The Effect of Schroth Exercises on Pulmonary Function in Adolescent Idiopathic Scoliosis
Hande Tunc1*, Hurriyet Yilmaz2 and Ahsen Buyukaslan2
1Kavacık Mah. Ekinciler Cad. No:19, Kavacık Kavsagi, 34810, Istanbul, Turkey
2Formed Healthcare Scoliosis Treatment and Brace Center, Halaskargazi Mah. Zafer Sok. No:28/A, Nisantası, Istanbul, Turkey
Submission:August 23, 2023; Published:October 31, 2023
*Corresponding author: Hande Tunc, Istanbul Medipol University, Department of Pysiotherapy and Rehabilitation, Kavacık Mah. Ekinciler Cad. No:19, Kavacık Kavsagi, 34810, Beykoz, Istanbul, Turkey
How to cite this article: Hande T, Hurriyet Y, Ahsen B. The Effect of Schroth Exercises on Pulmonary Function in Adolescent Idiopathic Scoliosis. Ortho & Rheum Open Access J. 2023; 22(3): 556087. DOI: 10.19080/OROAJ.2023.22.556087
Abstract
Background: Idiopathic scoliosis is a three-dimensional structural deformity and adolescent form is the most common type (AIS). Conservative treatment methods in AIS include brace and scoliosis-specific exercise treatments. Respiratory limitations have been reported in relation to the nature of scoliosis itself. However, the evidence regarding treatment interventions is controversial. The purpose of the study, to investigate the effects of Schroth exercises on pulmonary functions on adolescents who use rigid braces and perform Schroth exercises.
Method: Twenty-four patients with AIS were included in the study. The patients who wore brace and performed the SSE therapy constituted the “Brace & Exercise” (N=12), and the patients who wore full time brace but did not perform exercise constituted the “Brace’’ (N=12) group of the study. The effects of Schroth exercises on pulmonary functions were measured at the beginning of treatment and 8th week of the treatment.
Findings: At the beginning of the treatment, there were not found statistical differences in demographic data and pulmonary function values between Brace and Brace & Exercise groups. At 8th week of the treatment, there was an increase in the FEV1 parameter in the Brace & Exercise group. Also, at 8th week of treatment, there was found a strong negative correlation between brace using time – FVC and negative correlation between brace using time and FEV1 values (p <0.05).
Conclusion: It was determined that the use of full-time brace did not cause a statistical difference on respiratory values and Schroth exercises performed during treatment period could have a positive contribution on FEV1 value.
Keywords: Adolescent idiopathic scoliosis; Conservative treatment; Brace; Respiratory function; Schroth exercises
Introduction
Scoliosis is a complex deformity that is caused by the rotation of the spine on its axis and causes deformity in sagittal and transverse planes which mainly affects the coronal plane. Adolescent Idiopathic Scoliosis (AIS) occurs during the puberty period and affects 3% to 5% of adolescents. The age of onset of AIS is 10-16 and more common in girls [1]. Treatment options in AIS are made by considering the skeletal maturation of the patient. In the conservative treatment of AIS, for Cobb angle < 25º curvatures, the observation approach is preferred by six months intervals. Cobb curvatures 25-45º and Risser stage 0-2 immature adolescents are treated with brace and exercise [2]. Due to rotation on the transverse plane, the rib cage is affected and causes severe deformity in patients. Concerning the degree of curvature, there is a decrease in vital capacity and total lung volume in moderate (30-50 degrees) and severe (≥50) curves, while the residual volume remains within normal limits. The most important reason for these reductions is the deformation caused by curvature and rotation, limiting the lung parenchyma, and revealing lung volume and compliance restriction. As a result, asymmetry in the rib cage leads to an asymmetrical breathing pattern, pulmonary muscle weakness, and impairment of cardiopulmonary functions [3,4]. Recent studies on if there are pulmonary and functional restrictions in patients with AIS [5,6]. In addition, it is stated that the rigid braces used in the conservative treatment cause a decrease in the paravertebral muscle strength and lung capacity by restricting the rib cage movement. The effect of the brace on respiratory functions; it is closely related to many factors such as the size of the curvature, brace design, rib cage mobility, material rigidity and brace usage time [7]. Scoliosis Specific Exercises (SSE) which are planned specifically to curvature patterns is the general name of approaches with common basic principles generally including breathing applications. The Schroth method, which is a common SSE method provides that breathing exercises can increase the vital capacity and decrease the respiratory restrictions related to scoliosis [8].
The main purpose of this study is to compare the pulmonary functions of patients with AIS who use rigid scoliosis braces and do not perform exercise, with patients who use braces and perform regular Schroth exercises. In addition, it is also to reveal whether both methods make a difference in terms of respiratory function in the conservative treatment of scoliosis.
Material-Methods
This study was conducted in F**** H**** S**** C**** between December 2019 – October 2020. Twenty-four patients with AIS aged 10-16 years, with curves of 25-45º, were included in the study. AIS patients who were prescribed full-time rigid brace and Schroth exercises for 60 minutes 5 days a week by the physician, constituted the sample group of the study. The patients who wore the rigid brace and regularly performed the SSE therapy in the specified constituted the Brace & Exercise (N=12), and the patients who wore full-time rigid brace but did not perform exercise constituted the Brace group (N=12) of the study. The study was approved by the H** U** Non-Interventional Clinical Research Ethics Committee (approval numbered 167). It was carried out in accordance with the Declaration of Helsinki and registered at ClinicalTrials.gov (Registration number: NCT**** ). Research information was explained verbally and written to participants and their families/caregivers. A consent form was signed by the families/caregivers of the participants who agreed to participate in the study.
All patients enrolled in the study were informed that they should use the modified Cheneau type asymmetrical brace for 20 hours a day (full-time use). Cheneau-type braces are designed specifically for the curve pattern, skeletal maturity, flexibility, and structural component of the individual. With an asymmetrical design of braces, it applies torsional forces and three-point compression systems to improve spinal alignment in all three planes [9]. Patients were asked to record their wearing times in the “Brace Diary”. In the 8th week, the information obtained from the diary and approved by the parents were recorded as research data. The patients who had chronic respiratory diseases, smoking, and professional athletes, who did not perform the exercises regularly and did not compliance the brace did not enroll in the study.
The exercise protocol was defined for 60 minutes, 5 days a week, as recommended in the literature [10]. Exercises which specific to the patients’ curve type were taught by a certified experienced Schroth therapist to the patient. The Schroth method is an evidence-based exercise methodology developed by Katharina Schroth in Germany. Schroth exercises include asymmetric trunk exercises with rotational breathing. In this way, it is based on the reorganization of muscle imbalance due to rotational forces associated with scoliosis through sensoriomotor and kinesthetic stimulation [11,12]. It also includes posture training that will help individuals with scoliosis maintain the correct posture in their daily activities The exercises were performed with a physiotherapist once a week for the first 4 weeks, while the other sessions were performed as a home program and the application of the exercises was checked by the therapist. The frequency of the exercises of the patients was checked by the “Exercise Diaries”, and the patients who achieved 85% compliance with the program were included in the Brace & Exercise group.
Height, sitting height, weight, body mass index (BMI), gender, Tanner and Risser stages, type, and degree of the curve were recorded as demographic and clinical data. Patients’ maturity was determined at the beginning of the treatment according to Risser and Sanders stages as recommended in the literature [13]. The Risser classification is the grade of skeletal maturity based on the level of ossification and fusion of the iliac crest apophyses. Risser divided bone ossification and fusion levels into 6 different groups. Patients in the lower stage are assumed to be immature in terms of ossification and fusion level, while higher stages indicate that the patients are mature in terms of bone structure. Stage 0 describes an x-ray on which no ossification center is seen in the apophysis, whereas Stage 5 represents complete ossification and fusion of the iliac apophysis. Risser 0-2 are considered immature. Sanders classification is the degree of ossification of the physis in both the metacarpals and phalanges as a marker of skeletal maturity. It consists of 8 stages and patients with Sanders 0-6 are considered immature [14]. The respiratory functions of the patients in both groups were obtained at the beginning and 8th weeks of the treatment using a handheld type spirometer (SP10W, Contec). For spirometric measurement, the patient was seated in an upright position in a chair without armrests and positioned with the feet in contact with the ground. The procedure was demonstrated by a physiotherapist. Afterwards, for the measurement process, a clip was placed on the patient’s nose to keep the nostrils closed. The device was placed in the patient’s mouth, they were asked to take a deep breath and give it to the device with maximum force. Measurements were repeated three times and the highest measurement value accepted for the respiratory function data.
Results
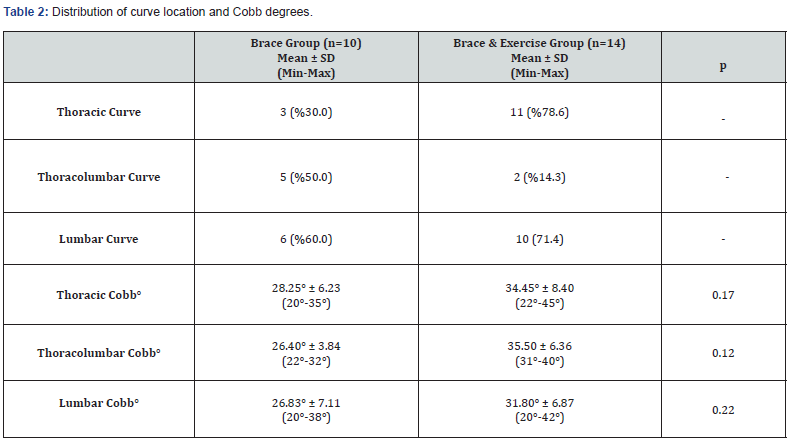
Twenty-four AIS patients enrolled in the study and ten patients were in the “Brace” group and fourteen patients were in the “Brace& Exercise” group. The mean age of the Brace group was 12.0±1.15, and the Brace & Exercise group was 12.42±1.22. The distribution of the demographic and clinical features of the patients was similar (Tables 1 & 2). The mean brace wearing time of groups were 21.40 ±1,35 and 20,79 ±1,12 in Brace and Brace & Exercise groups respectively. There was not statistically difference in between groups in scope of brace wearing time (p=0,20). Forced Vital Capasity (FVC), Forced Expiratory Volume in One Second (FEV1) and Peak Expiratory Flow (PEF) values were similar of patients at the beginning of treatment in both groups, and there was no statistical difference. In the 8th week of the treatment, although there was no difference between the groups in FVC and PEF values, there was a statistical increase in FEV1 in Brace & Exercise group in the comparison between the groups. The comparison of respiratory parameters of the groups before and after treatment is shown in Table 3. In the 8th week of the treatment, there was no difference in respiratory values ingroup comparison (Table 4).
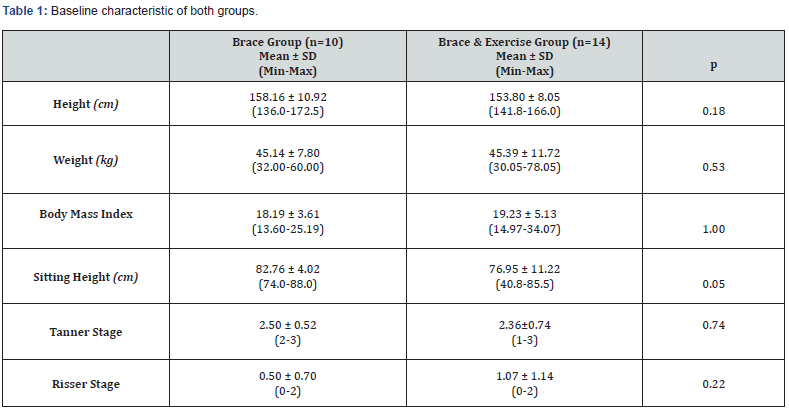
*Mann Whitney U test, p<0.05
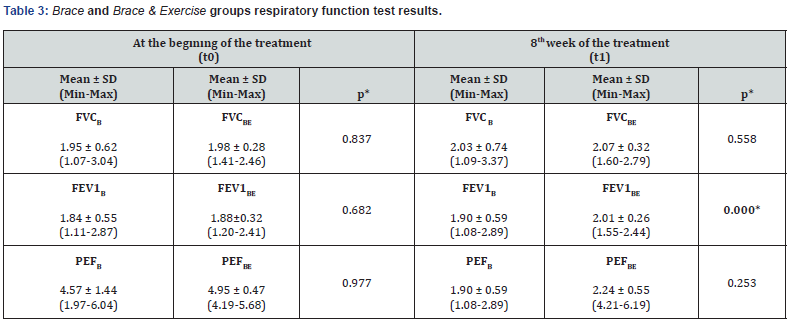
B: Brace Group BE: Brace & Exercise Group
FVC: Forced Vital Capacity FEV1: First Second of Forced Expiration, PEF: Peak Expiratory Flow
* Mann- Whitney U test, p<0.05
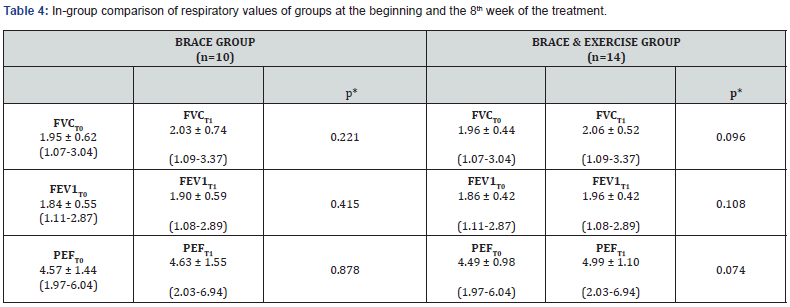
T0: Beginning of Treatment T1: 8th Week of Treatment
FVC: Forced Vital Capacity FEV1: First Second of Forced Expiration, PEF: Peak Expiratory Flow
* Wilcoxon test, p<0.05
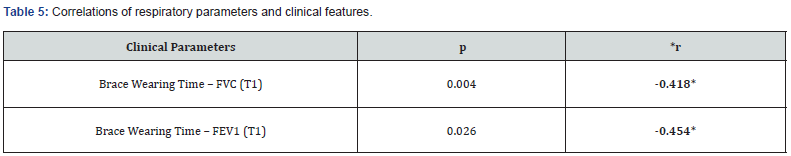
p= Significance value, r= Spearman Correlation
p < 0.05, r < 0.60 level relationship
T1: 8th Week of Treatment
In the correlation analysis between respiratory function values and brace wearing time; There was a significant negative correlation at r < 0.60 between 8th week of treatment and FEV1- FVC values and brace wearing time (Table 5). The relationship between respiratory parameters and brace wearing time of the patients is shown in Table 5. The effect size was found to be d<0.2 in terms of brace wearing time (Cohen`s d<0.2) [15].
Discussion
In this study, it was determined that the use of braces did not have a negative effect on respiratory functions in the short term. Respiratory problems in AIS are related to the severity of Cobb angle, age, comorbidities, and treatment methods. Also, the pathophysiological changes thought to be caused by scoliosis on the respiratory system are still controversial [13]. Despite early studies related to scoliosis reported that pulmonary functions are not significantly changed until the thoracic curve reaches higher than 100º however recent studies showed that pulmonary function deficits occur in a substantial proportion of patients with much smaller curves [16]. Alves et al. [17] reports that vertebral rotation and thoracic cage deformity due to AIS cause respiratory dysfunction by disrupting chest biomechanics. Previous studies have shown that scoliotic patients have narrower rib cages than non scoliotic patients. Also, trunk rotation and distortion of the rib cage can cause alterations on diaphragm and intercostal muscles that reduce the respiratory muscle capacity and muscle weakness [17,18]. Johnstone [18] reported that the deterioration of respiratory parameters in AIS patients with severe thoracic curvature compared to healthy controls. Kusvuran [19] reported that patients with AIS with mild/moderate curvature had lower FEV1, FVC, and PEF values compared to healthy controls Kusvuran et al. [19]. Similar to the study of Kusvuran et al. [19], it was found that the respiratory values of the patients enrolled in this study, at the beginning of the treatment respiratory values were lower than the healthy controls. Another reason for respiratory problems in AIS is associated with the use of rigid braces but the results are still debated. Katsaris et al. [20] and Korovessis et al. [21] reported that the use of a thoracolumbosacral orthosis (TLSO) in AIS patients may cause compression on the thorax, decrease in lung volume, and restrictive ventilation dysfunction.
Kennedy et al. [22] reported that there was a 26% decrease in functional residual capacity (FRC) after TLSO is used, and that FVC and FEV1 were also adversely affected. In this study, there was no decrease in respiratory parameters at the 8th week in patients who used full-time braces. This may be related to the short-term effect as the asymmetrical design of the braces allows expansion of the rib cage in all three planes. Gao et al. [23] found a significant decrease in respiratory values after using the TLSO model rigid brace for 6 months. Yu et al. [24] deterioration of respiratory parameters after 17.5 months of follow-up, Willers et al. [25] reported a decrease in vital capacity and adverse effects on lung functions after rigid brace treatment with 8.5 years of follow-up. Contrary to all this, Gao et al. [23] like this study, did not find a significant decrease in respiratory parameters at the end of 4-week follow-up of patients using rigid braces. Sevastikoglou et al. [26] and Barrios et al. [27] did not find a significant difference in respiratory values after an average of 16 months of brace use compared to healthy controls. Although several studies in literature assess the relationship of severity of AIS and pulmonary functions, to our knowledge, there are few studies examining the relationship between the use of asymmetrical rigid braces and respiratory functions in short and long-term follow-up. Some studies showed a decrease in FRC, total lung capacity (TLC), vital capacity (VC), and maximum voluntary ventilation (MVV) in patients who use the rigid brace. According to Yagci et al. [28] TLSO type brace used in AIS patients caused a decrease in FEV1, VC, FVC, MVV, and PEF even after using the brace. Katsaris et al. [20], a decrease in VC, RV, FRC, TLC, and FEV1 after 10 minutes of use of a Boston type rigid brace and Ran et al. [29] a decrease in FVC and FEV1 after use of a Boston type brace have been reported.
The common trait of these studies is that a rigid brace that has a symmetrical design was used in the treatment of patients with AIS. In this research, there was not any deterioration in respiratory values in both groups according to the beginning of the brace treatment. The main difference between the results of this research and the literature is that the braces used in this study are the asymmetric Cheneau type braces. Cheneau type braces have expansion space, allow chest expansion, and enable asymmetric rotational breathing. Classic TLSO’s or Boston type braces have a symmetrical biomechanical design and do not provide this advantage for chest expansion. As a result of the insufficient expansion of the lungs, inability to maintain thoracic cage mobility, and inability to perform rotational breathing effectively in relation to this, a decrease in respiratory parameters may have been found in both instant and short-term use. Schroth exercises are a treatment method that includes 3-dimensional, rotational deep breathing exercises. Otman et al. [3] followed 50 AIS patients by Schroth exercises 5 days a week for 6 weeks, and they found an increase in VC and respiratory muscle strength in the patients at the end of the treatment. Moramarco et al. [30] found significant changes in VC and Maximum Expiratory Pressure (MEP) values in the Schroth group of 8-week follow-up. In this study, there was no significant difference between the groups in respiratory values except FEV1 at the end of the 8-week follow-up (Table 3). Gao et al. [23] followed their patients as brace (n=22) and braceexercise (n=23) groups and reported significant increases in FVC and FEV1 in the brace and exercise group at the 6th month results. In this study, the increase detected only in FEV1 was associated with Schroth exercises were based on forced inspiration and expiration. It should also be considered that the increase in FEV1 alone may be the result of the short-term effect of exercise. In our study, there was a moderate negative correlation between brace wearing time and FVC-FEV1 values at the 8th week of the treatment (r=-0.418 and r=-0.454, respectively) (Table 5).
Despite this negative correlation, the absence of difference in respiratory parameters in the groups (except FEV1 value in Brace & Exercise group) at the beginning and 8th week of the treatment was associated with the mean and standard deviation values of the groups were close and the effect size was small. Gao (2019) found a decrease in FVC and FEV1 values and similar to that, Ran [29] found a decrease in %FEV1 value in patients with AIS patients with using full-time braces Gao et al. [23]; Ran et al. [29]. Yagci et al. [28] reported an increase in the perception of dyspnea in AIS patients who using brace and it was associated with decreased FEV1, FVC, and FEV1/FVC Yagci et al. [28]. In our study, it was revealed that FVC and FEV1 decreased compared to the initial values of treatment at the 8th week of the treatment. Although this relationship was obtained in correlation analyses, it could not be statistically demonstrated. This situation is associated with the number of samples, and a negative correlation between wearing time and expansion is more affected by this situation. However, it was also obtained that the asymmetrical brace used in our study affected respiratory values less than the symmetrical braces.
This study has some limitations. The most important limitation of this study is the small sample size because the study was conducted during the Coronavirus pandemic period. This was an important reason for this process is that patients abstain from treatment during the pandemic. Another limitation of the study is that the participants could not be blinded to the interventions due to ethical conditions. In AIS treatment, brace and exercise therapy are recommended together during the rapid growth period. Therefore, these treatments were offered to both groups.
Conclusion
In this study, it was determined that the use of a full-time brace did not cause a deterioration in respiratory values, and performing Schroth exercises during the follow-up period could have a positive contribution to FEV1. It is thought that the negative effects of a rigid brace on respiration in AIS can be prevented by Schroth exercises and asymmetric braces.
Ethics Approval
The study was approved by the Halic University Non- Interventional Clinical Research Ethics Committee 10.03.2019 date ethics committee, approval numbered 167 and was carried out in accordance with the Declaration of Helsinki and registered at ClinicalTrials.gov (Registration number: NCT05505695 ).
Conflict of Interest
The authors declare no conflict of interest.
References
- Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7(1): 3-9.
- El-Hawary R, Chukwunyerenwa C (2015) Update on evaluation and treatment of scoliosis. Pediatr Clin N Am 61(6): 1223–1241.
- Otman, S, Kose, N, Yakut Y (2005) The efficacy of Schroth's 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Neurosciences 10(4): 277- 283.
- Park S, Shim J (2015) Effect of 8 weeks of schroth exercise (Three-dimensional convergence exercise) on pulmonary function, Cobb’s angle, and erector spinae muscle activity in idiopathic scoliosis. Journal of the Korea Convergence Society 14: 61-68.
- Kım MJ, Park DS (2017) The Effect of Schroth’s three-dimensional exercises in combination with respiratory muscle exercise on Cobb’s angle and pulmonary function in patients with idiopathic scoliosis. Physical Therapy Rehabilitation Science 6(3): 113-119.
- Abdelaal AAM, Abd El Kafy EMA, Elayat MMS, Mohamed Sabbahi, Mohamed Salem Saed Badghish, et al. (2015) Changes in pulmonary function and functional capacity in adolescents with mild idiopathic scoliosis: Observational cohort study. Journal of International Medical Research 3: 451-457.
- Negrini S, Negrini A, Romano M, Nevia Verzini, Alessandra Negrini, et al. (2006) A controlled prospective study on the efficacy of SEAS: Exercises in preparation to bracing for idiopathic scoliosis. Stud Health Technol Inform 123: 519-522.
- Burger M, Coetzee W, du Plessis LZ, Larissa Geldenhuys, Francois Joubert, et al. (2019) The effectiveness of schroth exercises in adolescents with idiopathic scoliosis: A systematic review and meta-analysis. S Afr J Physiother 75(1).
- Wood GI, Rigo M (2017) The principles and biomechanics of the Rigo Chêneau type brace. In J. Bettany-Saltikov, & S. Schreiber (Eds.), Innovations in Spinal Deformities and Postural Disorders. IntechOpen Innovations in Spinal Deformities and Postural Disorders.
- Burger M, Coetzee W, du Plessis LZ, Larissa Geldenhuys, Francois Joubert, et al. (2019) The effectiveness of Schroth exercises in adolescents with idiopathic scoliosis: A systematic review and meta-analysis. S Afr J Physiother 75(1): 904.
- Yang JM, Lee JH, Lee DH (2015) Effects of consecutive application of stretching, Schroth, and strengthening exercises on Cobb’s angle and the rib hump in an Adult with İdiopathic Scoliosis. J Phys Ther Sci 27(8): 2667-2669.
- Kuru T, Yılmaz H (2012) Assessment of stress in adolescent idiopathic scoliosis patients while wearing a brace. 2012: 8th international conferance on conservative management of spinal deformities and SOSORT 2011 annul meeting.
- Trobisch P, Suess O, Schwab F (2010) Idıopathıc scoliosis. Dtsch Arztebl Int 107(49): 875–878.
- Hacquebord JH, Leopold SS (2012) In brief: The risser classification: A classic tool for the clinician treating adolescent idiopathic scoliosis. Clinicaş Orthopaedics and Related Research 470(8): 2335-2338.
- Gravesande J, Richardson J, Griffith L, Fran Scott (2019) Test-retest reliability, internal consistency, construct validity and factor structure of a falls risk perception questionnaire in older adults with type 2 diabetes mellitus: a prospective cohort study. Arch Physiother 9(1): 1–11.
- Kempen DH, Heemskerk JL, Kacmaz G, Mark C Altena, Herre J Reesink, et al. (2022) Pulmonary function in children and adolescents with untreated idiopathic scoliosis: a systematic review with meta-regression analysis. Spine J 22(7): 1178-1190.
- Alves VLS, Stirbulov R, Avanzi O (2006) Impact of a physical rehabilitation program on the respiratory function of adolescents with idiopathic scoliosis. Chest 130(2): 500-505.
- Johnston CE, Richards BS, Sucato DJ, Keith H Bridwell, Lawrence G Lenke, et al. (2011) Spinal deformity study group. Correlation of preoperative deformity magnitude and pulmonary function tests in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 36(14): 1096–102.
- Kusvuran A, Yildirim B, Yılmaz H (2020) Respiratory function in adolescent girls with mild and moderete idiopathic scoliosis. Journal Of Turkish Spinal Surgery 31(2): 75-79.
- Katsaris G, Loukos A, Valvanis M, M Vassiliou, P K Behrakis, et al. (1999) The immediate effect of a boston brace on lung volumes and pulmonary compliance in mild adolescent idiopathic scoliosis. European Spine Journal 8(1): 2–7.
- Korovessis P, Kyrkos C, Piperos G, P N Soucacos (2000) Effects of thoracolumbosacral orthosis on spinal deformities, trunk asymmetry, and frontal lower rib cage in adolescent idiopathic scoliosis Spine 25(16): 2064–2071.
- Kennedy JD, Robertson CF, Olinsky A, D R Dickens, P D Phelan et al. (1987) Pulmonary restrictive effect of bracing in mild idiopathic scoliosis Thorax 42(12): 959–961.
- Gao Zheng Y, Fan C, Yang Y, He C, Mansang Wong, et al. (2019) Could the clinical effectiveness be improved under the integration of orthotic intervention and scoliosis-specific exercise in managing adolescent idiopathic scoliosis?: A randomized controlled trial study. American Journal of Physical Medicine & Rehabilitation 98(8): 642-648.
- Yu B, Wang Y, Qiu G, Jianxiong Shen, Jianguo Zhang, et al. (2013) The influence of preoperative brace treatment on the pulmonary function test in female adolescent idiopathic scoliosis. J Spinal Disord Tech 26(6): E254–E258.
- Willers U, Normelli H, Aaro S, O Svensson, R Hedlund (1993) Long-term results of boston brace treatment on vertebral rotation in idiopathic scoliosis Spine 8(4): 432–435.
- Sevastikoglou JA, Linderholm H, Lindgren U (1976) Effect of the milwaukee brace on vital and ventilatory capacity of scoliotic patients. Acta Orthop Scand 47(5): 540–545.
- Barrios C, Perez-Encinas C, Maruenda J, Manuel Laguia et al. (2005) Significant ventilatory functional restriction in adolescents with mild or moderate scoliosis 45 during maximal exercise tolerance test. Spine 30(14): 1610–1615.
- Yagci, G, Demirkiran, G, Yakut Y (2019) In-brace alterations of pulmonary functions in adolescents wearing a brace for idiopathic scoliosis. Prosthetics and Orthotics International 43(4): 434-439.
- Ran B, Fan Y, Yuan F, Kaijin Guo, Xiaodong Zhu (2016) Pulmonary function changes and its influencing factors after preoperative brace treatment in patients with adolescent idiopathic scoliosis. A retrospective case–sontrol study. Medicine 95(43): e5088.
- Moramarco M, Fadzan M, Moramarco K, Amy Heller, Sonia Righter et al. (2016) The influence of short-term scoliosis-specific exercise rehabilitation on pulmonary function in patients with AIS. Current Pediatric Review 12(1): 17-23.






























