Early Results from the Evaluation of Spinopelvic Angles in Patients with Hip Pain by Femoroacetabular Impingement
Fernando Martins de Pina Cabral1*, Rodrigo Diego Vieira Pantoja2, Renato Locks1,4, Felipe Figueiredo3, Marcos Emilio Kuschnaroff Contreras4 and Daniel Fernandes5
1 Orthopaedic surgeon at Regional Hospital of São José - Dr. Homero de Miranda Gomes (SC), Brazil
2 Hip fellow at Regional Hospital of São José - Dr. Homero de Miranda Gomes (SC), Brazil)
3 Biostatistics at Oswaldo Cruz Foundation (FIOCRUZ) (RJ), Brazil)
4 Orthopedic surgeon at SOS Cardio Hospital - Florianopolis (SC), Brazil
5 Orthopedic surgeon at Federal University of Santa Catarina Hospital (SC), Brazil
Submission:April 22, 2023; Published: May 02, 2023
*Corresponding author: Fernando Martins de Pina Cabral, Orthopaedic surgeon at Regional Hospital of Sao Jose - Dr. Homero de Miranda Gomes (SC), Brazil
How to cite this article: Cabral FMP, Pantoja RDV, Locks R, Figueiredo F, Contreras MEK, Fernandes D, et al. Early Results from the Evaluation of Spinopelvic Angles in Patients with Hip Pain by Femoroacetabular Impingement. Ortho & Rheum Open Access J. 2023; 21(4): 556069. DOI: 10.19080/OROAJ.2023.21.556069
Abstract
Purpose: to evaluate spinopelvic angles in patients with hip pain and femoroacetabular impingement (FAI). After the discovery of the FAI in 2003, a complete biomechanical analysis of the lower limb and its relationship with the spine became indispensable, in the context of preservative surgery and/or at hip arthroplasty.
Methods: twenty patients aged between 18 and 60 years with hip pain were evaluated. All had pain for more than 3 months and FAI syndrome. All signed the informed consent form, had their anthropometric data and Harris Hip Score (HHS) evaluated.
Results: the average age was 40 years and female gender in 76%. The mean Body Mass Index (BMI) was 21 kg/m2 and the mean HHS was 70 points. The time between hip pain onset and clinical evaluation was two and a half years. Alterations of the spinopelvic angles were found in 58% of the patients. We found statistically significant differences at the sacral slope (SS) (p: 0.006) and anterior pelvic plane (APP) angles (p: 0.013), between patients with and without hip arthrosis, and a decrease in both angles between standing and sitting positions. This translates into a more up verticalization pelvis position and posterior tilt, the greater the arthrosis.
Conclusion: the presence of lower back pain associated with angular spinopelvic alterations in 58% of patients with FAI and the difference between patients according to the degree of hip arthrosis reveal the importance of evaluating this parameters and showing this early results.
Keywords: Femoroacetabular impingement; Spinopelvic angles; Hip arthrosis; Lumbar spine arthrosis; Hip preservation surgery; Hip arthroplasty
Introduction
The evaluation of the spinopelvic angles have been subject of increased interest in the biomechanical assessment of the hip [1]. It is known that there is an association between degenerative diseases of the hip and lumbar spine, first described by Macnab as Hip-Spine Syndrome in 1983, when it was reported that 27% of the patients over 45 years of age had symptoms in both places [2]. The incidence of hip and spinal arthrosis has increased in the population, and it may be difficult to differentiate the origin of the pain when concomitant, due to the complaints being generally subjective and possibly overlapping [2-4].
The change to bipedalism led to increased verticalization of the pelvis and this resulted in a change in the structure of the muscles that support the spine [5]. The orthostatic position is a unique, stable and ergonomic posture, which has led the pelvis to be a key structure in the human motor apparatus, also called the pelvic vertebrae [6]. The sacral plateau forms the base to support the spine and is the point of load transfer from the trunk to the pelvis. The normal pelvis is horizontal in the frontal plane, but this geometry is more complex in the sagittal plane, whose parameters needs to be defined for a better biomechanical interpretation [7]. In a progressively unbalanced spine, there is a tilting of the upper body anteriorly, and consequently the posterior muscles from the trunk exert more force to counterbalance the gravitational moment of force. The lack of sagittal balance progressively leads to lumbar hyperextension, posterior pelvic tilt, knee flexion and ankle extension [8,9].
FAI is a dynamic conflict between the femoral head and the acetabulum, that can be of three types: CAM type, when there is an absence of sphericity in the femoral head-neck transition; Pincer type, which occurs when the acetabulum provides excessive coverage of the femoral head; and Mixed type, which is a combination of both types of impingement [9-12]. FAI occurs mainly in younger patients, especially at those who play high-impact sports, perform torsional or lateral movements, or constant squatting [10,11]. The aim of the study was to evaluate patients with hip pain by FAI and to investigate possible variations of the spinopelvic angles as sacral slope and anterior pelvic plane between standing and sitting positions.
Materials and Methods
Thirty-eight patients aged over 18 years who spontaneously presented to the doctor’s authors and co-author’s outpatient offices for hip pain assessment were evaluated, in the period from June 2020 to June 2021, after approval of the study by the research ethics committee, respecting the statement of the Human and Animal Rights. Subsequently, 18 patients could not complete all the images protocol due to covid-19 restrictions and were excluded. Three patients were excluded too, one for having angular alteration of the femur (varus), another due to torsional alteration of the femur (antetorsion) and other one due to a concomitant lesion of the gluteus medius musculature (tendinosis). Four patients had bilateral pain, totaling 17 patients evaluated and 21 hips with radiographic alterations of FAI.
The patients presented hip pain for more than three months and were submitted to a complete anamnesis, physical examination and complementary radiographic series, according to the protocol described by Tannast et al. [13,14]. On physical examination, hip pain was presented with intra-articular features on specific tests. The patients had their anthropometric data measured and HHS performed [15]. All other possible causes of hip-related diseases were excluded.
The determining angles for the radiographic diagnosis of FAI, were measured on the AP X-ray, were the alpha angle, acetabular center-edge angle, acetabular index, cervical-diaphyseal angle and the measurement of joint space. The radiographic incidence of Lequesne was also used to evaluate posteroinferior acetabular arthrosis and the hip profile view was used to measure the alpha angle. Computed tomography (CT) was requested to evaluate the acetabular version and the torsional alterations of the femur [16]. The spinopelvic angles of the patients were evaluated in the radiographic profile view of the lumbar spine, in the standing and sitting positions, where we measured the SS and the APP angles. The SS is the angle of inclination of the sacral plateau relative to the ground and determines the position of the lumbar spine, since it forms the base of the spine. It has an average inclination of 41.2° ± 7° [8]. The PPA is the angle between the line connecting the pubic symphysis to the anterior superior iliac spines, measured in comparison to the line perpendicular to the ground, with an average variation of 0° to 12° [17] (Figures 1 & 2).
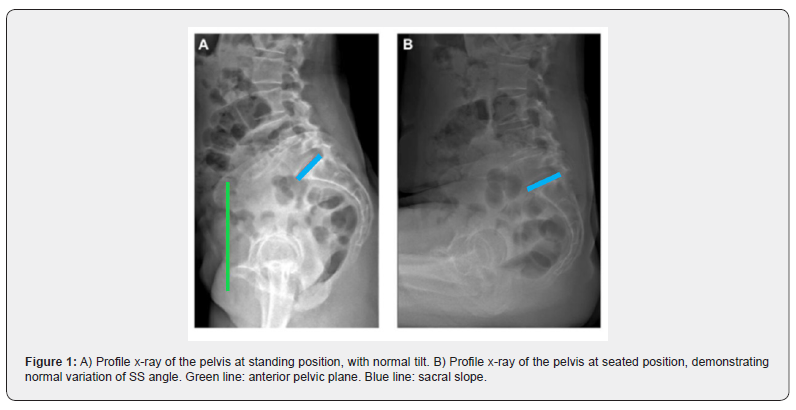
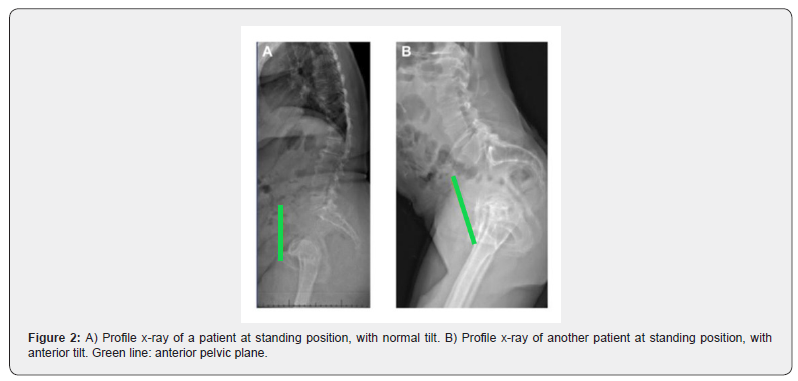
The evaluation of the lumbar spine mobility was done by the difference between the angle of the SS in standing and sitting positions. The normal values ranges from 10° to 30°. Values below 10° are considered a stiff lumbar spine and values above 30° are classified as hypermobile [8]. The position of the pelvis was assessed by the APP angle in the standing position. Negative values were considered as posterior tilt and values greater than 12° were considered as anterior pelvic tilt (Figures 1 & 2).
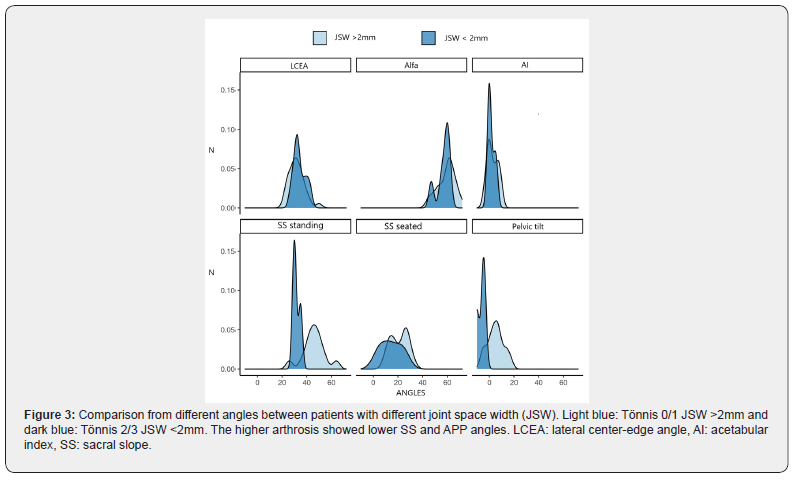
Patients were classified based on the degree of hip arthrosis according to the classification recommended by Tonnis [18], where grades 0 and 1 meant hips with joint space greater than 50% or 2 millimeters, were considered normal or mild alterations respectively and categorized with less arthrosis. Grades 2 and 3 meant hips with a compromised joint space more than 50%, with moderate and severe arthrosis respectively, categorized with more arthrosis and used as a comparative group. All angles were checked manually at two different times by the author, with a goniometer measured in degrees and millimeters (Figure 3).
Demographic characteristics such as gender, age, BMI and clinical characteristics such as side and time of pain, occurrence of lower back pain, HHS, type of FAI, spinopelvic mobility and Tonnis classification, were described as mean standard deviation (SD) or frequency and proportion in percentage (%), as appropriate. Continuous variables were compared between groups with a linear model adjusted for sex, age and BMI of participants (ANCOVA), allowing adjustment for covariates to correct for confounding. All analyses were performed at 5% significance level. All hypothesis tests were calculated at two-tailed confidence intervals. The software used was R, version 4.1.1.
Results
The average age was 40 years, and the female gender was more prevalent in this study (76%). The mean BMI was 21 kg/m2. Patients had hip pain on average for 2 and ½ years before the evaluation, mainly on the right side (41%). Bilateralism was present in 24% of cases (Table 1). The mean HHS was 70 ± 11 points, but in patients with more arthrosis, the mean score was 61 points (Tonnis > 1), found in 17% of the patients in the study.
Regarding FAI, CAM type was the most present among the patients, in 73% of the cases, with an average alpha angle of 58° ± 3°. Mixed type was observed in 21% of cases and the Pincer type in 6% of cases. Of the patients with less arthrosis (Tonnis 0 or 1), 53% had type 0 and 29% had type 1. In the groups with more arthrosis (Tonnis 2 or 3), 6% had moderate, type 2 and 12% had type 3, severe (Table 1). The SS angle showed a statistically significant difference between the group with less arthrosis, compared with the group with more arthrosis (p: 0.0006), being found on average 46° and 32° respectively. The pelvic tilt also showed a statistically significant difference between those groups, with a mean of 5° and -6° respectively (p: 0.013) (Table 2).
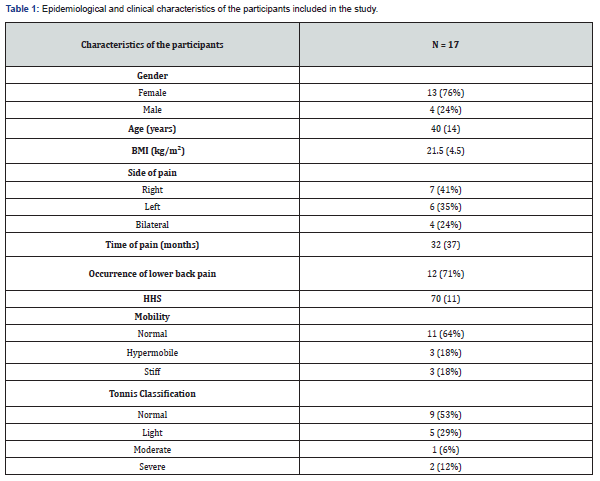
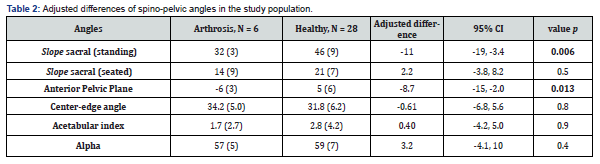
Most patients had no alteration in spinopelvic mobility (64%), but 18% had hypermobility and 18% had stiffness between the sitting and standing positions. Of the patients, 71% reported lower back pain for more than 3 months. The average standing SS in the study was 43.2° (SD 9.67°), ranging from 26° to 64°. The average seated SS was 19.8° (SD 7.41°) and ranged between 5 and 32°. The mean APP angle was 3.12° (SD 7.12°), ranging from -10° to 17°. The average center-edge angle was 32.2° (SD 6.04°), the average alpha angle was 58.8° (SD 6.70°) and the average acetabular index was 2.56° (SD 3.99°) (Table 2). The standing SS and the APP were significantly different in the group with less arthrosis when compared to the group without more arthrosis (Table 2). After adjusting for gender, age, BMI and HHS the difference in the standing SS was 11° (ANCOVA, CI: -19 -3.4; p= 0.006) and the APP was 8.7° (ANCOVA, CI: -15 – -2.0; p= 0.013). The seated SS angle had no statistically relevant difference: 2.2° (ANCOVA, CI: -3.8 – 8.2, p= 0.5). Other angles had similar distributions between the two groups. The mean center-edge angle in the more arthrosis group was 34.2° and 31.8° in the less arthrosis group (CI: -6.8 - 5.6°). The mean acetabular index was 2.8° and 1.7° respectively (CI: -4.2 - 5.0°). The mean alpha angle was 59 and 57° respectively (CI: -4.1° - 10°) (Table 2).
Discussion
Following the publication of the Ganz et al. [11] in 2003 and the discovery of FAI, there has been an increased interest in procedures that try to prevent or at least slow down the evolution of hip arthrosis [12]. It is known that the ageing of the population and the consequent increase in the number of cases of hip fracture have led to an increase in the number of surgeries for joint replacement [19]. Recent projections in the United States predict an increase in this surgery of 129% and 284% in the years 2030 and 2040 respectively [20]. Therefore, a complete biomechanical analysis of the relationships between the spine, pelvis and lower limbs is very important for a better understanding and treating the hip problems [1,2,21].
In our study, lower back pain was reported in 71% of patients. Of these, 58% of the patients presented spinopelvic alterations, this being the main reason for presenting this study in a preliminary form. We evaluated patients with FAI alterations with emphasis on preservative surgeries, but despite this, we have found patients with grades 2 and 3 arthrosis, whose indications for preservative surgeries have worse results, so they were used as a comparative group [10]. Spinopelvic evaluation, in the context of hip surgery, has been more emphasized in recent years, as adverse results have been demonstrated with the non-observation of the degree of lumbar mobility and pelvic positioning, both in patients with FAI syndrome and hip arthroplasties [22-24].
In the assessment of the mobility of the lumbar spine, hypermobility may be investigated in cases of FAI as a supportive factor in the impingement analysis, and in planning arthroplasty, seeking to position the components as close as possible to the range-of-motion considered ideal. This is an attempt to avoid dislocation, when the components are out of the ideally recommended version and/or inclination [21,22].
On the other hand, in cases in which the pelvic mobility is reduced, it is necessary to observe in which position the pelvis is, in the orthostatic position, for the appropriate correction [22,23]. It has been shown that with aging, there is increased stiffness and the most found pelvic position is the posterior tilt [22,23]. In our study, this association was also found with an increase in the degree of arthrosis, but this was not our final desired outcome, so we should not extrapolate this finding to the treatment of FAI. However, in the evaluation related to arthroplasty, we should in these cases with less inclination and anteversion at the acetabular component, to avoid a lack of anterior and superior coverage in the standing position. Conversely, patients with fixed anterior pelvic tilt may predispose to posterior dislocation of the hip in the sitting position, due to lack of posterior coverage and/or anterior impact of the neck against the acetabular edge [25].
Aaron et al calculated that for each degree of posterior deviation of the APP angle, there was an increase in acetabular anteversion of between 0.7° to 0.8°, and 0.29° in acetabular tilt [26]. This mathematically proves the direct influence of the spino-pelvic angle on acetabular version and inclination. Hypotheses for dislocations after arthroplasties have been previously reported, such as the study by Abdel et al., who identified in a cohort of almost 10,000 cases, where 58% of the dislocations were within the recommended acetabular inclination and anteversion range [23]. Therefore, it is recommend an acetabular component with greater anteversion [27,28], or the use of double mobility components, whose articulation has already demonstrated lower rates of dislocation when compared to conventional prostheses, by increasing the impact-free movement arc between the cone and the acetabular edge [29]. In our study, we found posterior tilt in 29% of the patients in the lateral view of the pelvis in the standing position, which translates as a greater up verticalization of the pelvis, mainly found in patients with arthrosis (p: 0.013) which may influence impingement.
Pelvic mobility was altered in 1/3 of the patients, half of them had hypermobility and the other half had stiffness. It has been observed that symptomatic patients with FAI may require more hip flexion to achieve a sitting position, due to limited spinal flexion when anterior pelvic tilt occurs. The compensatory mechanisms involved in the change from standing to sitting position, such as flexion and external rotation of the hip, are related to pain reduction, thus trying to avoid the impingement [24]. Finally, the relationship of the FAI and the static evaluation of lumbar and pelvic biomechanics need further studies, possible diagnostic innovations and a larger target population, trying to better understand this interaction. Perhaps it can also be better understood if the study includes an associated dynamic assessment. There is still no standardization in this evaluation either in static or kinematic examination [30].
We observed alteration of the spino-pelvic angles in 58% of the patients with IFA, where 71% of them reported associated lumbar pain. Sacral slope and pelvic tilt varied according to the degree of hip arthrosis. The greater the degree of arthrosis, the lower were the values of the sacral slope and anatomic pelvic plane angles. This translates into a greater up verticalization of the pelvis and posterior pelvic tilt, which may affect the hip biomechanics, especially in more advanced cases of joint injury. Despite the small number of patients in this study, the association observed between spino-pelvic angles and FAI has aroused greater interest in this evaluation and was the main reason for this preliminary publication. We believe that further studies should be carried out for a better understanding of all the factors involved, including associating dynamic biomechanical analyses.
Conflict of interest
The authors declare that they have no conflicts of interest that could influence the results obtained.
References
- Pierannunzil L (2017) Pelvic posture and kinematics in femoroacetabular impingement: a systematic review. J Orthop Traumatol 18(3): 187-196.
- Offierski CM, MacNab I (1983) Hip-spine syndrome. Spine 8(3): 316–321.
- Swezey RL (2013) Overdiagnosed sciatica and stenosis, underdiagnosed hip arthritis. Orthopedics 26(2): 173-174.
- Prather H, Cheng A, Steger-May K, Maheshwari V, VanDillen L (2018) Association of hip radiograph findings with pain and function in patients presenting with low back pain. PM & R 10(1): 11-18.
- Berge C (1998) Heterochronic processes in human evolution: an ontogenetic analysis of the hominid pelvis. Am J Phys Anthropol 105(4): 441-459.
- Dubousset J, Charpak G, Dorion I, Skalli W, Lavaste F, et al. (2005) A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull Acad Natl Med 189(2): 287-297.
- Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20(4): 451-462.
- Boulay C, Tardieu C, Hecquet J, Benaim C, Mouilleseaux B, et al. (2006) Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J 15(4): 415–422.
- Mac-Thiong JM, Labelle H (2006) A proposal for a surgical classification of pediatric lumbosacral spondylolisthesis based on current literature. Eur Spine J 15(10): 1425-1435.
- Leunig M, Beaule PE, Ganz R (2008) The Concept of Femoroacetabular Impingement: Current Status and Future Perspectives. Clin Orthop Relat Res 467(3): 616–622.
- Ganz R, Parvizi J, Beck M (2003) Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 417: 112-120.
- Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, et al. (2002) The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 84(4): 556–560.
- Tannast M, Siebenrock KA, Anderson SE (2007) Femoroacetabular Impingement: Radiographic Diagnosis-What the Radiologist Should Know. AJR Am J Roentgenol 188(6): 1540-1552.
- Tannast M, Murphy SB, Langlotz F, Anderson SE, Siebenrock KA (2006) Estimation of pelvic tilt on anteroposterior X-rays – A comparison of six parameters. Skeletal Radiology 5: 149-155.
- Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4): 737-755.
- S B Murphy, S R Simon, P K Kijewski, R H Wilkinson, N T Griscom (1987) Femoral anteversion. J Bone Joint Surg Am 69(8): 1169-1176.
- Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7(2): 99-103.
- Tonnis D, Heinecke A (1999) Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 81(12): 1747–1770.
- Ingvarsson T, Agglund G, Lohmander LS (1999) Prevalence of hip osteoarthritis in Iceland. Ann Rheum Dis 58(4): 201–207.
- Singh JA, Yu S, Cleveland J, Cleveland LC (2019) Rates of Total Joint Replacement in the United States: Future Projections to 2020–2040 Using the National Inpatient Sample. J Rheumatol 46(9): 1134-1140.
- Abdel MP, Von Roth P, Jennings MT, Hanssen AD, Pagnano MW (2016) What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin Orthop Relat Res 474(2): 386-391.
- Lewineck GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 60(2): 217–222.
- Lee SH, Lim CW, Choi KY, Jo S (2019) Effect of Spine-Pelvis Relationship in Total Hip Arthroplasty. Hip Pelvis 31(1): 4-10.
- Fader RR, Tao MA, Gaudiani MA, Turk R, Nwachukwu BU, et al. (2018) The role of lumbar lordoses and pelvic sagital balance in femoroacetabular impingement. JBJS 100-B(10): 1275-1279.
- Abdel MP (2019) Simplifying the Hip-Spine Relationship for Total Hip Arthroplasty: Introduction. The J Arthroplasty 34(7S): S51-S52.
- Aaron JB, DelSole EM, George SG, Vira S, Lafage V Errico, et al. (2017) Sagittal Pelvic Orientation. A Comparison of Two Methods of Measurement. Bull Hosp Jt Dis 75(4): 234-240.
- Wan Z, Malik A, Jaramaz B, Chao L, Dorr LD (2009) Imaging and Navigation Measurement of Acetabular Component Position in THA. Clin Orthop Relat Res 467(1): 32-42.
- Yang G, Li Y, Zhang H (2019) The Influence of Pelvic Tilt on the Anteversion Angle of the Acetabular Prosthesis. Orthop Surg 11(5): 762-769.
- Heckmann N, Weitzman DS, Jaffri H, Berry DJ, Springer BD, et al. (2020) Trends in the use of dual mobility bearings in hip arthroplasty. Bone Joint J 102-B: 27-32.
- Papi E, Bull MJA, McGregor AH (2018) Is there evidence to use kinematic/kinetic measures clinically in low back pain patients? A systematic review. Clin Biomech (Bristol, Avon) 55: 53-64.






























