Traumatic Hip Dislocation Associated with Iatrogenic Proximal Femoral Physeal Fracture in Children: A Systematic Review and Case Report
Sulaiman Mohammed Hushlul*, Rayyan Saeed suqaty, khalid idris and Ahmad Abdullah Alsulami
Degree of Bachelor of Medicine MBBS, UQU, Saudi Arabia board of orthopedic surgery, Saudi Arabia
Submission:September 11, 2023; Published:September 26, 2023
*Corresponding author: Sulaiman Mohammed Hushlul, Degree of Bachelor of Medicine MBBS, UQU, Saudi Arabia board of orthopedic surgery, Saudi Arabia
How to cite this article: Sulaiman Mohammed H. Traumatic Hip Dislocation Associated with Iatrogenic Proximal Femoral Physeal Fracture in Children: A Systematic Review and Case Report. Ortho & Rheum Open Access J. 2023; 22(2): 556085. DOI: 10.19080/OROAJ.2023.22.556085
Abstract
Background: Traumatic hip dislocation (THD), which accounts for 3% of all joint dislocations in children which is a rare condition. pediatric hip dislocation with transphyseal femoral neck fracture accounts for less than one percent of all hip injuries. Less than 8% of hip fractures and 1% of pediatric fractures are caused by femoral head and neck fractures. A high rate of complications is linked to transphyseal femoral neck fracture related THD. Avascular necrosis, premature epiphyseal closure, nonunion, soft tissue loss injuries in open fracture-dislocation that necessitate negative pressure wound therapy, leg length discrepancy, coxavara, and the angular deformity that goes along with it are list of these complications.
Report: A 15-year-old boy medically free case of road traffic accident (RTA) sustained right distal radius fracture which reduced and treated conservatively and right hip posterior dislocation, three trails of reduction in peripheral hospital result in iatrogenic transphyseal proximal femur fracture dislocation. Treated surgically by cannulated screws but still dislocated. We receive this patient in our hospital as an emergency case, planned and operated on in next day. Pushed as emergency case to operative room and reduced and fixed with plate and screws. Suggest early intervention with anatomical reduction and stable fixation with closure of the capsule and the labrum will give a good result and increase the stability of hip joint.
Keywords: Hip Dislocation; Proximal Femoral Physeal Fracture; Iatrogenic complication
Introduction
Traumatic hip dislocation (THD), which accounts for 3% of all joint dislocations in children which is a rare condition [1]. There are four types of traumatic hip dislocation, all of which are related to the relationship between the acetabulum and the displaced femoral head: central, inferior, anterior, posterior, and central [2]. The posterior hip dislocation, which occurs approximately nine times more frequently than the anterior type [3]. Hip dislocations in pediatrics can be brought on by both low-energy trauma and same-level falls, as well as high-energy trauma like car accidents and falls from height [4]. Due to the hyperlaxity of the periacetabular structures, low-energy trauma, such as slips, can result in these injuries in children under the age of five. Due to the high-energy trauma involved, hip dislocations in older children approaching skeletal maturity resemble those of adults [5,6]. Dislocation can weaken the growth plate [7,8]. Fractures of the femoral neck typically occur more frequently in older patients, but they can also occur in younger patients with various systematic diseases [9].
In rare conditions, pediatric hip dislocation with transphyseal femoral neck fracture accounts for less than one percent of all hip injuries [9]. Less than 8% of hip fractures and 1% of pediatric fractures are caused by femoral head and neck fractures [10]. The location of the fracture is the basis for the Delbet and Colonna classification of femoral neck fractures. This indicates that type I fracture, also known as transphyseal separation, is the least common type of fracture and may result in femoral head osteonecrosis [9-11]. The type of fracture, the patient's age, and the time between the traumatic event and the patient's admission to the hospital all determine the course of treatment for pediatric hip fractures and dislocations. IN the operating room (OR), it consists of pain management and urgent reduction. open reduction of the dislocation and fracture as well as internal fixation of the physeal separation and Cast immobilization is required after reduction [4]. After reduction, it is recommended that children under the age of 10 wear a spica cast for three to four weeks. The recommended period of cast immobilization following reduction is between six and twelve weeks for patients over the age of 10 [5]. THD is a medical emergency that necessitates prompt orthopedic evaluation and treatment [12]. The femoral head's blood supply needs to be carefully examined due to the high risk of AVN. The primary blood supply to the femoral head is provided by the medial femoral circumflex artery, which emerges from the profunda femoris artery [12].
The risk of separating the capital femoral epiphysis (CFE) from the femoral neck must be carefully guarded during reduction; This may have an impact on the physis' or CFE's biomechanics. When the CFE is reduced in the acetabulum, it may separate from the femoral neck [13]. Acute vascular disruption that affects the lateral circumflex artery and causes irreversible blood loss to the CFE is likely to result from partial reduction [14]. In this type of lesion, early reduction is essential to reduce the risk of ischemic (avascular) necrosis [15]. Vascular shearing, blood supply disruption, and local ischemia are potential causes of femoral head and neck osteonecrosis [9]. In the treatment of THD, it is mandatory to perform a closed reduction as soon as possible and to diagnose the condition as soon as possible. The following cases call for open reduction: fracture-dislocation is impossible, as is a closed or concentric reduction [2]. A high rate of complications is linked to transphyseal femoral neck fracture related THD [2]. Avascular necrosis, premature epiphyseal closure, nonunion, soft tissue loss injuries in open fracture-dislocation that necessitate negative pressure wound therapy [16], leg length discrepancy, coxavara, and the angular deformity that goes along with it [9] are list of these complications. We wanted to learn more about this kind of injury to find the best treatment with a better outcome. As a result, we conducted this systematic review and investigated the literature cases treatment and prognosis of complications and presented our case report.
Material and Methods
Using the following keywords, we conducted the study on PubMed, Google Scholar, and Web of Science: fracture-dislocation of the hip in children, traumatic hip dislocation in children and hip dislocation in children associated with a transphyseal fracture. There was a total of 617 articles that met these criteria. All these articles were reviewed by us using Covidence. inclusion criteria were Children between the ages of 10 and 18, hip dislocation with physeal separation and articles published after 1990 were all considered. The exclusion criteria were Patients with transphyseal femoral head and neck fracture or THD alone, patients with associated systemic conditions, incorrect study design, and articles published prior to 1990 and we omitted all articles written in languages other than English. There was a total of 11 articles included in our study (Tables 1-3). All the cases were examined clinically and radiologically at two weeks, one, two, three, four, five, six, and twelve months, and at the final follow-up. Osteonecrosis occurred in all patients within six months on average. Our study's primary objective was to determine the incidence of osteonecrosis following this type of injury. Finding a connection between osteonecrosis, age, gender, and the acetabular fracture that was associated with it was the secondary objective and presenting a case report for iatrogenic proximal femur transphyseal fracture dislocation.
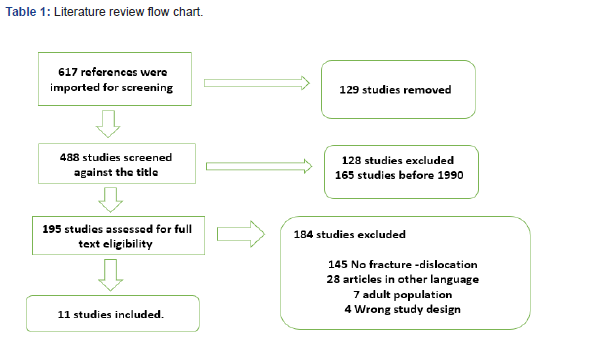
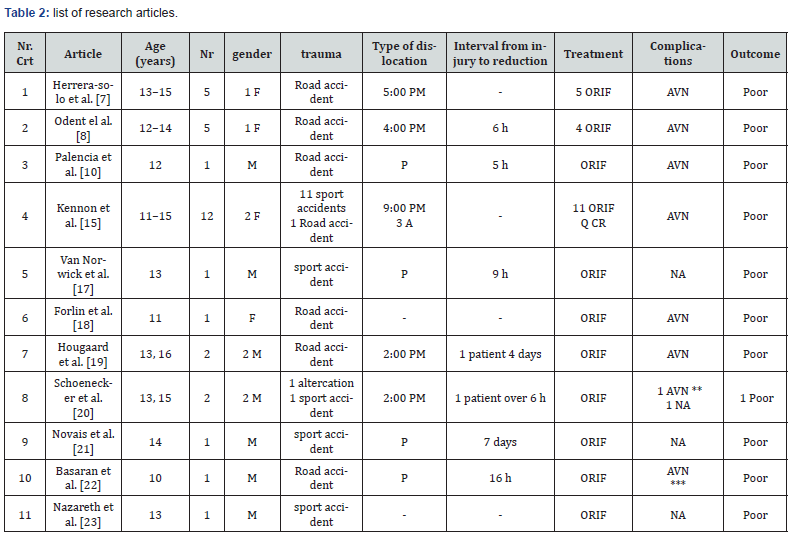
M= male; F = female; P = posterior; A = anterior; ORIF = open reduction with internal fixation; CR = close reduction; NA = non associated; AVN = avascular necrosis; * associated premature Physeal closure and chondrolysis; ** associated subluxation of the femoral head; *** associated arthritis and femoral head subluxation.
M = male; F = female; ORIF = open reduction with internal fixation; CR = close reduction; NA = nonassociated; AVN = avascular necrosis; * associated premature physeal closure and chondrolysis; ** associated subluxation of the femoral head; *** associated arthritis and femoral head subluxation.
Result
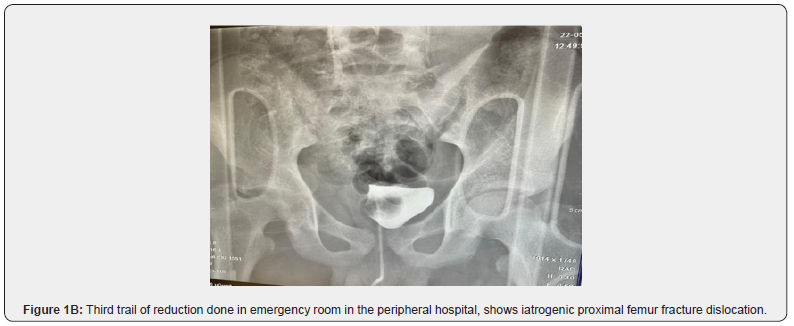
We evaluated 35 patients between 10 and 16 years old, the average age at diagnosis was 13 years and 2 months. There were 30 men and 5 women. Road accidents (16 patients) and sports accidents (16 patients) were the most common causes of injuries. There were four anterior dislocations in addition to 29 posterior ones; The type of dislocation was not specified in two cases. For 16 patients, the interval between diagnosis and reduction ranged from 5 hours to 7 days; It was not documented for the remaining 19 patients. Eight patients had additional associated lesions (acetabulum fractures, peroneal nerve paralysis, distal radius fracture, femoral head fracture, bilateral tibiae and fibular fracture, multiple trauma severe head injury) because of the high trauma mechanism of injury. Open reduction and internal fixation are recommended for treating traumatic hip dislocation associated with transphyseal femoral head fracture. Open reduction and internal fixation were the treatment in 34 of the cases. Due to multiple traumas and a severe head injury, one patient received closed reduction and cast immobilization as part of their treatment.
The type of dislocation determines the approach for open reduction. The posterior approach was the one used the most frequently (14 cases). The posterolateral approach was used in nine patients, the anterior approach in four, the lateral approach with greater trochanteric osteotomy in four and the anterior approach in two patients. Avascular necrosis was the most common complication after traumatic hip dislocation and transphyseal femoral head fracture, affecting 31 patients. AVN did not occur in four patients; Three of them were treated with greater trochanteric osteotomy and open reduction through a lateral approach. After a traumatic hip dislocation associated with transphyseal femoral neck fracture, 88.57% of patients developed osteonecrosis. Head subluxation (two patients), physeal closure (one patient), chondrolysis (one patient), and septic arthritis (one patient out of the 31 patients with AVN) were additional complications. The fastest onset of AVN was 2 months and the latest was 72 months.
Case Report
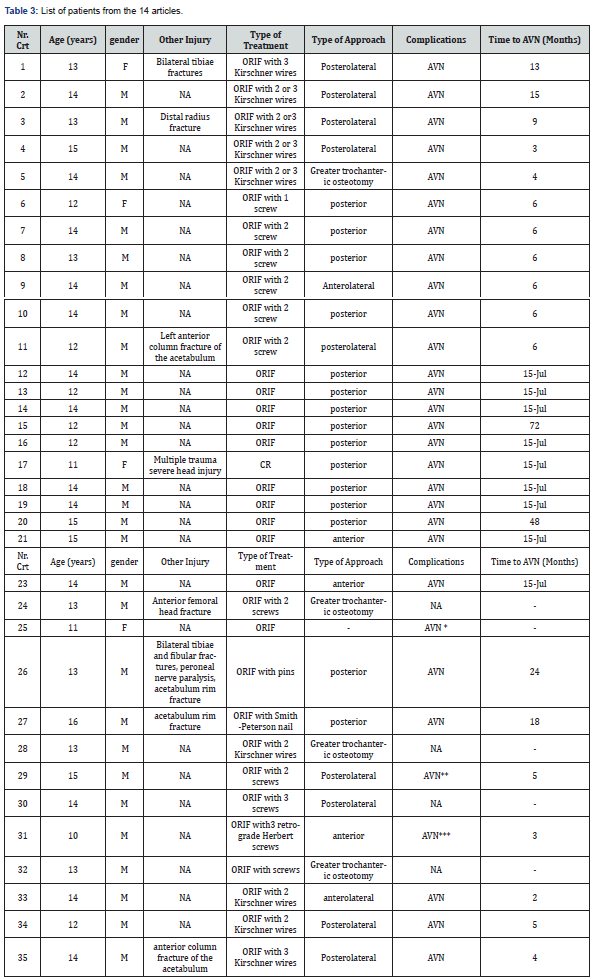
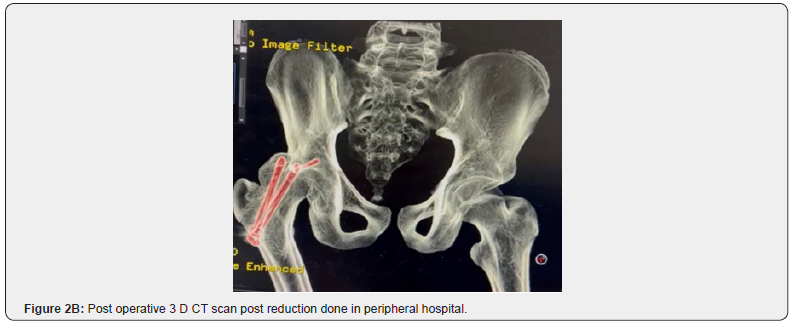
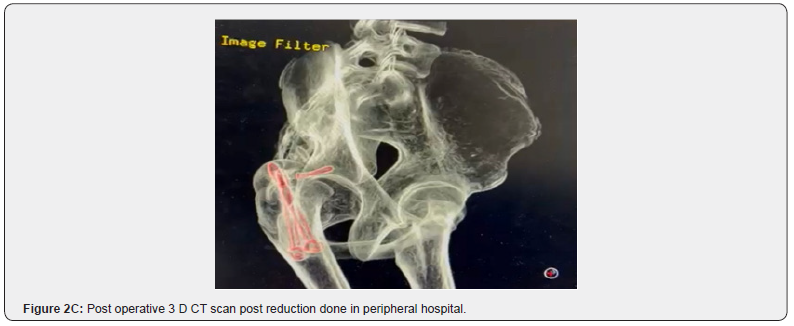
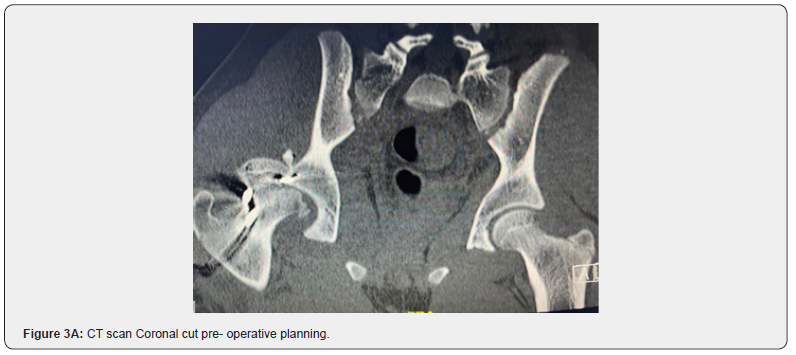
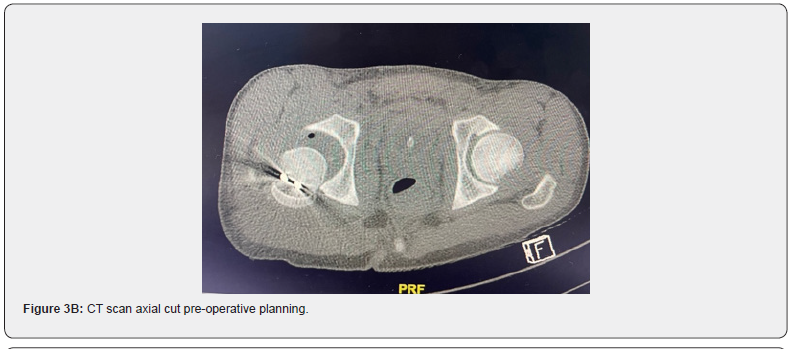
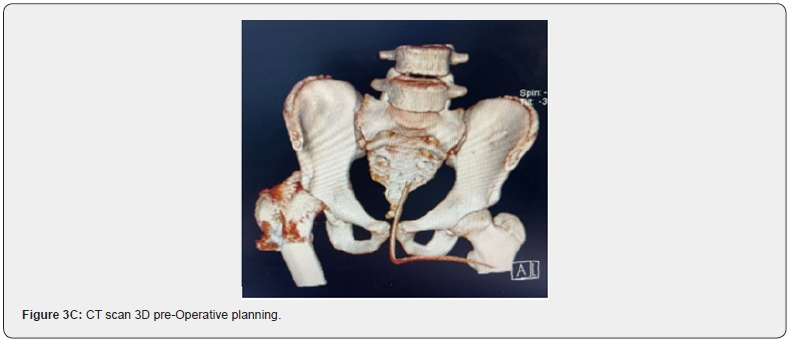
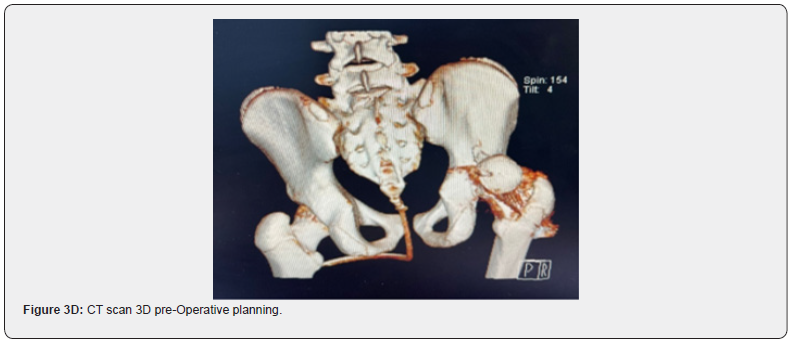
15 years old boy medically free case of road traffic accident (RTA) sustained right distal radius fracture which reduced and treated conservatively and right hip posterior dislocation, three trails of reduction in peripheral hospital result in iatrogenic transphyseal proximal femur fracture dislocation. Treated surgically by cannulated screws but still dislocated. We received this patient in our hospital as an emergency case, planned and operated on the next day. Upon arrival deep history was taken, patient was victim of RTA, he was the driver with unknown speed, not ejected from the car, no role over. lost conscious for seconds then he brought by ambulance to the peripheral hospital that treated in emergency department by successful reduction of right distal radius and 3 filed trails of reduction right posterior hip dislocation which complicated with iatrogenic transphyseal proximal femur fracture and dislocation (Figure 1). And then pushed as emergency case to operative room. As reported, they go through posterior approach and reduction of proximal femur fracture done and fixed with two cannulated screws 7.5 mm and posterior acetabulum wall reduced with cannulated screw 3.5 mm (Figure 2). Then transferred to our hospital the next day. The secondary survey done, patient was stable vitally conscious and alert. Head to toe examination done, right upper limb below elbow full cast with intact neurovascular examination otherwise unremarkable head, neck and both upper limbs.



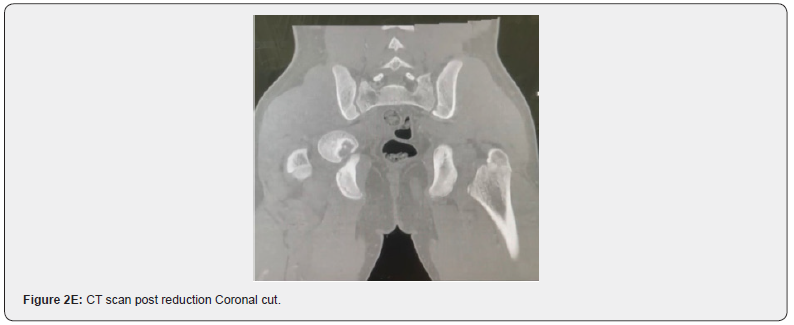
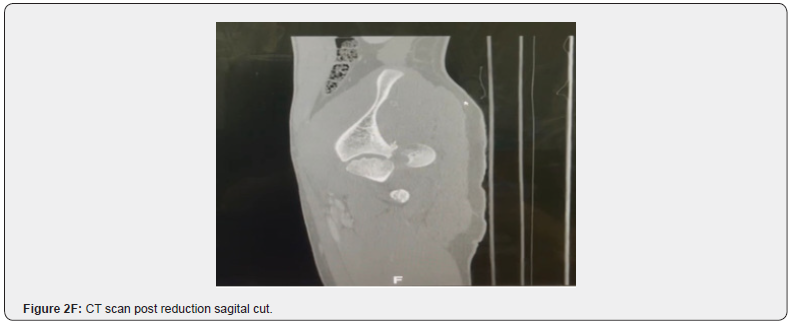
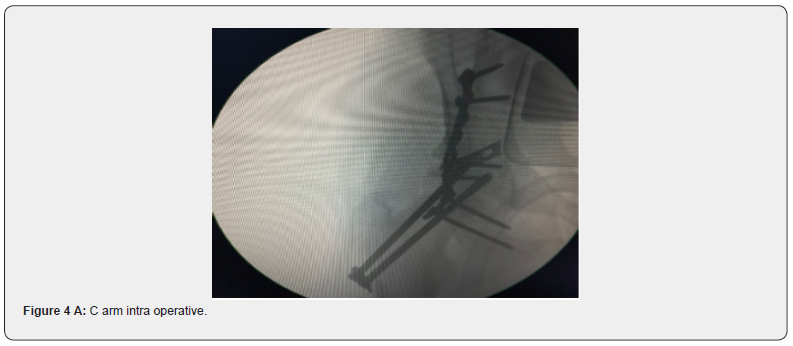
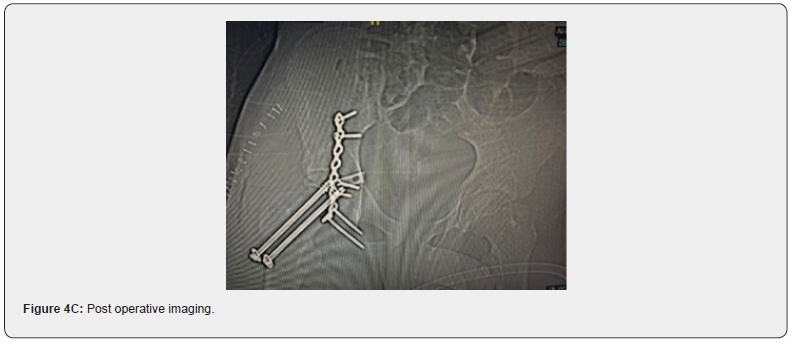
The lower limb was unremarkable except for the lower limb shortened and adducted and internally rotated. There was a right foot drop with intact vascular examination. skin traction applied and CT and full lab was ordered and planned then booked for emergency open reduction and internal fixation right hip in the next day (Figure 3). Patient brought to holding area consented and marked and pushed to operative room on supine position over translucent table under general anesthesia and using C arm, preb and dreb in sterile manner then throw previous scar posterior approach to right hip done and deep careful dissection applied , sciatic nerve identified and protected and then wash done and reduction done to right hip then small screw removed from posterior wall of acetabulum and then reduction of the posterior wall with two plates one as hook plate and the other one as buttress plate then two suture anchor applied to repair the capsule, stability achieved, c arm confirmation done then wash and closure layer by layer and then skeletal traction applied with weight six kg and wound swab was taken from surgical site for culture and sensitivity and sterile dressing done .Patient tolerated procedure well then transferred to recovery in good condition (Figure 4). Post operative examination patient had stable hip, pain controlled and vascular examination intact. there was foot drop. Post-operative non weight bearing and hemoglobin within normal range and pain tolerated and started on antibiotics and culture was negative. skeletal traction removed after two weeks and physiotherapy bed to chair then toe touch. discharged home after three weeks for follow up. Patient seen in clinic with stable hip and improving with physiotherapy.

Discussion
In the pediatric population, traumatic hip dislocations are a rare injury and account for less than 5% of all dislocations [17]. Hip dislocations are occasionally associated with minor trauma in younger children; however, as age increases toward adolescence, major trauma is almost always required [18]. In children and adolescents, posterior dislocations account for nearly all traumatic hip dislocations, just like they do in adults. Obturator dislocations have been reported very rarely [19,20]. The incidence of avascular necrosis of the femoral head following a traumatic hip dislocation in the pediatric population ranges from 3 to 15 percent [21-23]. A few cases of adolescents with traumatic hip dislocations and physeal separation (epiphysiolysis) of the proximal femur have been reported. In these patients, the rate of AVN is close to 100%. Many of the patients in these series had posterior dislocations, and epiphysiolysis has been reported both at the time of injury, [23-25] and because of attempted reduction, [18-26]. None of them had an obturator dislocation, as the patient we present here in article. Many agree that reduction with complete muscle relaxation may play a role in preventing iatrogenic epiphysiolysis in adolescents with hip dislocations. The likelihood of epiphysiolysis can be decreased by using general anesthesia and gentle intraoperative reduction to lessen the force exerted on the growth [18-26]. Herrera-Soto et al. Also recommend reduction under fluoroscopy so that the epiphysis can be stabilized and any early signs of physeal instability can be found [27]. The patient in our research suffered from an extraordinarily uncommon injury - irreducible trans obturator hip dislocation - that has only ever been documented in adult patients [28,29]. Prior to transfer, he had many reduction efforts at a different location, as well as a closed reduction attempt while under general anesthesia at our facility.
The proximal femoral physis may have been destabilized by previous attempts. Interestingly, while our patient's epiphysis moved during open reduction, all reports of epiphysiolysis during hip reduction occurred during closed reduction attempts. Clinicians should be aware of the possibility of epiphysiolysis during any difficult reduction of a traumatic hip dislocation in an adolescent patient, regardless of the dislocation's direction, based on this case and previous reports. Under fluoroscopic guidance and general anesthesia, these should be reduced. Before making any attempts at reduction, surgical stabilization of the epiphysis should be considered if there is any fluoroscopic evidence of Physeal instability or if the reduction is difficult. When it is difficult to determine the position of the femoral head on plain radiographs, adolescents with obturator hip dislocations may benefit from a prereduction CT scan. Prior to closed or possible open reduction, transphyseal fixation should be considered if the femoral head is intrapelvic.
Conclusion
Traumatic hip fracture dislocation is uncommon in children and may present with a mechanism that seems insignificant. The clinical condition is a true orthopedic emergency regardless of age, and closed reduction should be performed under sedation or general anesthesia as soon as possible to prevent avascular necrosis, post-traumatic arthritis, and long-term morbidity. Serious level of doubt joined with right on time and brief decrease is the cornerstonein the management: X-rays are required for ongoing follow-up, and treatment can be stopped until skeletal maturity. A vascular necrosis of the femur head and an increased risk of an iatrogenic fracture are both increased by multiple hip reduction attempts. We recommend a single trial reduction, and if that fails, we should push the patient to be reduced intraoperatively. Good preoperative planning and congruent reduction should be followed by a suitable fixation. We suggest that a stable fixation and closure of the capsule and the labrum will give a good result and increase the stability of hip joint.
Human Ethics
Consent was obtained by all participants in this study.
Foot Notes
The author reports that he has no conflicts of interest in the authorship and publication of this article.
References
- Zakry M, Mahmoodi MS, Saad G, Morgan M (2012) Traumatic anterior dislocation of hip in a teenager: An open unusual type. Eur J Orthop Surg Traumatol 22(1): 99-101.
- Ba saran SH, Bilgili MG, Erçin E, Bayrak A, Ones HN (2014) Treatment and results in pediatric traumatic hip dis-location: Case series and review of the literature. Ulus Travma Acil Cerrahi Derg 20(6): 437-442.
- Cytodeme M, Aydin D, Ozcan M, Copuroglu C (2014) Traumatic posterior hip dislocation and ipsilateral distal femoral frac-ture in a 22-month-old child: A case report. J Pediatr Orthop 23(6): 544-548.
- Bressan S, Steiner IP, Shavit I (2013) Emergency department diagnosis and treatment of traumatic hip dislocations in children under the age of 7 years: A 10-year review. Emerg Med J 31(5): 425-431.
- Herrera-Soto JA, Price CT (2009) Traumatic Hip Dislocations in Children and Adolescents: Pitfalls and Complications. J Am Acad Orthop Surg 17(1): 15-21.
- Barquet A, Vécsei V (1978) Traumatic dislocation of the hip with separation of the proximal femoral epiphysis. Arch Orthop Trauma Surg 103(3): 219-223.
- Herrera-Soto JA, Price CT, Reuss BL, Riley P, Kasser JR (2006) Proximal Femoral Epiphysiolysis During Reduction of Hip Dislocation in Adolescents. J Pediatr Orthop 26(3): 371-374.
- Odent T, Glorion C, Pannier S, Bronfen C, Langlais J (2003) Traumatic dislocation of the hip with separation of the capital epiphysis: 5 adolescent patients with 3-9 years of follow. Acta Orthop Scand 74(1): 49-52.
- Shaath MK, Shah H, Adams MR, Sirkin MS, Reilly MC (2018) Management and Outcome of Trans epiphyseal Femoral Neck Fracture-Dislocation with a Transverse Posterior Wall Acetabular Fracture: A Case Report. JBJS Case Connect 8(3): e64.
- Palencia J, Alfayez S, Serro F, Alqahtani J, Alharbi H (2016) A case report of the management and the outcome of a complete epiphyseal separation and dislocation with left anterior column fracture of the acetabulum. Int J Surg Case Rep 23: 173-176.
- Mandell JC, Marshall RA, Weaver MJ, Harris MB, Sodickson AD (2017) Traumatic Hip Dislocation: What the Orthopedic Surgeon Wants to Know. Radiographics 37(7): 2181-2201.
- Gautier E, Ganz K, Krügel N, Gill T, Ganz R (2000) Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Jt Surgery Br 82(5): 679-683.
- Shrader MW, Jacofsky DJ, Stans AA, Shaughnessy WJ, Haidukewych GJ (2007) Femoral neck fractures in pediatric patients: 30 years experience at a level 1 trauma center. Clin Orthop Relat Res 454: 169-173.
- Ogden AJ (1981) Hip development and vascularity: Relationship to chondro-osseous trauma in the growing child. Hip 139-187
- Kennon JC, Bohsali KI, Ogden JA, Ogden J, 3rd Ganey TM (2016) Adolescent Hip Dislocation Combined with Proximal Fem-oral Physeal Frac-tures and Epiphysiolysis. J Pediatr Orthop 36(3): 253-261.
- Tevanov I, Enescu DM, Carp M, Dusca A, Ladaru A (2018) Negative pressure wound therapy in reconstructing ex-tensive leg and foot soft tissue loss in a child: A case study. J Wound Care 27 (Sup6): S14-S19.
- Sink EL, Kim Y (2015) Fractures and Traumatic Dislocations of the Hip in Children. In: Rockwood and Wilkins’ fractures in children 8th Wolter Kluwer Philadelphia pp. 974
- Herrera-Soto JA, Price CT (2009) Traumatic hip dislocations in children and adolescents: pitfalls and complications. J Am Acad Orthop Surg 17(1): 15-21.
- Durand Y, Bruyere C, Saglini M (2018) Traumatic obturator hip dislocation in a 15-year-old adolescent: A high-energy trauma Report of a case. In SWISS MEDICAL WEEKLY148, pp.60S-60S.
- Avery D M, Carolan G F (2013) Traumatic obturator hip dislocation in a 9-year-old boy. Am J Orthop 42(9): 81-83.
- Barquet A (1979) Traumatic hip dislocation in childhood: a report of 26 cases and a review of the literature. Acta Orthopaedica Scandinavica 50(5): 549-553.
- Mehlman C T, Hubbard G W, Crawford A H (2000) Traumatic Hip Dislocation in Children: Long-Term Follow up of 42 Patients. Clin Orthop Relat Res 376: 68-79.
- Offierski C M (1981) Traumatic dislocation of the hip in children. J Bone Joint Surg Br 63(2): 194-197.
- Kennon Justin C, Bohsali KI, Ogden JA (2016) Adolescent hip dislocation combined with proximal femoral Physeal fractures and epiphysiolysis. J Pediatr Orthop 36(3): 253-261.
- Barquet A, Vecsei V (1984) Traumatic dislocation of the hip with separation of the proximal femoral epiphysis. Archives of orthopaedic and traumatic surgery 103(3): 219-223.
- FiddianN J, and D L Grace (1983) Traumatic dislocation of the hip in adolescence with separation of the capital epiphysis. Two case reports. J Bone Joint Surg Br 65(2): 148-149
- Herrera-Soto J A, Price C T, Reuss BL (2006) Proximal femoral epiphysiolysis during reduction of hip dislocation in adolescents. J Pediatr Orthop26(3): 371-374.
- Rancan M, Esser M P, Kossmann T (2007) Irreducible traumatic obturator hip dislocation with subcapital indentation fracture of the femoral neck: a case report. Journal of Trauma and Acute Care Surgery 62(6): E4-E6.
- Kenan S, Stein S, TrasoliniR (2018) Iatrogenic Obturator Hip Dislocation with Intrapelvic Migration. Case Rep Orthop 2018: 5072846.






























