Investigation Of Mobility Challenges Faced by Trans-Tibial Prosthesis Users
Tochukwu Nze Ugorji1*, Churchill Chisom Ogbonna2, James ifeanyi Nwakamma3 and Jane Nduchekwe1
1Department of Prosthetics and Orthotics, School of Health Technology, Federal University of Technology Owerri Imo Satate.
2Department of Biomedical Engineering, David Umahi Federal University of Health Sciences Uburu Ebonyi State Nigeria.
3Department of Prosthetics and Orthotics, Federal College of Dental Technology and Therapy Enugu.
Submission:August 15, 2023; Published:October 12, 2023
*Corresponding author: Tochukwu Nze Ugorji. Postal Address: Department of Prosthetics and Orthotics, Federal University of Technology Owerri Imo State Nigeria
How to cite this article: Tochukwu Nze U, Nduchekwe J. Investigation Of Mobility Challenges Faced by Trans-Tibial Prosthesis Users. Ortho & Rheum Open Access J. 2023; 22(3): 556086. DOI: 10.19080/OROAJ.2023.22.556086
Abstract
Background: Rehabilitation and reintegration of trans-tibial amputees do not give required optimal results at times. Studies have continuous being conducted on how to identify these challenges that hamper user’s optimal performance with prosthesis, so as proffer solutions to them. Insight into these challenges will help the caregivers to know the predominant ones and guide against their occurrences in susceptible amputees, to achieve a better rehabilitation and reintegration for them.
Method: This study used the descriptive approach to determine the occurrence level of different mobility challenges experienced by different categories of amputees. Raw data was obtained from 100 trans-tibial prosthesis users in South-East Nigeria through questionnaire and physical assessments. Tables and percentage analysis were used to present the data.
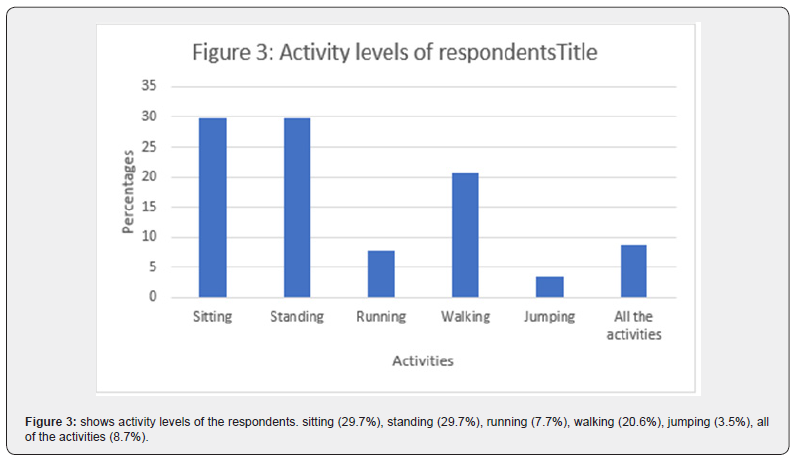
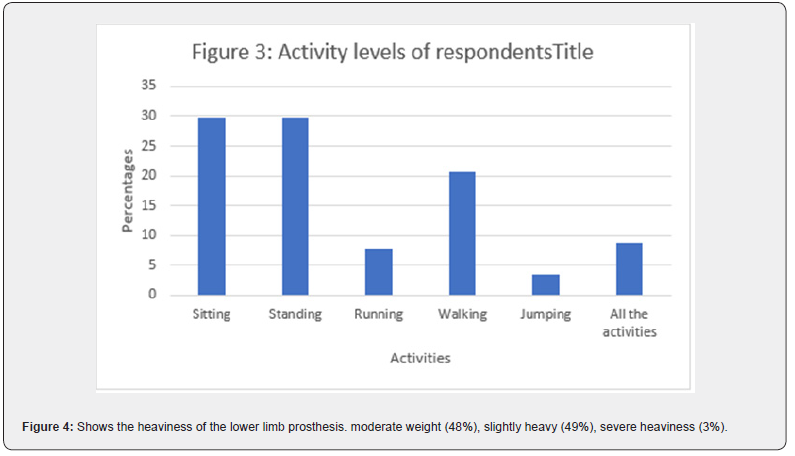
Results: 68% reported it was difficult to use prosthesis, while 32% reported no difficulty. The challenges/difficulties reported by amputees are pistoning effect (14.9%), poor foot clearance (33.8%), waddling gait (3.9%), pain on the stump (33.8%), and tightness of socket on the stump (21.4%). Activities achieved with the prosthesis are sitting (29.7%), standing (29.7%), running (7.7%), walking (20.6%), jumping (3.5%), all the activities (8.7%). Heaviness of the prostheses was reported as; moderate weight (48%), slightly heavy (49%), severe heaviness (3%).
Conclusion: Trans-tibial amputees are faced with some mobility challenges which included poor foot clearance, pain on the stump, tightness of prosthesis on the stump, pistoning effect and waddling gait in South-East Nigeria. This could be because of materials used, training given to prosthesis users or the skill level of the caregivers.
Keywords:Challenges; Amputee Trans-tibial prosthesis; Mobility; South-East Nigeria
Introduction
Amputation, which is mother to prosthesis had been defined as the removal of a limb by trauma, medical illness, or surgery [1,2]. It can also be defined as loss of body part following injury or disease through surgical procedure or automatic amputation (in the case of crush injury). There could also be a congenital absence of a body part. Individuals (amputees) who had benefited from amputation will have the need to be rehabilitated and reintegrated into society to continue with their normal socio-economic activities using prosthesis [1,3-5]. A prosthesis is a device designed to substitute the function or appearance of a missing limb or body part [6]. Producing an artificial device that will take over the form and functions of a lost human leg is not an easy one because of the complexity of human structures. Therefore, an ideal prosthesis must be comfortable, easy to don and doff, light weight, durable, cosmetically pleasing, functioning mechanically well and requires reasonable maintenance [4,7]. Studies have been conducted on how to improve material quality and technology in fabricating artificial limbs for amputees, as well as to identify the difficulties experienced by users of the artificial limbs, to get feedback that can be useful to improve the designing and fabrication of artificial limbs that will rehabilitate and reintegrate amputees into the society better [8-12].
Below-knee prosthesis users, sometimes come back to the clinic with complaints of inability to use their prosthesis conveniently and effectively, and some even end up abandoning their prosthesis, especially in developing countries like Nigeria. This study aims to identify the most prevalent challenge(s) that hinder below-knee amputees from effective use of prosthesis, and the most susceptible group(s) to each of these challenges. This, when established, will help caregivers to know the most common limiting challenges to the amputees, the most susceptible group of amputees to the challenge(s), and work vigorously to tackle and guide against such challenge during the fabrication and entire rehabilitation processes. This will also help them to know the challenges/faults to look out for, when below-knee prosthesis come back to the clinic with complaints of inability to use prosthesis effectively [13].
Trans-tibial prosthesis is a type of lower limb prosthesis that is fitted along the length of the remaining tibia bone after amputation. It is used to rehabilitate/mobilize trans-tibia/belowknee amputees. It can also be referred to as below-knee prosthesis because it does not have a knee joint [14,15]. Trans-tibial prosthetics users at times do not function optimally, especially when not given a satisfactory prosthesis and this can affect their ability to work and general function. There is need to investigate these mobility challenges and know the most prevalent ones, to help prosthetic users and rehabilitation team to guide against such anticipated mobility challenges and proffer solution on how to cope with them when they exist [16-18].
Materials and Methods
The study made use of a descriptive survey approach, which required selection of respondents from a population of amputees. Any amputee encountered, who was ready and willing to be part of the study was included. Questionnaire for data collection was designed in simple terms, printed and hard copy distributed to amputees and some of the respondents who couldn’t fill out their questionnaires, were helped to do so.100 respondents from the five states that make up the south-eastern Nigeria participated in the study.
Results
(Table 1).
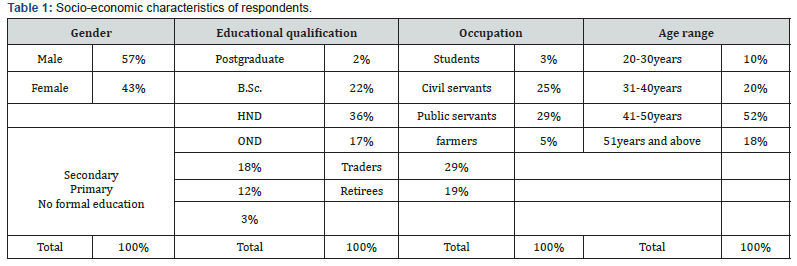
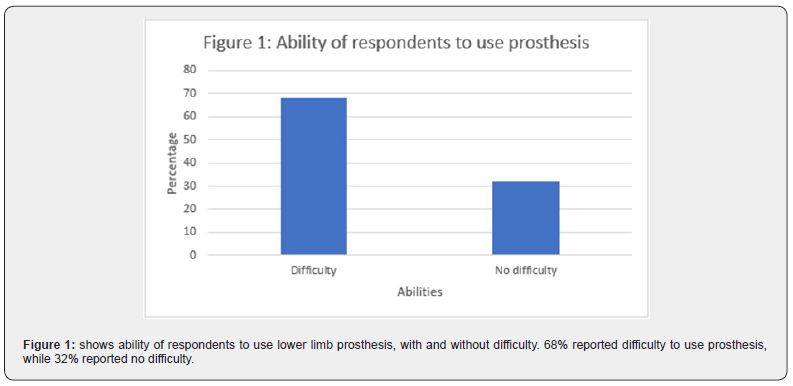
Table 1 shows the gender distribution of respondents, with male and female being 57% and 43%, respectively. It also shows the educational distribution of respondents as; 2% had postgraduate education, 22% are B.Sc. holders, 26% are HND holders, 17% are OND holders, 18% are O ’level holders, 12% are FSLC holders and 3% had no formal education. occupational distribution of respondents is as follows: 3% were students, 25% were civil servants, 29% were public servants, 5% were farmers, 29% were traders and 9% were retirees. Age range distribution of the respondents is as follows; 10% were 20-30years old, 20% were 31-40years old, 52% were 41-50years and 18% were 51years and above (Figures 1-3).

Material/physical characteristics of the trans-tibial prosthesis
(Figures 4-8).

Discussion
The purpose of this study is to categorize trans-tibial prosthesis users based on socio-economic demography and identify the mobility challenges faced by trans-tibial prosthesis users and classify them based occurrence frequency to know the most frequent and anticipated challenge that the caregivers should guide against or improve their design and fabrication skills to overcome them. There are more male (57%) trans-tibial prosthesis users than female (43%) which could be because of engagement of male in physical activities than female that makes them more prone to amputation. More enlightened amputees go for prosthesis, which could be attributed to their socio-economic status and access to information about prosthesis. Amputees within the age range of 41-50years and 31-40yeras were the highest users of prosthesis. This could be because of access to resources because most people attain economic independence at that age, coupled with active style of people at that age [19]. Public servants, traders and civil servants were the highest users of trans-tibial prosthesis, respectively. This can be attributed to their socio-economic status and active lifestyle as well [20]. (68%) of the tans-tibial prosthesis users had difficulty in using their prosthesis. Pain on the stump, poor foot clearance and tightness of the socket on the stump were the most prominent difficulties experienced by trans-tibial prosthesis users. This could be attributed to the level of expertise of the caregivers and available materials for fabrication of prosthesis [21].
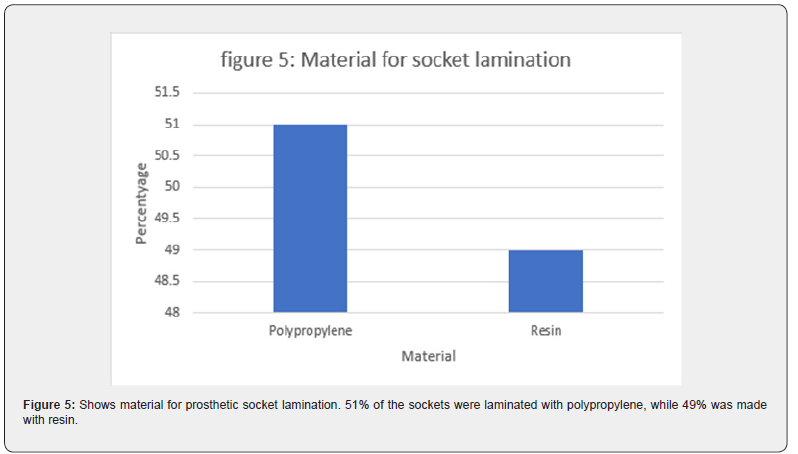
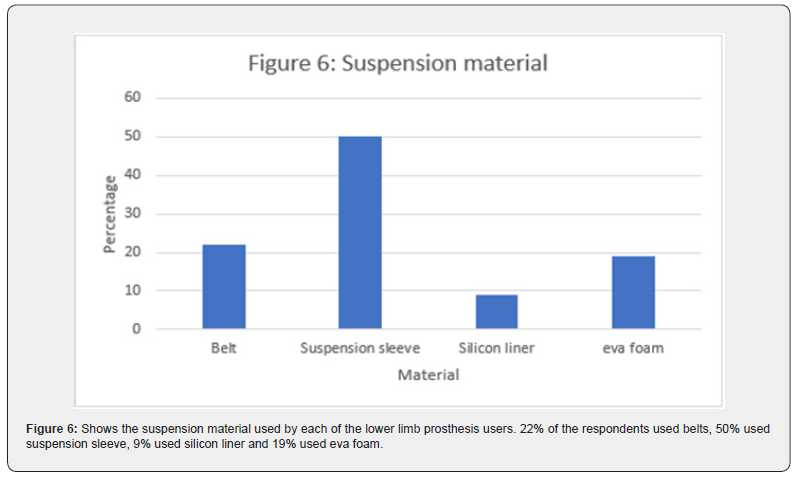
The most prominent activities achieved by the trans-tibial prosthesis users are sitting, standing, and walking, respectively. Only (3%) of trans-tibial prosthesis users reported of their prosthesis being severely heavy for them. Polypropylene and resin were the materials for lamination of trans-tibial prosthesis socket. Suspension sleeve (50%) dominated as the prosthesis suspension material, while few amputees (9%) used silicon suspension, probably because of its high cost. Most of the amputees (73%) used foreign pylon, which indicates that the technology for its manufacture might not be readily available, and majority of the amputees (85%) used single axis foot.
Conclusion
Trans-tibial amputees are faced with some mobility challenges which included poor foot clearance, pain on the stump, tightness of prosthesis on the stump, pistoning effect and waddling gait in South-East Nigeria. These most likely challenging experiences of trans-tibial prosthesis users are to be guided against in designing, fabrication and fitting of lower limb prosthesis, via; improved materials for fabrication, improved technology, and adequate skills for caregivers, to rehabilitate the amputee better and effectively.
References
- Agrawal V, Gaunaurd I, Kim KJ, Bennett C, Gailey RA (2022) Comparison of the Center of Pressure Trajectory Between Dynamic Response Prosthetic Feet Having Different Ankle Designs. J Prosthet Orthot 34(2): 44-51.
- Ernest M, Altenburg B, Schmalz T (2020) Characterizing Adaptations of Prosthetic Feet in the Frontal Plane. Prosthet Orthot Int 32(44): 225-233.
- Jayne DM, Scoville C (2013) Development and Reliability Testing of the Comprehensive High-Level Activity Mobility Predictor (CHAMP) in Male Servicemembers with Traumatic Lower-Limb Loss. J Rehabil Res Dev 50(3): 905-918.
- Horne CE, Neil JA (2019) Quality of life in patients with prosthetic legs: A comparison study. Journal of Prosthetics and Orthotics 21(3): 154-159.
- Klodd E, Hansen A, Fatone S, Edwards M (2010) Effects of Prosthetic Foot Forefoot Flexibility on Gait of Unilateral Transtibial Prosthesis Users. J Rehabil Res Dev 47(9): 899-910.
- Sinha R, van den Heuvel WJ, Arokiasamy P (2011) Factors Affecting Quality of Life in Lower Limb Amputees. Prosthet Orthot Int 35(1): 90-96.
- Highsmith MJ, Kahle JT, Miro RM, et al. (2016) Prosthetic interventions for people with transtibial amputation: systematic review and metaanalysis of high-quality prospective literature and systematic reviews. J Rehabil Res Devel 53(2): 157-184.
- Walke KM, Pandure PS (2017) Mechanical Properties of materials used for prosthetic foot: A Review. J Mech Civil Engineering 2278(1684): 61-65.
- Ugorji TN, Osuagwu CG, Ekezie J, Igwe A, Okeafor W (2017) Design and Fabrication of Improved Below-Knee Prosthesis to Better Mimic Natural Limb. Current Trends in Biomedical Engineering and Biosciences 10(2): 1-4.
- Mark AF, Zhang M, Boone DA (2001) State-of-the-art research in lower-limb prosthetic biomechanics-socket interface: A review. Journal of Rehabilitation Research and Development 38(2): 161-174.
- Ahmed NH, Jawa KO (2015) Improve Flexural Strength of PMMA/SR Polymer Blend by Reinforcement with Carbon Fibers as Prosthetic Foot Polymer Material. Int J Appl Innov Engi Manag (IJAIEM) 4(2): 172-176.
- Andrysek J (2010) Lower-limb prosthetic technologies in the developing world: A review of literature from 1994–2010. Prosthet Ortho Int 34(4): 378-398.
- Elaine AB, Tom TC (2007) Upper limb prosthesis use and abandonment: A survey of the last 25years. Prosthet Orth Int 31(3): 236-257.
- Highsmith MJ, Kahle JT, Lewandowski A, et al. (2016) Economic evaluations of interventions for transtibial amputees: a scoping review of comparative studies. Technol Innov 18(2-3): 85-98.
- Ugorji TN, Agbasi PU, Daniel JA, Azeez TO, Nwakanma JI, et al. (2023) Comparison of the Physical Properties Between Resin and Polypropylene Laminated Trans-Tibial Prosthetic Socket. Current Trends in Biomedical Engineering and Bioscience. 21(2): 1-7.
- Aaron L, Glenn G, Robert SR (2016) Lengthening of tibia after trans-tibial Amputation: Use of a weight Bearing External Fixator-Prosthesis Composite. HSSJ 12(1): 85-90.
- Armstrong C (2013) Ankle functions, The next frontier for clinical outcomes among lower limb amputees. Am Academy of Orthopaedic surgeon 2(45).
- Au S, Berniker M, Herr H (2008) Powered ankle-foot prosthesis to assist level-ground and stair-descent gaits. Neural Netw 21(4): 654-666.
- Coleman KL, Boone DA, Laing LS, Mathews DE, Smith DG (2004) Quantification of prosthetic outcomes: elastomeric gel liner with locking pin suspension versus polyethylene foam liner with neoprene sleeve suspension. J Rehabil Res De 41(4): 591-602.
- Davis RB, Õunpuu S, Tyburski D, Gage JR (1991) A gait analysis data collection and reduction technique. Human Movement Science 10(5): 575-587.
- Genin JJ, Bastien GJ, Franck B, Detrembleur C, Willems PA (2008) Effect of speed on the energy cost of walking in unilateral traumatic lower limb amputees. Eur J Appl Physiol 103(6): 655-663.






























