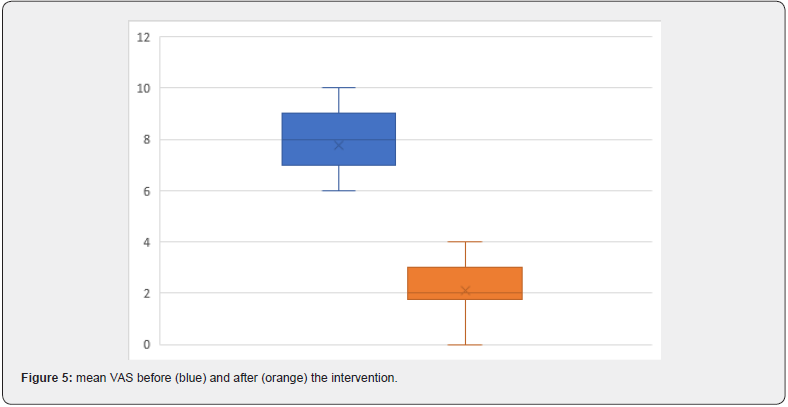
Visual Analogue Scale
Mean VAS before the intervention was 7.8 (range 6-10). At twelve-month follow-up, VAS was significantly improved (p< 0.05, Figure 5) in all the patients. No patient had worse or equal VAS at follow-up.
Range of Motion
The Median ROM before the intervention was 0-2-130. Median ROM was 2-0-145 at follow-up. No patient showed worse ROM at follow-up.
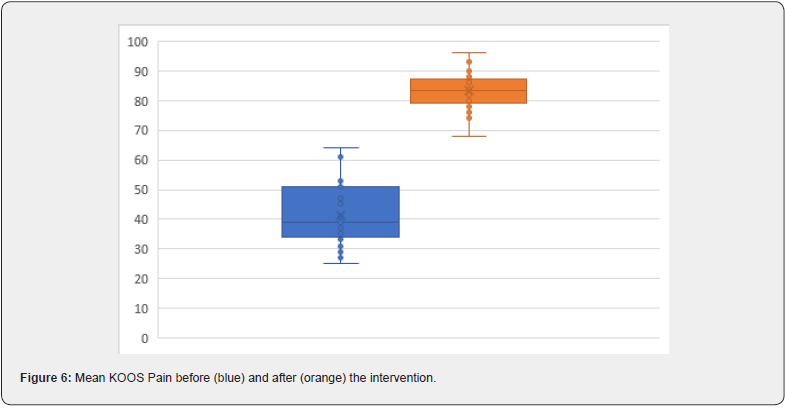
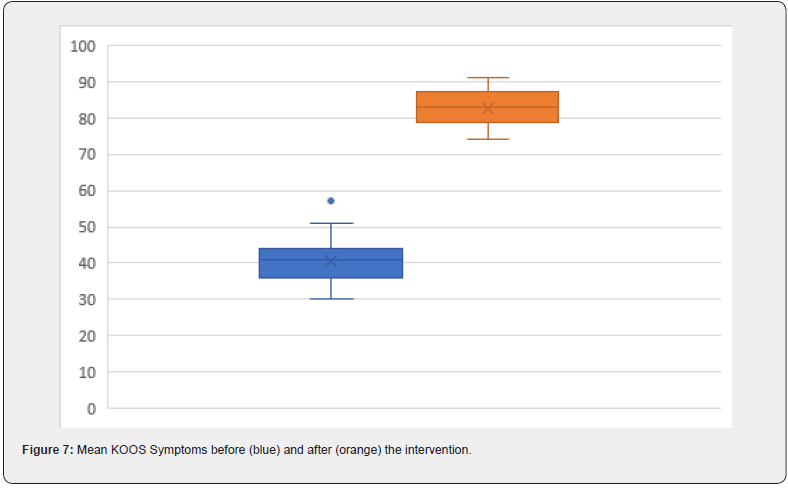
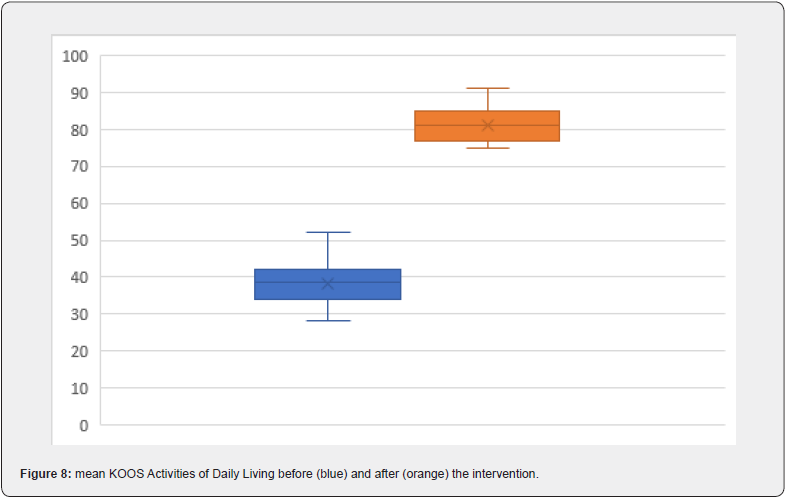
KOOS
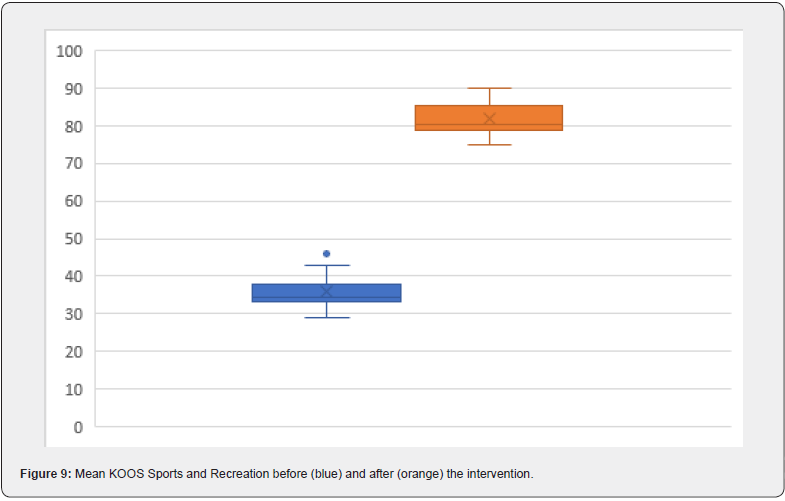
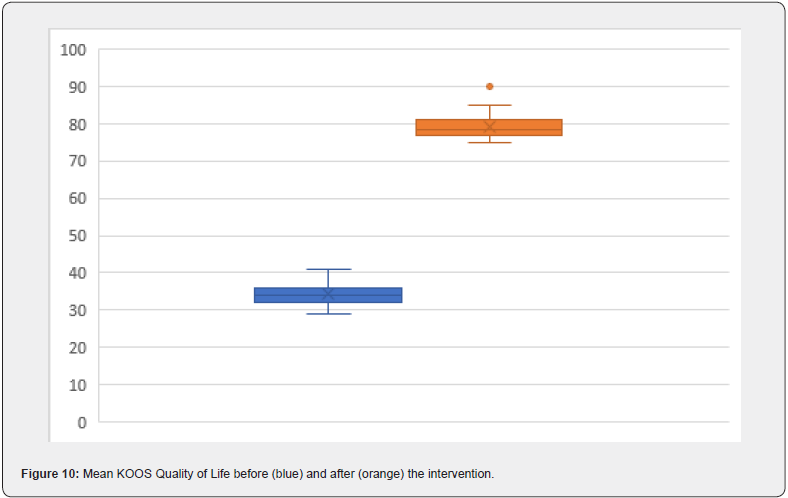
In all KOOS categories, significant improvement was shown at follow-up (p< 0.05; Figure 6-10). No patients showed worse or equal KOOS values at follow-up.
Discussion
The use of intraarticularly injectable substances to treat knee OA has been vastly described in the past [6,7]. Intraarticular administration of stem cell-rich fat grafts is relatively new and not a common practice, yet. Froschauer et al. published a study describing the results after liparthroplasty of the first carpometacarpal joint and the same group reported improved outcome scores after five years [20,21]. Jo et al. reported encouraging results after intraarticular injection of adipose-derived mesenchymal stem cells for the treatment of OA of the knee in a series of eighteen patients [22]. This is also in accordance with the publication of Lee et al. who found improved outcome after six months follow-up [23].
In a recent study by Kim et al., the authors showed cartilage regeneration visualized in magnetic resonance imaging (MRI) scans and significant pain relief in patients with knee OA after arthroscopic implantation of ASC [24]. Also, Lapuente et al. found improved clinical outcome after ASC injection and correlated this with ultrasound imaging and biochemical parameters by showing a marked decrease of pro-inflammatory molecules and a significant increase of anabolic and anti-inflammatory parameters [25]. Despite different non-surgical treatment options are available for patients with symptomatic knee OA, KA often still is the first-line treatment and recommended by most orthopedic surgeons. As already described in the Introduction section, complications that might be connected to the operation or to the post-operative period are inevitable. It also needs to be pointed out that KA hardware has limited duration and revision surgery has to be considered in younger patients. These revision surgeries are associated with higher morbidity and mortality compared to the index operation [26].
Resulting from extended life-expectancy and a subsequently resulting over-aged population, the incidence of knee OA is expected further to rise [1,2]. Also, the extended life-expectancy might lead to a population with higher rates of co-morbidities. This combination may lead to a dilemma in which relatively old and ill patients will undergo high-risk operations such as KA. Considering the recently ended SARS-CoV 2 pandemic with long waiting lists of cancelled operations, the here described technique might be of value to treat patients without the need for an operation. The protocol is used for in-office treatment without the need for highly sophisticated hospital infrastructure such as intensive care or blood bank. From a socio-economic point of view the here described regime combining ASC with RF ablation is cheaper than KA and might also be useful for patients in poorer countries or in countries with underdeveloped medical infrastructure. As shown in the here presented study, no adverse effects were found in our population that mainly included elderly patients. We also point out that symptom improvement and pain relief was found in every single patient. As a result, patient satisfaction was 100% at followup, which is very seldom in medicine.
Although high patient satisfaction and improved outcome parameters one has to be cautious when interpreting the results. We only have data of a small study population with twelvemonth follow-up. We cannot extrapolate to higher numbers or longer follow-up. Further, it is not clear what caused outcome improvement: ASC administration or RF ablation or both. In this context, we also need to highlight the study by Salzmann et al. who found improved symptoms in patients with knee OA even after administration of saline [27]. Therefore, further studies with longer observational periods seem necessary.
Conclusion
To the best of our knowledge, this is the first study reporting on ASC in combination with RF ablation in a population of patients with severe OA of the knee who already were scheduled for KA. According to our results, the herein described treatment regime appears to be safe and effective at twelve months follow-up.
References
- Cui A, Li H, Wang D, Junlong Zhong, Yufeng Chen, et al. (2022) Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. eClinical Medicine 29: 100857.
- Allen KD, Thoma LM, Golightly LM (2022) Epidemiology of osteoarthritis. Osteoarthritis Cartilage 30(2): 184-195.
- Altmann R, Asch E, Bloch D, G Bole, D Borenstein, et al. (1986) Development of criteria for the classification and reporting of osteoarthritis. Classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum 29(8): 1039-1049.
- Suri P, Morgenroth DC, Hunter DJ (2012) Epidemiology of osteoarthritis and associated comorbidities. PM R 4 (Suppl): S10-19.
- Palazzo C, Nguyen C, Lefevre-Colau MM, Francois Rannou, Serge Poiraudeau, et al. (2016) Risk factors and burden of osteoarthritis. Ann Phys Rehabil Med 59(3): 134-138.
- Zhao J, Huang H, Liang G, Ling-Feng Zeng, Weiyi Yang, et al. (2020) Effects and safety of the combination of platelet-rich plasma (PRP) and hyaluronic acid (HA) in the treatment of knee osteoarthritis: a systematic review and meta-analysis. BMC Muskuloskelet Disord 21(1): 224.
- MacFarlane LA, Mass H, Collins JE, Elena Losina, Jeffrey N Katz, et al. (2023) Response to intra-articular cortisone injections in knee osteoarthritis patients with and without effusion on ultrasound: a pilot study. Osteoarthr Cartil Open 5(2): 100361.
- Dekker TJ, Aman ZS, DePhillippo NN, Jonathan F Dickens, Adam W Anz, et al. (2021) Chondral lesions of the knee: an evidence-based approach. J Bone Joint Surg (Br) 103(7): 629-645.
- Calcei JG, Ray T, Sherman SL, Jack Farr (2020) Management of large focal chondral and osteochondral defects of the knee. J Knee Surg 33(12): 1187-1200.
- Trofa DP, Hong IS, Lopez CD, Allison J Rao, Ziqing Yu, et al. (2023) Isolated osteochondral autograft versus allograft transplantation fort he treatment of symptomatic cartilage lesions of the knee: a systematic review and meta-analysis. Am J Sports Med 51(3): 812-824.
- Healy WL, Della Valle CJ, Iorio R et al. (2013) Complications of total knee arthroplasty: a standardized list and definitions of the Knee Society. Clin Orthop Relat Res 471(1): 215-220.
- Cheuy VA, Foran JRH, Paxton RJ, Michael J Bade, Joseph A Zeni, et al. (2017) Arthrofibrosis associated with total knee arthroplasty. J Arthroplasty 32(8): 2604-2611.
- Ji JH, Park SE, Song IS, Hanvit Kang, Ji Yoon Ha, et al. (2014) Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg 6(4): 365-372.
- Ma Q, Liao J, Cai X (2018) Different sources of stem cells and their application in cartilage tissue engineering. Curr Stem Cell Res Ther 13(7): 568-575.
- Huang K, Li Q, Li Y, Zhihao Yao, Daowen Luo, et al. (2018) Cartilage Tissue Regeneration: The roles of cells, stimulating factors and scaffolds. Curr Stem Cell Res Ther 13(7): 547-567.
- Conger A, Gililland J, Anderson L, Christopher E Pelt, Christopher Peters, et al. (2021) Genicular nerve radiofrequency ablation for the treatment of painful knee osteoarthritis: current evidence and future directions. Pain Med 22 (Suppl 1): S20-S23.
- McCormick ZL, Cohen SP, Walega DR, Lynn Kohan (2021) Technical considerations for genicular nerve radiofrequency ablation: optimizing outcomes. Reg Anesth Pain Med 46(6): 518-523.
- Swanson JL (2023) Genicular nerve radiofrequency ablation. JAAPA 36(3): 32-36.
- Weninger P (2023) Joint preservation in patients with grade-IV osteo-arthritis of the knee – 12-months results after a multimodal approach using radiofrequency ablation and platelet-rich plasma supercharged stem cell-rich fat graft in 42 consecutive patients. J Surg 8: 1914.
- Froschauer SM, Holzbauer M, Wenny R, Manfred Schmidt, Georg M Huemer, et al. (2020) Autologous fat transplantation for thumb carpometacarpal joint osteoarthritis (liparthroplasty): a case series with two years follow-up. J Clin Med 10(1): 113.
- Holzbauer M, Schmidt M, Mihalic JA, Dominik Duscher, Stefan Mathias Froschauer, et al. (2022) Liparthroplasty for thumb carpometacarpal joint osteoarthritis: a case series with median 5 years follow-up. J Clin Med 11(21): 6411.
- Jo CH, Lee YG, Shin WH, Hyang Kim, Jee Won Chai, et al. (2014) Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells 32(5): 1254-1266.
- Lee WS, Kim HJ, Kim KI, Gi Beom Kim, Wook Jin, et al. (2019) Intra-articular injection of autologous adipose tissue-derived mesenchymal stem cells for the treatment of knee osteoarthritis: a phase IIb, randomized, placebo-controlled clinical trial. Stem Cells Transl Med 8(6): 504-511.
- Kim KI, Lee WS, Kim JH, Jung-Kwon Bae, Wook Jin, et al. (2022) Safety and efficacy of the intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritic knee: a 5-year follow-up study. Stem Cells Transl Med 11(6): 586-596.
- Lapuente JP, Dos-Anjos S, Blazquez-Martinez A (2020) Intra-articular infiltration of adipose-derived stromal vascular fraction cells slows the clinical progression of moderate-severe knee osteoarthritis: hypothesis on the regulatory role of intra-articular adipose tissue. J Orthop Surg Res 15 (1): 137.
- Berstock JR, Beswick AD, Lopez-Lopez JA, Michael R Whitehouse, Ashley W Blom, et al. (2018) Mortality after total knee arthroplasty: a systematic review of incidence, temporal trends, and risk factors. J Bone Joint Surg Am 100(12): 1064-1070.
- Saltzman BM, Leroux T, Meyer MA, Bryce A Basques, Jaskarndip Chahal,et al. (2017) The therapeutic effect of intra-articular normal saline injections for knee osteoarthritis: a meta-analysis of evidence level 1 studies. Am J Sports Med 45(11): 2647-2653.






























