Delayed Allograft Reconstruction and Heterotopic Bone Excision of Chronic Neglected Patella Tendon Avulsion in an Adolescent
Peter T Simonian* and Taylor L Simonian
Simonian Sports medicine Clinic, Clovis, USA
Submission:May 14, 2023; Published:May 24, 2023
*Corresponding author: Peter T Simonian, Clinical Associate Professor, University of Washington, Department of Orthopaedic Surgery and Sports Medicine, Simonian Sprots Medicine Clinic 729 N Medical Center Drive West, Suite 101 Clovis CA, 93611, USA
How to cite this article: Peter T Simonian, Taylor L Simonian. Delayed Allograft Reconstruction and Heterotopic Bone Excision of Chronic Neglected Patella Tendon Avulsion in an Adolescent. Ortho & Rheum Open Access J. 2023; 21(5): 556072. DOI: 10.19080/OROAJ.2023.21.556072
Introduction
Complete patella tendon tears and avulsions are typically treated with acute surgical intervention to maintain function of the extensor mechanism of the knee. It is rare for such injuries to be neglected because of the significant disability in quadriceps function associated with complete injuries of the extensor mechanism. Further, delayed heterotopic ossification appears to be a potential complication of conservatively treated patella tendon injuries in adolescents before skeletal maturity [1].
Heterotopic ossification is a process that results in the formation of mature lamellar bone in tissues other than bone, including muscle, tendon, ligament, vascular, and neural [2]. We have identified 3 cases of heterotopic ossification of the patella tendon after rupture [1,3]. All 3 cases were male and involved injury to the patella tendon as an adolescent, one at 13 years old and two at 15 years of age. All three patients were treated with heterotopic bone excision and subsequent patella tendon reconstruction. Two were reconstructed with a synthetic Leeds-Kio ligament [1]. The third was repaired and augmented with a semitendinosus autograft [3], utilizing a technique similar to what we have previously described [4].
The 2 cases described by Matsumoto et al. [1], were immobilized in a straight leg cast at the time of their initial injury and then many years later (one 40 years and the other 6 years) presented with disability with patella alta and heterotopic ossification and underwent corrective surgical intervention. After surgery, one patient had a range of motion (ROM) of 10 to 130 degrees with an Insall-Salvati ratio of 1.4 and the other had other had full range of motion with an Insall-Salvati ratio of 1.0.
The third case described by Supreeth et al. [3], was treated in a more acute fashion. It is uncertain when the initial injury occurred, but the patient was presented at the age of 13 years old with dysfunction, patella tendon disruption, patella alta and heterotopic ossification. Patella tendon repair and reconstruction with semitendinosus autograft was immediately performed. The patient regained full active ROM with no extensor lag.
We present a case of a 22-year-old male with documented complete patella tendon disruption at the age of 16 years. The injury was completely neglected until the patient sought treatment 6 years later. The patient was presented with symptoms related to a dysfunctional extensor mechanism with mature heterotopic ossification of nearly the entire patella tendon and severe patella alta. The patient underwent large posterior tibialis allograft reconstruction with suture and anchor augmentation (internal brace) after heterotopic ossification excision, 6 years after neglected injury.
Case Report
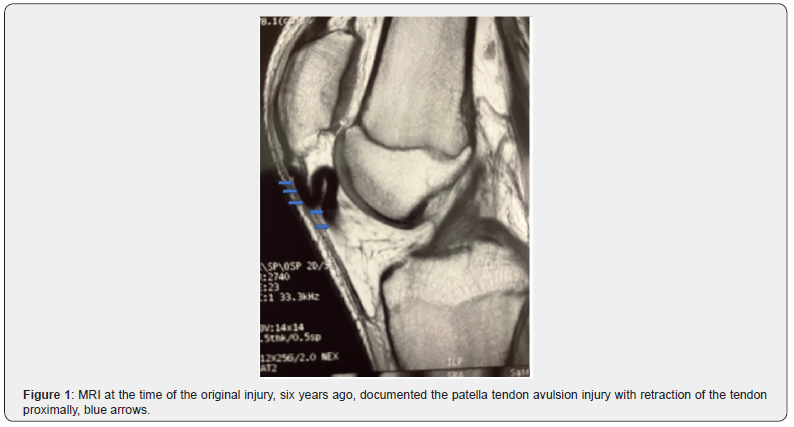
A 22-year-old male presented with disability, weakness, giving-way, pain after sustaining a documented left patella tendon avulsion from the tibial tubercle 6 years earlier at the age of 16 years. He was playing basketball and came down awkwardly on the left knee after performing a lay-up. At the time of the injury, the patient was seen in the emergency room and diagnosed with a complete avulsion of the patella tendon. MRI at the time of the original injury, six years ago, documented the patella tendon avulsion injury with retraction of the tendon proximally, blue arrows (Figure 1) as well as disruption of the medial retinaculum. It was a pure tendon avulsion with no bone or cartilage attached. There was no evidence of heterotopic ossification at that time. He did not seek orthopedic consultation secondary to being uninsured. The patient had no further treatment until a recent presentation to our clinic six years later.
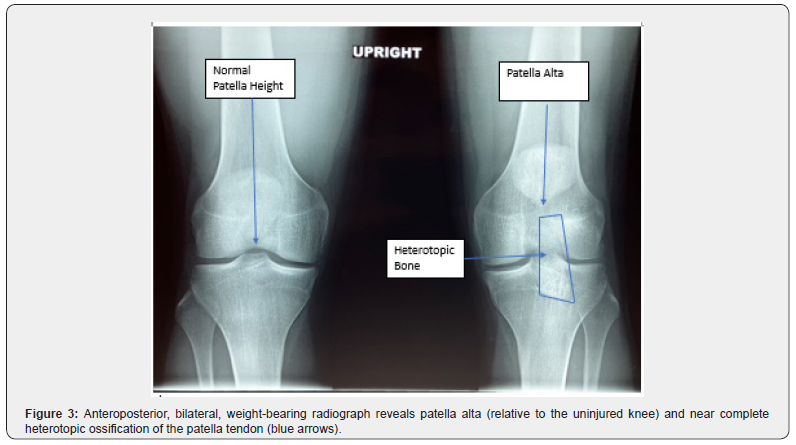
Upon presentation to our clinic six years later, the patient complained of ongoing weakness, pain, giving way, and the inability to run or participate in sports. On physical examination, the patient was found to have patella alta, a 20-degree extensor lag, atrophy of the quadriceps, and solidification of the patella tendon on the affected extremity. Interestingly, knee flexion was symmetric to the opposite extremity. Radiographs revealed patella alta and near complete heterotopic ossification of the patella tendon (Figures 2 & 3). The heterotopic bone did not connect directly to the patella or the tibial tubercle; therefore, the patient was able to maintain complete flexion of the knee. The preoperative Insall-Salvati ratio was 1.6. For intraoperative reference, the length of the inferior pole to the tibial tubercle, on the uninjured contralateral knee, was 6 cm and notated on the operative knee with an indelible marker.

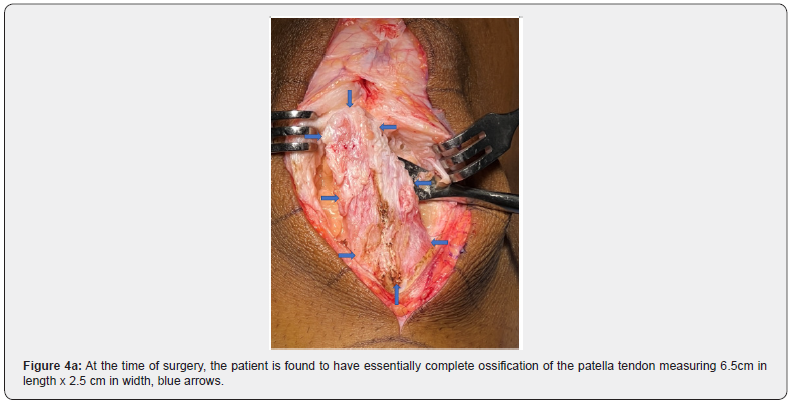
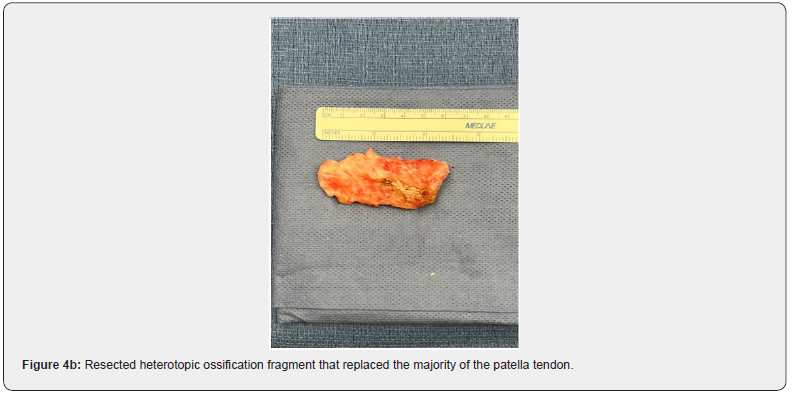
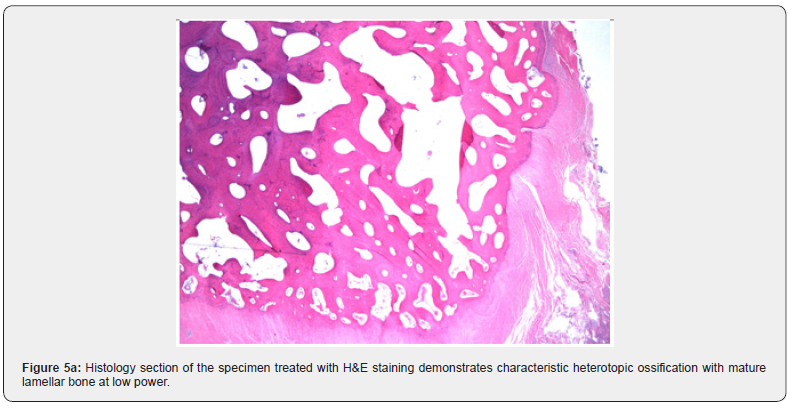
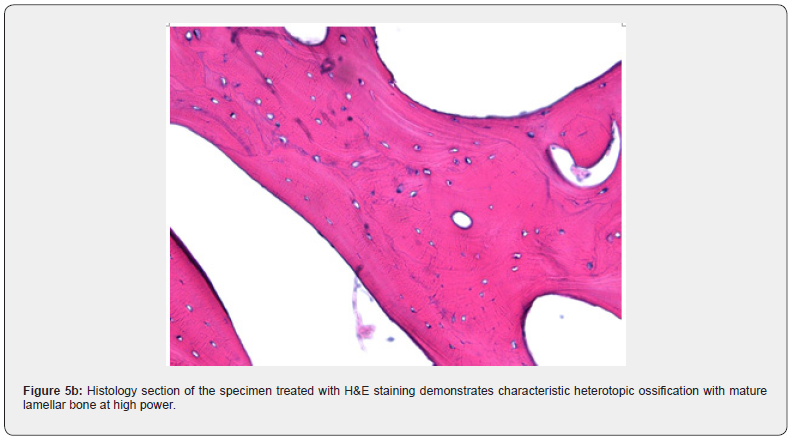
The patient elected to move forward with heterotopic bone excision and allograft reconstruction of the patella tendon. At the time of surgery, the patient was found to have essentially complete ossification of the patella tendon measuring 6.5cm in length x 2.5 cm in width, blue arrows (Figures 4a & 4b). This fragment of bone was excised while attempting to carefully preserve the superficial fascial tissue of the patella tendon. The heterotopic bone fragment was one solid fragment but did not connect to the patella or the tibia. It was excised with sharp and blunt dissection, no osteotome, rongeur, or saw was required. A very small additional bone fragment was not seen grossly or with fluoroscopic imaging and left behind and seen only on postoperative radiographs. Histology sections of the specimen treated with H&E staining demonstrate characteristic heterotopic ossification with mature lamellar bone at low and high power (Figures 5a & 5b).
Once the heterotopic bone was excised, the patella tendon was reconstructed with a large fresh-frozen non-irradiated, agematched, posterior tibialis allograft. The single limb diameter varied from 8 to 9mm dependent on graft location; the length measured 26 cm. Under fluoroscopic control, a transverse 8mm drill hole was carefully made in the patella closer to the articular surface to completely preserve the cortical bone on the more superficial tension cortex (green arrows), to minimize the risk of patella fracture (Figure 6). Each arm of the allograft was prepared in whip stitch fashion with #2 Fiberwire (Arthrex, Naples, FL).
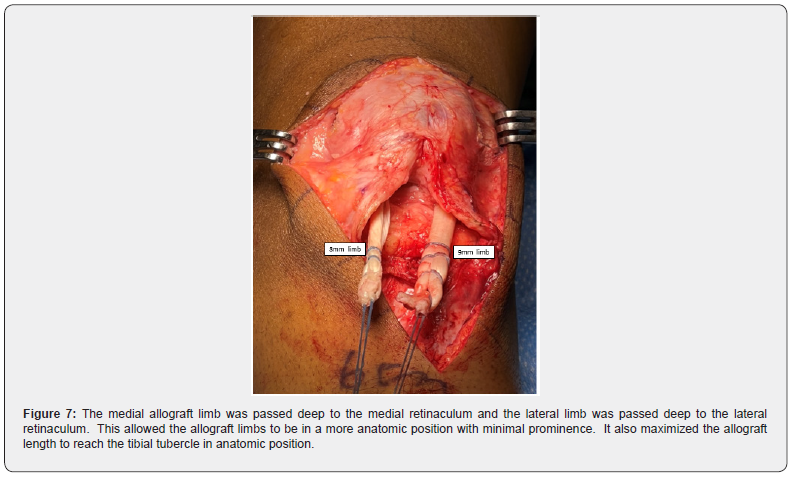
The smaller, 8mm, limb of the allograft was passed through the transverse tunnel in the patella. The medial allograft limb was passed deep to the medial retinaculum and the lateral limb was passed deep to the lateral retinaculum (Figure 7). This allowed the allograft limbs to be in a more anatomic position with minimal prominence. It also maximized the allograft length to reach the tibial tubercle for direct bone fixation in anatomic position. Each free end of the allograft was tensioned, to correct the patella alta, and fixed to the tibial tubercle in two 9mm tunnels, located on the medial and lateral aspects of the tibial tubercle, with a robust anterior cortical bridge left intact between the 2 tunnels. The 9mm tibial tubercle bone tunnels connected to each other, angled 45 degrees deeper in the anterior, proximal tibia. A suture passer was used to retrieve the sutures in the lateral arm of the graft through the medial 9mm tunnel, and then the suture passer was used to retrieve sutures in the medial arm of the graft through the lateral 9mm tibial tubercle tunnel.
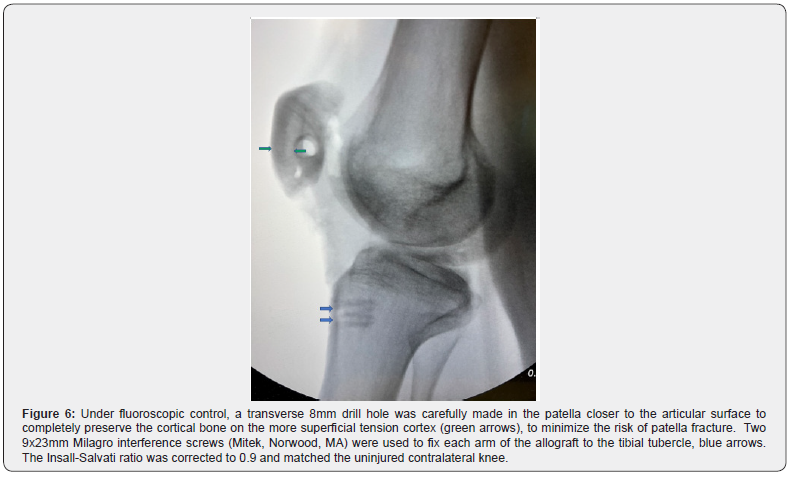
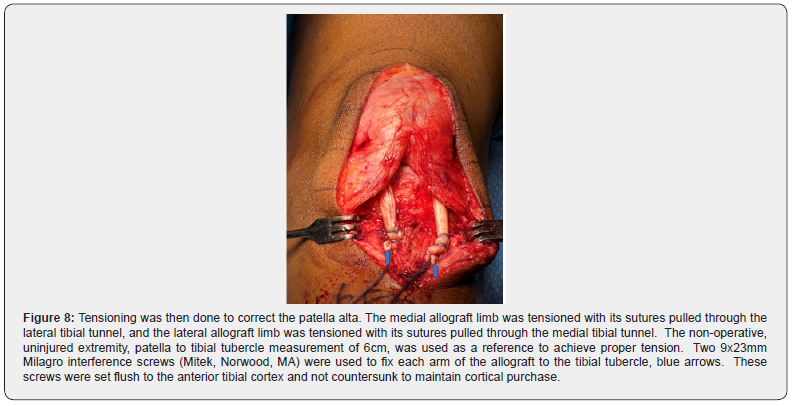
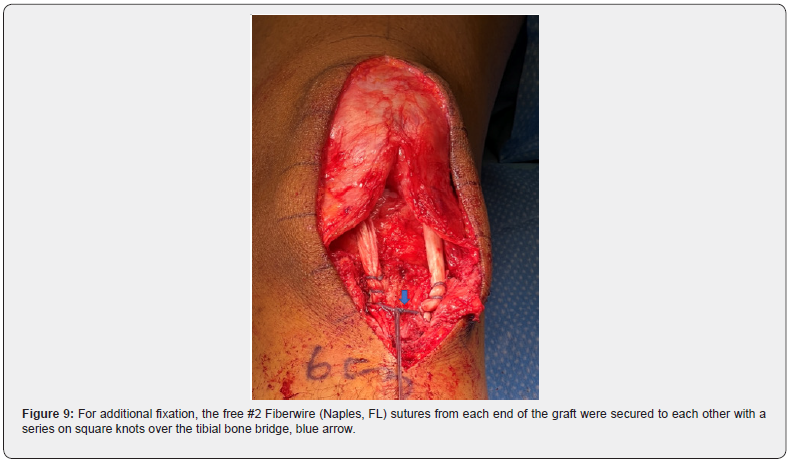
Tensioning was then done to correct the patella alta. The medial allograft limb was tensioned with its sutures pulled through the lateral tibial tunnel, and the lateral allograft limb was tensioned with its sutures pulled through the medial tibial tunnel. The contralateral uninjured extremity, patella to tibial tubercle measurement of 6cm, was used as a reference to achieve proper tension. Two 9x23mm Milagro interference screws (Mitek, Norwood, MA) were used to fix each arm of the allograft to the tibial tubercle, blue arrows (Figures 6 & 8). These screws were set flush to the anterior tibial cortex and not countersunk to maintain cortical purchase. Approximately 2cm of allograft was placed into each tibial tunnel. For additional fixation, the free #2 Fiberwire (Naples, FL) sutures from each end of the graft limbs were secured to each other with a series on square knots over the tibial bone bridge, blue arrow (Figure 9). To help provide another level of stability, and an internal splint, these same four suture limbs (green arrows) were then secured above the patella in a cerclage fashion, (blue arrow) (Figure 10).
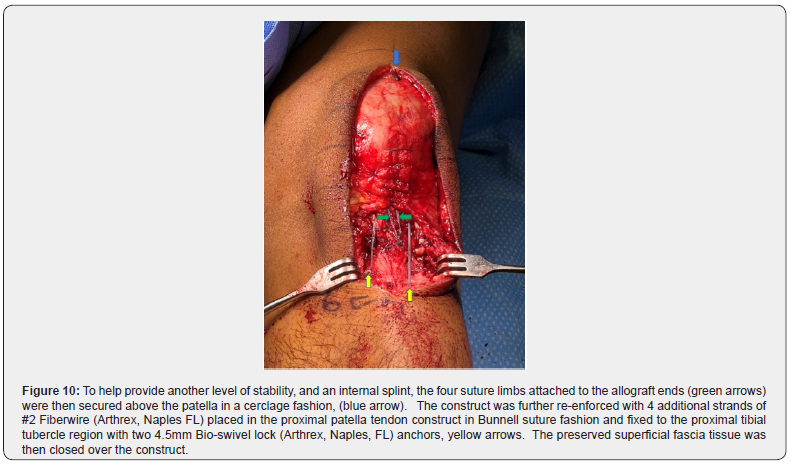
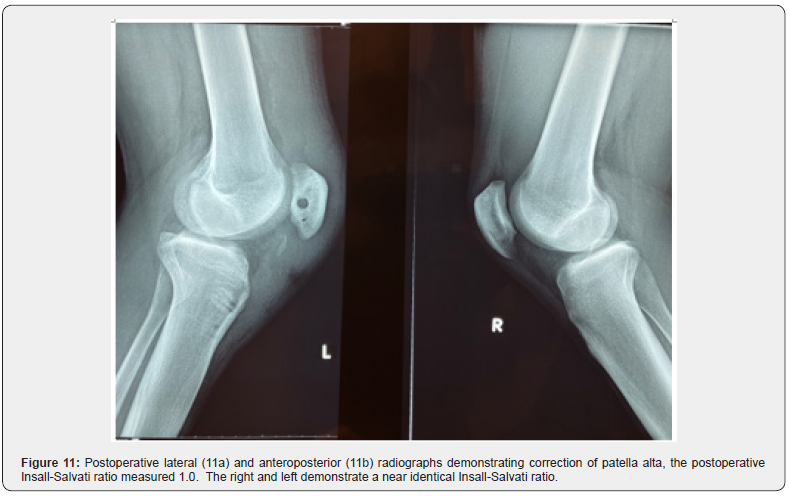
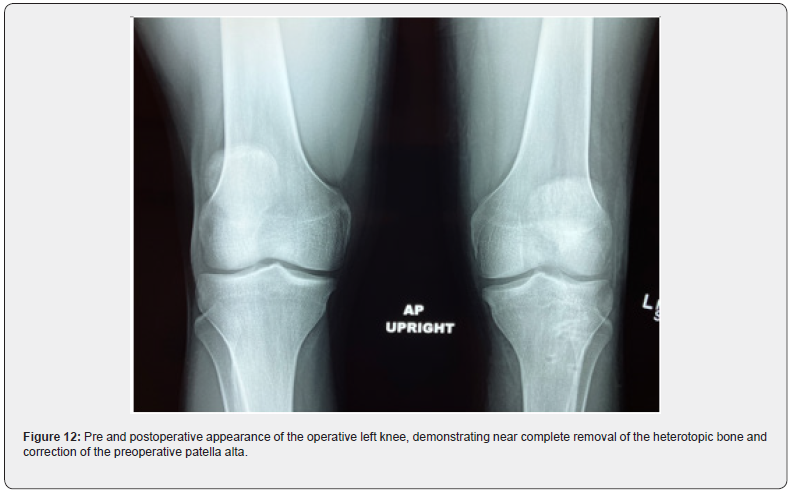
The construct was further re-enforced with 4 additional strands of #2 Fiberwire (Arthrex, Naples FL) placed in the proximal patella tendon construct in Bunnell suture fashion and fixed to the proximal tibial tubercle region with two, drilled and tapped, 4.5mm Bio-swivel lock (Arthrex, Naples, FL) anchors, yellow arrows (Figure 10). The preserved superficial fascia tissue was then closed over the construct (Figure 10). Intraoperatively, the knee flexed beyond 90 degrees without compromise to the construct. After correction of patella alta, the postoperative Insall-Salvati ratio measured 1.0 (Figure 11a & 11b). The right and left demonstrate a near identical Insall-Salvati ratio (Figure 11a & 11b). Figure 12 demonstrates the pre and postoperative appearance of the operative knee, demonstrating near complete removal of the heterotopic bone and correction of patella height. After one week of immobilization, the range of motion started. Flexion was limited to 90 degrees for the first 6 weeks and then progressed to ROM as tolerated.
Discussion
Yousef et al. [5] reported 5 male pediatric patient traumatic ruptures of the patella tendon in a series of 71 patients that sustained trauma to the extensor mechanism. The average age at the time of patella tendon injury was 13.6 years (12-15 years). Three of the patients had a pure soft tissue avulsion distally from the tibial tubercle, 1 patient had a pure soft tissue avulsion from the inferior pole of the patella, and 1 patient had a midsubstance rupture. Our case report, along with the three cases of heterotopic ossification after patella tendon rupture, fit a similar demographic to Yousef et al. [5]; adolescent males with probable incomplete closure of the epiphysis/apohysis around the knee. Our case along with 4 of 5 of Yousef et al. [5] series were nearing skeletal maturity, and all had pure patella tendon avulsion injuries without bone. However, Yousef et al. [5] patients all underwent immediate surgical repair, and none had evidence of heterotopic ossification. Calcification of the patella tendon after sleeve fractures of the inferior pole of the patella or the tibial tubercle have been reported after conservative treatment in 2 cases from Brujin et al. [6] and 1 case by Damrow et al. [7].
The heterotopic ossification in our cases and the three reported in the literature could be the result of residual tibial tubercle or inferior patella microscopic chondrocytes from the apophysis in the avulsed end of the tendon, resulting in heterotopic bone formation, similar to a sleeve fracture. In our present case, the avulsed distal patella tendon was retracted proximally upon itself (Figure 1); the distal end of the patella tendon with microscopic chondrocytes from the tibial tubercle apophysis could have possibly seeded the ossification process of the retracted and redundant tendon curled up on itself (Figure 1). There was no evidence of a sleeve fracture on MRI (Figure 1). In the two cases reported by Matsumoto et al. [1], both had cast immobilization as the form of initial treatment. There was no mention of sleeve fractures. Theoretically, both of these cases could have had retracted patella tendon avulsion tissue with chondrocytes from the apophysis of the inferior pole of the patella or the tibial tubercle, potentially seeding the area for heterotopic ossification. Or they could have been sleeving fractures similar to the cases reported by Brujin et al. [6] and Darrow et al. [7].
Regardless, early surgical fixation of these ruptures is essential to minimize the risk of long-term dysfunction of the extensor mechanism, the need for complicated delayed reconstruction of the patella tendon and to minimize the risk of heterotopic ossification. Recognizing patella alta is a critical finding in identifying these injuries. If there appears to be an increase in patella height, the contralateral uninjured knee can be used as a normal reference for confirmation. This contralateral knee physical examination and radiograph is also useful for preoperative and intraoperative planning to establish the correct patella height of the injured patella tendon.
As early as 1927, allograft material was used to augment the knee extensor mechanism [8]. Many cases of delayed patella tendon reconstruction have been reported [8-11]. This case presented represents a delayed treatment of patella tendon reconstruction along with the significant rare complication of heterotopic ossification of essentially the entire native patella tendon. After the necessary excision of the heterotopic ossification, there was little native patella tendon tissue remaining. This required the use of a large allograft to replace and substitute for the lost native patella tendon tissue. In our previous description of patella tendon reconstruction with semitendinosus autograft, the diameter of the graft was significantly smaller (5-6mm single limb diameter) and were able to place the tunnel in the patella more distal without risk of patella fracture [4]. That smaller size graft would not be sufficient to replace the area lost to heterotopic bone in this case; therefore, we opted for a significantly larger diameter (8-9mm single limb diameter) posterior tibialis allograft in the present case.
To secure such a large allograft, utilizing this technique, a large transverse tunnel was required in the patella. To minimize the risk of fracture, the tunnel was placed closer to the articular margin of the patella to preserve the superficial, tension-side, cortex (Figure 6). The graft was placed slightly distal to the midpoint of the patella from superior to distal (Figure 6). Ideally, the allograft could have been placed more distal in the patella to maximize length of the graft limbs; however, more distal placement would increase the risk of avulsion fracture of the distal patella. Fluroscopy and/or open visualization of the patella is recommended to make certain tunnel patella placement is ideal. To further maintain allograft and length and minimize prominence, the graft medial and lateral allograft limbs were placed deep to their respective retinacula. Maintaining the maximal length of the allograft is essential to allow for adequate tibial graft-bone fixation. Multiple layers of suture and anchor cerclage fixation provided an internal brace to allow immediate mobilization to minimize the risk of stiffness and recurrent heterotopic ossification.
Longitudinal patella drill holes, with suspensory fixation on the superior patella cortex, could also be used to fix the grafts if the morphology of the patella will accommodate without fracture [12]. Achilles tendon, on-lay, allograft could be used as well [13,14]. With calcaneal bone fixation at the tibial tubercle with screws, distal; and Achilles soft tissue fixation, on-lay, superficial to the patella with longitudinal trans-osseous suture or anchor fixation at the inferior pole of the patella, and soft tissue suture fixation or Pulvertaft weave of the Achilles allograft to the quadriceps tendon, proximal. This Achilles graft choice could result in abnormal prominence of the patella.
Achieving the proper length of the reconstructed patella tendon in this setting is another critical factor [4]. The contralateral uninjured knee should be used as a reference to not only help with diagnosis in these injuries but also for surgical planning. The measurement, on the uninjured contralateral extremity, of the patella tendon length from to inferior pole of the patella to the tibial tubercle should done on physical examination and with radiographs or fluoroscopic images to use as a reference to restore the proper position of the injured patella relative to the tibial tubercle, correcting the patella alta.
References
- Matsumoto H, Kawakubo M, Otani T, Fujikawa K (1999) Extensive post-traumatic ossification of the patellar tendon. A report of two cases. J Bone Joint Surg Br 81(1): 34-36.
- Balboni T A, Gobezie R, Mamon H J (2006) Heterotopic ossification: pathophysiology, clinical features, and the role of radiotherapy for prophylaxis. Int J Radiat Oncol Biol Phys 65(5): 1289–1299.
- Supreeth S, Al-Barwani A, Al Habsi I, Al Ghanami S, Al Abri Z, et al. (2020) A Rare Case of Heterotopic Ossification of the Patella Tendon in an Adolescent Presenting with Tendon Rupture. Joints 7(3): 131-134.
- Larson RV, Simonian PT (1995) Semitendinosus augmentation of acute patellar tendon repair with immediate mobilization. Am J Sports Med 23(1): 82-86.
- Yousef MAA, Rosenfeld S (2017) Acute traumatic rupture of the patellar tendon in pediatric population: Case series and review of the literature. Injury 48(11): 2515-2521.
- Bruijn JD, Sanders RJ, Jansen BR (1993) Ossification in the patellar tendon and patella alta following sports injuries in children. Complications of sleeve fractures after conservative treatment. Arch Orthop Trauma Surg 112(3): 157-158.
- Damrow DS, Van Valin SE (2017) Patellar Sleeve Fracture With Ossification of the Patellar Tendon. Orthopedics 40(2): e357-e359.
- Gallie WE, LeMesurier AB (1927) The late repair of fractures of the patella and of rupture of the ligamentum patellae and quadriceps tendon. J Bone Joint Surg 9(1): 47-54.
- Ecker ML, Lotke PA, Glazer RM (1979) Late reconstruction of the patellar tendon. J Bone Joint Surg 61(6A): 884-886.
- Kelikian H, Riashi E, Gleason J (1957) Restoration of quadriceps function in neglected tear of the patellar tendon. Surg Gynecol Obstet 104(2): 200-204.
- Mandelbaum BR, Bartolozzi A, Carney B (1988) A systematic approach to reconstruction of neglected tears of the patellar tendon. Clin Orthop 235: 268-271.
- Choi HS, Jang BW, Chun DI, Kim YB, Seo GW, et al. (2021) Staged patellar tendon reconstruction using doubled bone-patellar tendon-bone allograft for infected patellar tendon rupture: a rare case report of three years follow-up. J Exp Orthop 8(1): 13.
- Falconiero RP, Pallis MP (1996) Chronic rupture of a patellar tendon: a technique for reconstruction with Achilles allograft. Arthroscopy 12(5): 623-626.
- Ginesin EZ, Wojnowski NM, Patel RM (2020) Patellar Tendon Reconstruction for a Chronic Extensor Mechanism Deficit Using an Achilles Tendon Allograft With Hamstring Autograft and Suture Augmentation. Arthrosc Tech 9(4): e469-e475.






























