From Disaster to Triumph: How a Professional Basketball Team Becomes Injury - Free Implementing a Revolutionary Proactive Approach to Injuries
Tim Maggs1, Steven Brownstein2* and Alexandros Siozos3
1DC, Director, Maggs Sports Chiropractic Biomechanics and Wellness Center Director, Sports Injuries and Biomechanics, USA
2MD, Radiologist, Medical Director of Dynamic Medical Imaging, Medical Director of Spinal Kinetics, LLC Union, USA
3MD, Consultant in Orthopaedic Surgery, Private Practice, Kozani, Greece
Submission: July 27, 2023; Published: August 10, 2023
*Corresponding author: Steven Brownstein, MD, Radiologist, Medical Director of Dynamic Medical Imaging, Medical Director of Spinal Kinetics, LLC Union, USA
How to cite this article: Tim Maggs, Steven Brownstein* and Alexandros Siozos. From Disaster to Triumph: How a Professional Basketball Team Becomes Injury - Free Implementing a Revolutionary Proactive Approach to Injuries. Ortho & Rheum Open Access J. 2023; 22(1): 556080. DOI: 10.19080/OROAJ.2023.22.556080
Introduction
This is a case study looking at two completely different sports medicine approaches in back-to-back years of the Albany Patroons, a professional basketball team. When the team resorted to the traditional “reactive” sports medicine approach in 2022, the season was filled with x-rays, MRI’s and injury treatment. In contrast, 2023 adapted and utilized The Structural Management® Program (an advanced injury prevention program) which is based on Dr. Maggs℠ Law of Tissue Tolerance: When the loading of a tissue exceeds the capacity of that tissue, compensatory physiological changes occur. The Structural Management® Program identifies and addresses tissue tolerance deficiencies. The result was a near injury-free season. This study will review these details.
The Background
All pro sports have major injury issues, but no sport suffers injuries quite like football and the NFL. It’s no surprise then that an estimated $521 million was spent on sidelined players in the 2019 season according to a study by The Associated Press [1]. And while some degree of injury prevalence is expected in a sport characterized by extreme physical contact and raw force, the number is simply staggering considering it reflects only one sport during one season in the U.S. alone. Furthermore, the 2022 regular season saw nearly $800M in salaries paid to players while they were inactive due to injuries [2]. When we look at baseball players, the findings are similar. Major League Baseball teams lost an average of 961 man-games due to injuries in 2016. The average player salary in MLB is just over $4 million. Therefore, teams lost an average of $26 million last year in salaries alone paying injured players who could not play [3]. The NBA has an astronomical economic burden from paying the salaries of sidelined players as well [4]. In the year 2021-2022 the top 10 teams spent more than $443M on injuries, as presented in the chart below (Figure 1).
All leagues and teams, not only in the US but worldwide, have been using the reactive sports medicine approach to players’ injuries for decades. People may ask why, when every other industry in the world uses the words prevention and maintenance with an “Of course” response. Money and injuries have governed the significant growth of the sports medicine industry. Factors in that growth are political lobbying by the medical field, insurance guidelines, pharmaceutical and surgical profits, “because this is the way it’s always been done”, and a reluctance to find a better way. The reason these leagues don’t invest in prevention and maintenance is because no program before Structural Management® has ever existed. The field of applicable biomechanics spends research dollars on things like robotics, orthoses materials and Matrix-like exoskeleton suits costing more than 100,000 USD each [5]. To date, however, prior to the development of The Structural Management® Program, no one had ever thought about the preservation of the human structure or looking at the human being as an architectural structure which is greatly affected by gravity, aging, and biomechanical imbalances. These factors only add to the fact that all humans are born with biomechanical imbalances. Our prior studies [6] have proven that all people have biomechanical imbalances and faults, and today’s sports medicine industry never looks at or finds these faults. They treat the injuries caused by these faults.
From Disaster to Triumph
A new coach was hired at the beginning of the 2022 season. Unfortunately, the coach came from a Division 1 Program which tends to have close relationships with the orthopedists and athletic trainers who are the main providers of traditional sports medicine. His preference was to retain the personnel he was familiar with, despite the fact we were the team’s Drs. The outcome was a season filled with injuries, increased reactive x-rays and MRI’s and many lost games by injured players. At the beginning of the 2023 season, the coach from the 2020 season was re-hired. This provided a unified goal between the coaching department and the sports medicine department, which is important for success in sports today. This set the stage once again for The Structural Management® Program to be implemented beginning the day players arrived at camp. On Day 1, all players received a Structural Fingeprint® Exam that included a physical exam, biomechanical x-rays, and a digital laser foot scan. We ordered orthotics for all players, and when the orthotics arrived, we inserted them into the players’ shoes and re-took the A-P L-S x-ray for comparison. The year proved to be an incredibly successful year with regards to injury prevention, as only one player missed two games due to injury. This produced an environment of momentum and greater team camaraderie, as few mid-season adjustments were needed as team adjustments due to injuries tend to throw off both team chemistry and team rhythm.

Materials and Methods Part I: Disaster (The 2022 Season)
There was little to no communication between the coaching staff and the sports med department. The season started in crisis. There were no pre-season evaluations and pre-season try-outs started at a conditioning level most players were not prepared for. Two players came into us the first couple days with pulled muscles and sprained ankles. A third player, 6’8”, was described as lying in his hotel room crying in the fetal position with severe leg cramps. As soon as he could stand, he was brought in for treatment.
A secondary complication was our relationship with the MRI facility which normally sponsored the team and provided MRI’s at no charge. They anticipated that with the approach this coach was taking that more players would be injured and more MRI’s would be needed. They weren’t willing to sign on for that relationship. When we approached the coaching staff with this issue, they assured me their MRI personnel would provide all necessary testing. We quickly learned their MRI personnel were not going to provide testing at no cost (as our prior sponsors did). This produced complications as we had multiple knee injuries that could have been ACL tears, and without the MRI, we couldn’t definitively diagnose the injury so we couldn’t know if the player should stay or go home. The year played out with many players coming in with acute injuries. Injuries produce stress. The rotations were continually altered, the team camaraderie was weakened and ultimately, the last game was lost due to team controversy related to injuries that had occurred during the season.
Materials and Methods Part II: Triumph (The 2023 Season)
There was full communication and a plan between the coaching staff and the sports med department before the season began. The day players arrived at camp it was agreed that evaluations would be set up and a full screening would be performed. Architectural or biomechanical asymmetries were identified, and corrective measures were taken. A proactive treatment regime was set up for each player based on the findings from their screenings and prior history of injuries.
The primary test that was performed was The Dr. Maggs℠ Leg Length Test, which consists of 3 tests. The first test was a digital laser foot scan to detect any collapsing of the arches of the feet, as well as the percentage of body weight loading, left vs. right. The second test is then a standing A-P L-S digital x-ray of the patient while barefoot. An A-P L-S x-ray is the third test taken one week later when the patient received and inserted their orthotics into their shoes.
The Dr. Maggs℠ Leg Length Test is part of the broader Structural Fingeprint® Exam (SFE) which is a leading full biomechanical examination. This examination consists of a consultation to document injury history, physical examination, digital laser foot scan and 2 standing x-rays of the low back (A-P and lateral) and 2 standing x-rays of the neck (apom and lateral). These are all taken while the patient is barefoot. While positioning the patient to take the A-P L-S x-ray, either with shoes on or barefoot, the central ray was 1” below the umbilicus at 40” from the tube. The normal central ray is the umbilicus, but 1” below the umbilicus reduces magnification or distortion of the femoral heads producing a more accurate measurement.
We ordered orthotics for all players and when the orthotics were delivered, we inserted them into their shoes and took x-ray #2. If the femoral head height difference (fhhd) was greater than 3mm, we placed an appropriately sized lift underneath the orthotic on the “low” femoral head side. Once this was completed, we set up appointments of 1-3 times/week for each player to receive treatments. In our second published study [7], 60% of patients required a lift after orthotics were put into their shoes due to a fhhd >3mm. With this team of 11 players, 8 of 10 players were greater than 3mm and therefore required a lift. One player never received his second x-ray and therefore we never considered a lift for him.
Once the orthotics and lifts were in place, we focused on areas of prior injury or areas of soreness, tenderness and normal compression that occurs in athlete’s low backs. We performed chiropractic adjustments on every visit for every player, used cold laser therapy on any areas of soreness, bruise, strain, or inflammation and spinal decompression for the lumbar spine on every player every visit.
Results
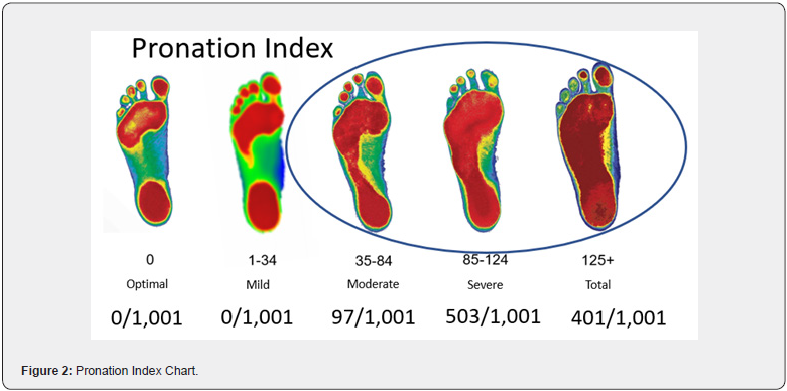
In April 2023 we published the results of a study of 1,001 patients who had their feet scanned with our digital laser scanner [8]. Based on the amount of collapse in each foot, each patient’s scan would provide a number reflecting their degree of collapse (Figure 2). There were 5 categories: optimal arches (0), mild pronation (1-34), moderate pronation (35-84), severe pronation (85-124) and total pronation (125+). Our results showed there were no patients with optimal feet. There were no patients with mild pronation. There were 97 patients with moderate pronation, 503 with severe pronation and 401 with total pronation.
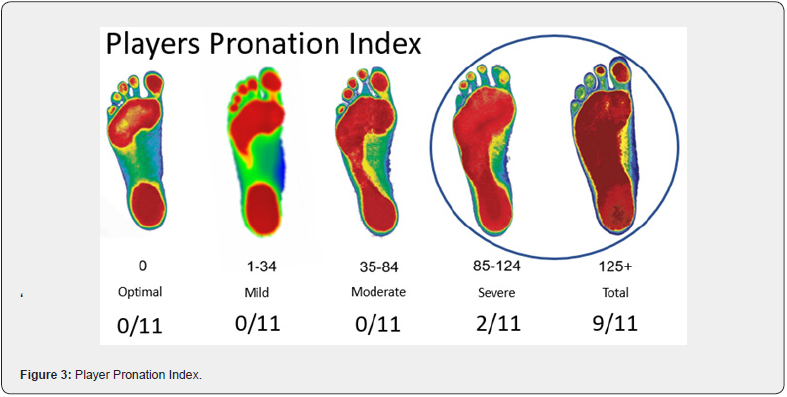
Our players’ results were worse than the results of the above referenced study. No player had optimal feet. No player had mild pronation. No player had moderate pronation. 2 players had severe pronation and 9 players had total pronation (Figure 3).
In 2020 we also published a study of 351 patients [6]. Our initial premise was that everyone is Crooked Man℠. Everyone has biomechanical faults at birth and these faults only worsen over one’s lifetime. We performed The Dr. Maggs℠ Leg Length Test on each patient, and we learned there are 5 unique Crooked Man℠ patterns and every human is one of these 5 patterns (Figure 4).
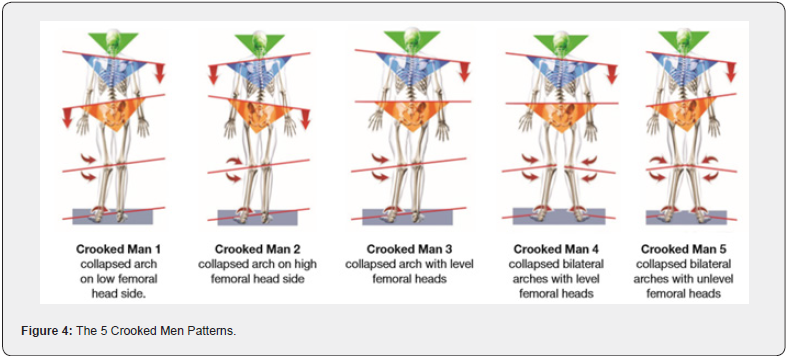
The study of 351 subjects produced the following results:
Crooked Man 1: 42% (148/351)
Crooked Man 2: 16% (56/351)
Crooked Man 3: 6% (21/351)
Crooked Man 4: 16% (56/351)
Crooked Man 5: 20% (70/351) [6]
When we completed this test on our 11 players, the results were:
Crooked Man 1: 2 players
Crooked Man 2: 2 players
Crooked Man 3: 1 player
Crooked Man 4: 2 players
Crooked Man 5: 3 players
Unknown CM: 1 player never had 2nd x-ray taken.
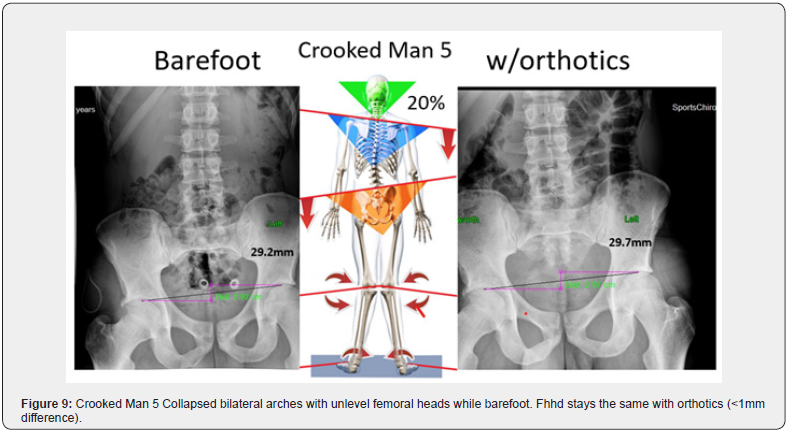
Here are actual pre-and post- x-rays of 5 players depicting Crooked Man 1-5 (Figures 5-9).
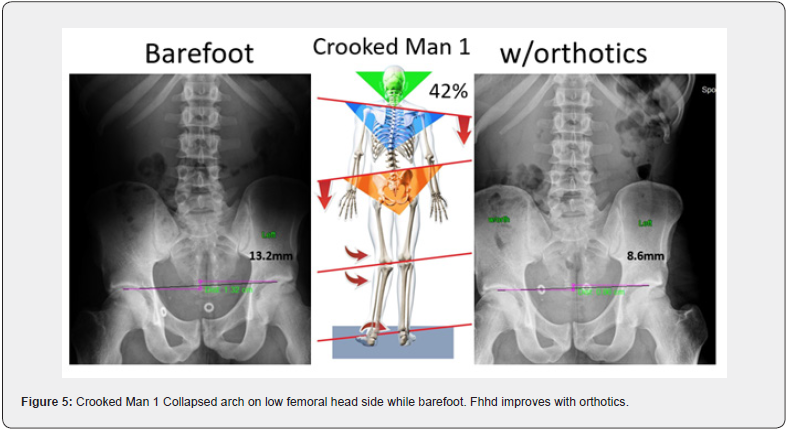
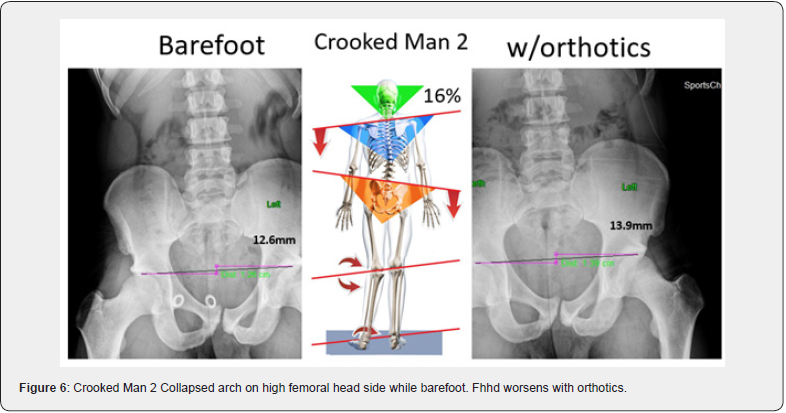
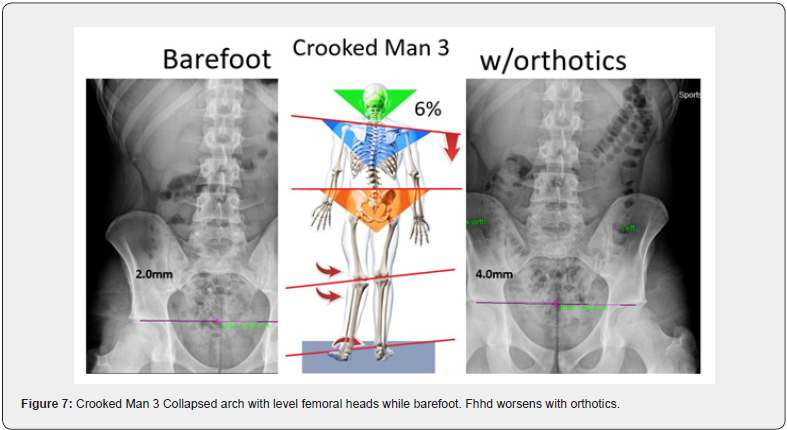
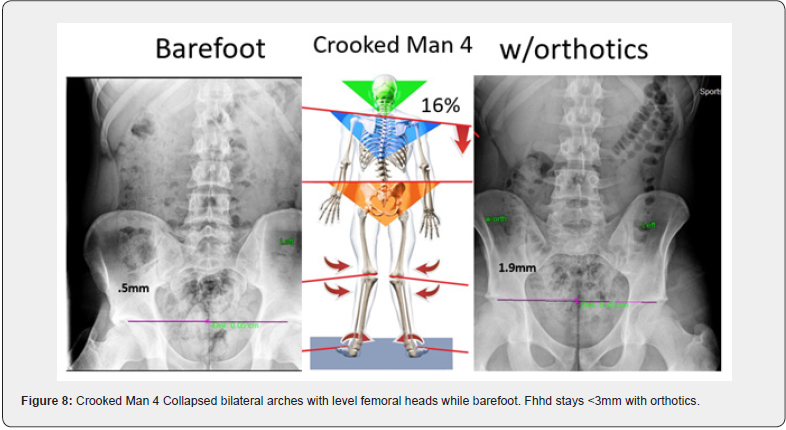
Studies have not been done yet to determine if clinically one pattern is more injury prone than another, but anecdotally, patients presenting as Crooked Man 2 have presented with the most and worst injuries over the past 5 years. However, by determining which Crooked Man an individual is and what mm difference there is when x-raying for femoral head height with orthotics in the shoes, you have a more specific understanding of the amount of lift that is needed under the low femoral head side. Improving balance and weight distribution and increasing tissue tolerance is a major goal for injury prevention.
In addition to the above biomechanical corrections made with orthotics (and lifts where needed) on the 2023 team athletes
Discussion
At the time of writing this study, it is believed that no professional team either in the U.S. or abroad, has systematically implemented an effective proactive approach in the sports medicine department of their team. The goal is always the same for every team—fewer injuries. The approach, however, is grossly different. All sports medicine today is reactive in nature. The athlete must be hurt for the attending physician or therapist to apply their diagnostic and therapeutic knowledge. No biomechanical preseason evaluations are performed on athletes to make quantifiable corrections that will dramatically lower injury incidence. No one looks at the feet of an athlete from an architectural perspective and how this very foundation of the body relates to the body’s 2nd foundation, the femoral head heights. When these findings are ignored, every athlete is participating with imbalances in one or more of the following: foot pronation, knee rotation, tibia torsion and alignment, leg length, pelvic rotation, mechanical axis, and centers of gravity. This creates significant imbalances in joint, tendon, muscle and bone loading, and added to repetitive activity and/or prolonged activity, leads to premature injuries.
The cost of injuries will continue to rise in the future for several reasons. First, salaries are escalating at a rate never before seen. A player lost for one year is exorbitantly more expensive than any prior time in history. Young athletes are beginning younger, are playing more year-round games, they’re in the weight rooms much earlier and their musculoskeletal systems have aged well beyond their chronological age, all prior to making it to the pros. There is also an absence of biomechanical evaluations and corrections for younger athletes. Finally, until someone breaks through the ranks of sports medicine providers, from physicians to therapists to athletic trainers, who can work biomechanically and proactively, the escalating costs will continue. Ironically, the only injury suffered in 2023 was to the player that we did not get a 2nd x-ray on and therefore, had no lift on his orthotic, nor did we learn which Crooked Man he was. On his barefoot x-ray, his femoral head height difference was 17.2mm, so there’s no doubt he would need a lift which would have been put on after his 2nd x-ray. He hyperextended his knee and missed the last 2 games. This may be coincidence, or it may endorse the incredible value of the Structural Management® Program.
Conclusion
We can now speak with a high degree of certainty that The Structural Management® Program, when used diagnostically and therapeutically for an entire season, can significantly reduce player injuries and team costs. For this program to succeed, everyone in an organization must be supportive. From the owners to the rest of the medical staff, to the coaching staff and even to those who help transport the players, everyone must be a contributor to this program. If the program were only used in part, we suspect the outcome would be positive, but only in part.
This program that started 30 years ago while working in the New York Giants strength department when it was recognized the reactive approach is applied only after a player was injured. The results of this study are exactly what was needed to prove the value of proactive treatment of structural imbalances. It is with great optimism that other teams, leagues and management groups will recognize the importance and significant cost effectiveness of being proactive and addressing the biomechanics of the athlete which currently is largely ignored.
18 years ago, The Concerned Parents of Young Athletes℠ Program (CPOYA) was developed to raise the awareness of biomechanics in the middle and high school population and to begin to make changes before breakdown occurs. We now have an office in Christian Brothers Academy in Albany, New York, performing Structural Fingerprint® Exams on all interested students at no charge and providing weekly treatment (in school) to those students who have gone through the exam. The hope is that this model will be recognized and begin to appear in all schools throughout the country and that either The Structural Fingerprint® Exam or The Dr. Maggs℠ Leg Length Test will become standard yearly exams pre-season for all students.
References
- Gary Philips (2020) Injuries Cost NFL Teams Over $500 Million In 2019 by Gary Philips.
- Daniel Parris (2023) What’s the true cost of NFL injuries? A Statistical Analysis. Do injuries dictate NFL season outcomes? Stat Significant.
- Major League Baseball: Cost of injuries in wins, dollars and final standings (2017).
- The Cost of Injuries to NFL and NBA Players Revealed (2022).
- Katleho Limakatso (2023) Exoskeletons: Costs and where to buy one.
- Tim Maggs D, Steven B M, Alexandros S M (2020) When Correcting the Collapse of Arches of the Feet with Custom Orthotics, are Other Areas of the Body Effected? A Revolutionary Approach towards Reduced Injuries and Better Outcomes. Ortho & Rheum Open Access J 17(1): 555953.
- Tim Maggs, Steven B, Alexandros S (2021) Is Prescribing Custom Orthotics Enough to Prevent and Treat Musculoskeletal Injuries and Degeneration? What if we Integrated Biomechanical X-ray Measurements with the Laser Foot Scan Procedure? Could this Reduce Injuries Even More? Ortho & Rheum Open Access J 17(4): 555970.
- Tim Maggs D, Steven B M, Alexandros S (2023) M Each Person’s Collapse of the Arches of the Foot May Be Unique, but its Correction is Standard. A Large Study Explains Why. Ortho & Rheum Open Access J 21(4):






























