Retrospective Review of 45 Implanted Human Acellular Dermal Lyophilized Implants to Stabilize Talotarsal Instability, Single Center, Single Surgeon Case Series
Vern Christensen1 JJ VanYperen2and Bruce Werber3*
1DPM, Foot Specialists of Mississippi, Armory, USA
2DPM Foot Specialists of Mississippi, Armory, USA
3DPM, MSc, FACFAS Cuboid Associates, Fort Lauderdale FL, USA
Submission:July 26, 2022; Published:August 08, 2022
*Corresponding author: Bruce Werber, DPM, MSc, FACFAS Cuboid Associates, Fort Lauderdale FL, USA Ortho &
How to cite this article: Vern C, JJ VanY, Bruce W. Retrospective Review of 45 Implanted Human Acellular Dermal Lyophilized Implants to Stabilize Talotarsal Instability, Single Center, Single Surgeon Case Series. Ortho & Rheum Open Access J. 2022; 20(2): 556035. DOI: 10.19080/OROAJ.2022.20.556035
Abstract
A retrospective review of 45 surgeries for repair of Talotarsal instability, with a review of the clinical, radiographic, and biomechanical aspects associated with Talotarsal dislocation and instability. The surgeons utilized an acellular lyophilized human dermal tissue engineered into a cylindrical configuration (stent) to be implanted from lateral to medial via the sinus tarsi. The goal of surgery is to reduce the dislocation, to enhance positioning of the rearfoot and allow regeneration of the Talotarsal ligamentous structures into a more stable configuration. Outcomes found in this review are very promising, none of the implant stents required removal, elimination of the sense of hard stop as seen with other materials in this procedure. Conclusion: excellent outcomes with minimal adverse events, rapid restoration of function in all patients.
Keywords: Talotarsal dislocation; Talotarsal instability; Sinus tarsistent; Flatfoot
Background
Musculoskeletal disorders are a leading cause of disability worldwide, with enormous associated economic healthcare costs associated with frequent pain causing limited or in many cases patients inability to move. This level of disability leads to tremendous secondary healthcare consequences including obesity, diabetes, cardiac issues of hypertension, heart failure, and osteoarthritis. In the USA these disorders account for over 40% of disabling conditions in persons 18 years or older and more than 50% of all chronic conditions in people 50 years of age in developed countries. The direct healthcare costs and indirect costs are estimated to be in the range of 849billion equivalent to 8% gross domestic product in 2015 [1-3].
Where does this all begin? In many but not all cases the origin can be traced back to foot/ankle failure (specifically pediatric and adult flatfoot) that has gone unrecognized as a disorder. It has been reported in multiple venues of Pediatricians’ advice to parents of the patient paraphrased as “don’t worry they will outgrow it”. In reality, the pediatrician does not follow the patient into their thirties or forties to see that the abnormal function has progressed markedly and was not outgrown but rather accommodated with abnormal foot function, limb length discrepancy, scoliosis, or other skeletal compensations [4,5].
Proximal symptoms of foot/ankle failure can include osteochondral lesions of the talar dome, growing pains, shin splints, patellofemoral pain, ACL strain, knee OA, sciatica, hip OA, functional leg length discrepancy, pelvic tilt, and spine malalignment [6]. Though, we cannot just focus on the pediatric painful flatfoot, the adult acquired flatfoot deformity cannot be ignored as it is the source of more significant pathology and disability. The adult flatfoot is characterized by flattening of the medial longitudinal arch with insufficiency of the posteromedial structures of the ankle and hindfoot. Closely associated with Posterior tibial tendon dysfunction (PTTD) as well as other common foot and ankle pathologies e.g., tarsal tunnel syndrome, plantar Fasciopathies, and Achilles enthesopathy to name a few [7-9].
Malalignment of the Talo Tarsal Joints (TTJ) leads to a faulty foot foundation that will lead to misalignment of proximal structures, e.g., the ankle, knee, hip, pelvis, and spine. The foot which creates, a foundation for the human skeleton must have proper alignment to be balanced for the entire skeletal kinetic chain to function as designed. In reviewing the literature painful flexible flatfoot occurs approximately 5% in the pediatric and adult population. Symptomatic patients present with a variety of complaints, such as generalized fatigue with minimal activity walking or standing in the foot, ankle or lower leg, nonspecific lower back, hip or knee pains, preferring to sit vs being active. As noted above, this can lead to a variety of additional health issues, number one being obesity which often leads to increased musculoskeletal and metabolic syndrome issues.
The imbalance in flexible flatfoot, a congenital or acquired talotarsal (talus/ calcaneus/ cuboid/ navicular) joint dislocation, with components of ligamentous laxity or injury to the structures, can be associated with this complex as well as imbalance/tightness of lower leg musculature.
The above combinations of instability, lead to imbalance and malalignment of joints within the entire kinetic chain. Musculoskeletal disorders can cause pain anywhere along the kinetic chain from head (migraines, TMJ type issues) back, hip, knee, ankle, and/or foot. Explained from a different perspective; the talotarsal dislocation causes a redistribution of weight bearing forces throughout the foot, the talus shifts forward and down on the articulating surface of the calcaneus, increasing tibial internal rotation and knee flexion. This leads to excessive pronatory motion within the talotarsal joint, and prolonged internal rotation of the leg. The upper kinetic chain is affected the increased energy (force) through additional medial knee stress and a lateral shift of patella. This energy (force) when experienced in a well-balanced extremity is dissipated equally throughout the foot and leg but when it becomes excessive has a detrimental effect along the full kinetic chain – head to toe [10-22]. The articular surfaces of talus abnormally displace medially, anteriorly, and plantarly during the early stance phase of the gait cycle. The axis point of the TTJ shifts to an excessive pronatory direction. As the limb/foot becomes non-weightbearing, i.e., during the noncontact, swing phase of the gait cycle, there will be a realignment of the articular surfaces.
The flatfoot is the result of a combination of deformities, resulting in peri-talar instability. Multiple studies have demonstrated that medial displacement calcaneal osteotomy has little to no impact on talar realignment. Campbell et al. [23] show that deformity of calcaneus being in the valgus position, results in the talus having a medial plantar tilt that leads to a reduction in or absence of the longitudinal arch [24].
Flatfoot can be categorized as being either flexible or rigid and the method of treatment depends on this designation. When non-weight-bearing, a flexible flatfoot has a normal architecture but excessive midtarsal and talotarsal joint pronation with a clear collapse of the medial arch during both static and dynamic weight-bearing [25,26].
While the majority of cases of flexible flatfoot in children remain asymptomatic, those cases that are symptomatic need to be treated with either conservative or surgical approaches [27,28]. Kirby [29] describes the subtalar joint as a mechanical link between the foot and the lower extremity (aka torque converter), Transverse plane rotations of the leg are converted into frontal plane rotations of the foot (and vice versa) by the oblique triplane orientation of the subtalar joint axis. Two functions of the STJ are to allow the foot to pronate and, to act as a mobile adapter when bearing weight to allow the foot to supinate into a position of increased sagittal plane stability during the propulsive phase of gait.
During the closed kinetic chain STJ pronation causes plantarflexion and internal rotation of the talus while supination causes dorsiflexion and external rotation of the talus in relation to the calcaneus/ground. When the STJ is in a normal position, a ground reaction force acting on the medial calcaneal tubercle causes a supination moment across the subtalar joint (STJ) axis. This is because the medial calcaneal tubercle is medial to the STJ axis. We can conclude that during many weightbearing motions the foot can be effectively modeled as a rigid body with the calcaneus, cuboid and navicular all rotating as a single unit around the talus at the STJ axis, to alter this abnormal response.
Placing a rigid cylinder into the sinus tarsi can change the pivot point of the axis to improve position and functionality of the rearfoot. One can consider the idea of moving the pivot point on a seesaw changes the balance of the board. This same concept exists in the STJ. Moving the pivot point influences the muscle tendon pull at their insertion. For example, the peroneus longus has greater stress on its insertion in the inferior aspect of the first ray when the rearfoot is supinated, thereby stabilizing the first ray, yet when the foot is pronated the PL is unable to fully stabilize the first ray.
The balance of forces within the TTJ are integral to efficient hindfoot functioning as they convert vertical force into horizontal force. The posterior Talocalcaneal joint accepts approximately 80% of the vertical force at heel strike and 50% at midstance acting on the posterior facet of the subtalar joint. The remaining force transitions occur within the anterior and middle facets of the subtalar joint [30,31]. The TTJ allows for the unlocking and locking of joints within the medial column of the foot while weight bearing. Pronation of the talotarsal joint complex unlocks the joints allowing for adaptability on uneven surfaces. Then the talotarsal joint resupinates about 1/3 of the way through gait cycle, which stabilizes (stiffens) the foot for heel lift and forward propulsion. In the flexible flatfoot there is a loss of stability and alignment of the talotarsal complex, causing malalignment of the talus and calcaneus. The navicular is forced both plantarly and medially due to the subtalar joint instability
The weightbearing forces are distributed incorrectly which leads to skeletal malalignment, increased strain of ligamentous structures, and increased muscle tendon contraction. This flow of excessive tissue loading and unloading creates excessive strain on the full skeletal structure. This is visualized by noting the lowering of the medial arch of the foot, thus demonstrating the midtarsal joints are unlocked and not prepared to accept the body weight
There is no consensus on the optimal method of treatment; however, there is a consensus on a stable hindfoot being critical to foot, ankle, and proximal musculoskeletal chain biomechanics [32,33]. The goal in treating flexible flatfoot syndrome is to reduce but not eliminate excessive hindfoot motion. Vogler describes the mode of action of a subtalar arthroereisis into three distinct modes “axis altering, impact blocking and self-locking” [34-41]. Multiple different surgical approaches have been presented in the literature for this range of painful flatfoot pathologies. E.g., osteotomies, tendon transfers, gastrocnemius/Achilles lengthening, and arthrodesis.
The subtalar approach initially presented by Chambers in 1946 developed the concept of limiting subtalar joint motion. He accomplished this by utilizing an autologous bone graft inserted into the sinus tarsi, to prevent forward motion of the talus [42]. Subsequently many surgeons have published variations on the bone block theme for limiting subtalar joint motion, Subotnick in 1974 utilized a silicone elastomer block, Maxwell-Brancheau developed a titanium alloy cylinder, and others have suggested staples, or a variety of other materials such as PEEK (Polyetheretherketone). Critics of this minimally invasive approach cite the incidence of sinus tarsi pain, hard stop of motion pain, and the need for implant removal on a frequent basis [43-45].
In a review of the literature by Metcalfe et al. 76 arthroereisis papers were identified. Nine radiographic parameters were used to assess the clinical outcome of arthroereisis. Eight of the nine radiographic parameters reported showed significant improvement following arthroereisis reflecting both increased static arch height and joint congruency. Calcaneal inclination angle demonstrated the least change with only small increases following arthroereisis. Arthroereisis may develop complications such as sinus tarsi pain, device extrusion, and under correction. Complication rates range between 4.8% and 18.6% with unplanned removal rates between 7.1% and 19.3% across all device types [46,47].
Cheng [49], found through finite element analysis that, flexible flatfoot is attributed to subtalar joint instability. The data showed that the stresses were more concentrated, had increased localization, an abnormal stress distribution, and abnormal movement of subtalar joint. The talus was partially dislocated from the calcaneus in the posterior to medial aspect during loading. Furthermore, partial dislocation was also associated with loading at the forefoot, which is clinically recognized during gait observation. In ideal treatments of flexible flatfoot, implants should both stabilize the subtalar joint and facilitate physiologic relative motion; Extraosseous talotarsal stabilization (EOTTS) appears to allow achievement of this goal [50].
EOTTS as developed by Graham et al. [47] is applicable to the flexible flatfoot with talotarsal partial dislocation with rigid flatfoot being a contraindication. The rationale for the EOTTS approach is its stabilizing effect on the subtalar axis of joint motion and its ability to restore an improved biomechanical functionality to the rearfoot. It achieves this without prolonged rehabilitation as may be required with more traditional rearfoot flatfoot surgery. After flexible flatfoot has been treated by EOTTS, an improvement in deformity, pain, instability, and other symptoms in children is often observed [45].
Devices that perform the functions of talotarsal stabilization are inserted outside the bone and outside the joint. These are also known as a sinus tarsi stent. The goal of these devices is to maintain the articular facets of the talus on the calcaneus and navicular. They are inserted from lateral to medial across the sinus tarsi to the pivot point of the talotarsal axis. Two types of arthroereisis devices have been described in the literature Type 1 devices are similar to bone blocks, or silicone blocks, STA-PEG is an example of a type 1 device. Type 2 devices fill in the sinus tarsi with a variety of shapes and materials typically more conical laterally and more cylindrical medially in an attempt to match the anatomy of the sinus tarsi.
The device that has been implanted in this retrospective review is a novel type 2 device, in that it is made from human dermis that has been decontaminated, processed to be acellular, molded into cylindrical form of various thicknesses, freeze dried, and terminally sterilized. This cylindrical dermal stent maintains congruent alignment of the talotarsal mechanism and allows for triplane helicoidal motion that is necessary for the subtalar joint to act as designed by transmitting motion and energy from the leg to the foot.
Advantages of this device design as a sinus tarsi stent, include the following: it does not involve any alteration of bone and is joint sparing, it normalizes joint forces, and it decreases strain on the posterior tibial tendon, nerve, and plantar fascia. There are reports that correcting the position and function of the subtalar joint decreases pressure on the tarsal tunnel [46,47]. Secondarily, the implant allows for a degree of compression, eliminating the painful stop noted in stents made from metals and other manmade materials. Since it is an extracellular matrix, the graft allows for ingrowth of the talotarsal ligaments, and it does so in a corrected position over time. This essentially eliminates the causes that lead to the removal of other type 2 sinus tarsi stents; however, one should not anticipate correcting all components of a flexible flatfoot deformity with only subtalar arthroereisis or a sinus tarsi stent [48]. Correcting deforming forces such as Equinus, may also have to be addressed.
The talotarsal stent shifts the load from the joints of the medial column back toward the lateral column, decreases the moments at the talonavicular joint and the medial cuneiform–navicular joint, and decreases the forces in the medial extensions of the long plantar ligament and plantar aponeurosis. In this retrospective review it was found that patients recovered quickly from the implant stent surgery and resumed walking and exercise without pain within days of surgery, motivating them to increase distance walked without pain from their preimplant condition.
Methods and Materials
Overview of the procedure
The patient is positioned supine with a pillow under the ipsilateral hip to reduce external rotation of the foot. The Achilles tendon and gastrocnemius are evaluated with the Silfverskiold test (measuring the dorsiflexion (DF) of the foot at the ankle joint (AJ) with knee extended & flexed to 90 degrees. The test is considered positive when DF at the AJ is greater with knee flexed than extended. The test is performed with the patient seated or in supine.) to determine if a lengthening should be performed. Tight Achilles versus tight GastrocSoleus must be identified to determine type of lengthening to be performed.
A curved 1-cm skin incision is performed just 1 cm inferior and anterior to the tip of the lateral malleolus. Blunt dissection to the lateral ligament of the capsule allows for easier implantation. The sinus tarsus is debrided (fat plug removed) to facilitate implantation. A probe type instrument (freer elevator) is inserted through the sinus tarsi into the sinus canal from lateral to medial. until tenting is noted on the medial aspect of the foot. The probe can then be moved in a clockwise and counterclockwise direction to dilate the tarsal canal. A guide pin is then inserted into the sinus tarsi from lateral to medial just inferior to the posterior tibial tendon and slightly anterior inferior to the medial malleolus, until tenting was noted on the medial aspect of the foot.
The subtalar joint is put through its range of motion, in order to assess the amount of inversion and eversion available. Then the one at a time sizers are placed onto the guide wire, and placed into the talotarsal canal, the range of motion is tested with each sizer. The appropriate sizer should limit “abnormal/ excessive” STJ joint eversion. The appropriate sizer will allow the calcaneal subtalar joint complex to evert approximately 4degrees. If possible, use Intraoperative imaging (fluoroscopy) with guide wire in place as the implant is essentially radiolucent, to evaluate the degree of correction and placement of the trial implant. The trial implant is then removed, and the proper sized implant is inserted, imaging can be repeated, if necessary, with guide wire in place, but once confirmation of proper seating of implant, guidewire is removed. The lateral aspect of the implant is sutured into the deep capsule if desired, and layered closure is completed. Imaging shows Talo-navicular congruent with the foot loaded, do not overcorrect (Figures 1 & 2).

Post Operative Instructions: Limited weightbearing is recommended with a below-the-knee removable boot for 2 weeks. Suture removal typically between 10 to 14 days. Gradual return to activity as tolerated and use of a running type of shoe with foot orthotic during first 6 months postoperative.
Postoperative radiographs should be taken weightbearing at 2 weeks to document repair of talotarsal dislocation. Note: If Tend Achilles or Gastroc Soleus lengthening performed, boot or cast may be required for more than 2 weeks.
Results of Data Collection
Patient data collected with all HIPA information protected Figure 1.
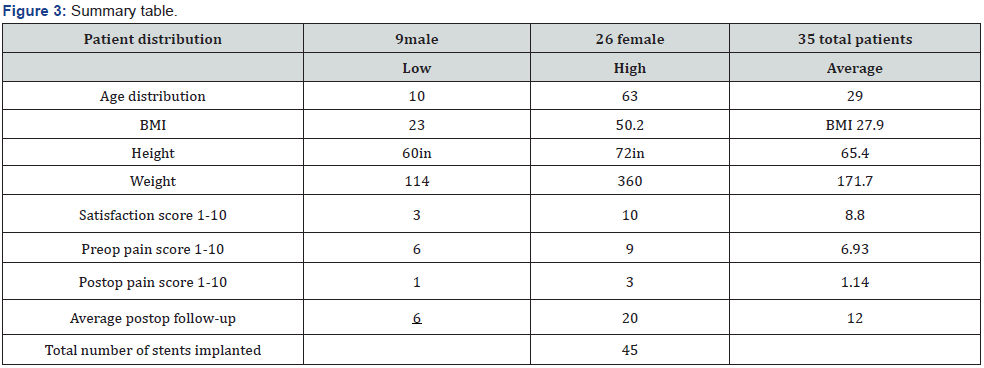
• 26 females, 9 males 35 individual patients, 11 patients had bilateral implants (separate surgical episodes).
• Average patient satisfaction (1 negative 10 more than satisfied), average score 8.8
• Average postoperative follow up 12 weeks. Date range of surgeries July 2020 thru Aug 2021
• Total number of human acellular dermal implants 45,
• Average age 29 years old, youngest 10years old-> oldest 63 years old
• Preoperative average pain score 6.93, Postoperative average pain score 1.14
• 4 mild postop complaints
• 1 keloid developed,
• 1 post operative incision site dehiscence,
• 2 surgical site pain,
• All resolved by 6 weeks postop.
• No implant removals required.
• Adjunctive procedures in 16 feet;
• 2 removal of failed device sinus tarsi,
• 3 gastrocsoleus recession,
• 6 chevron metatarsal 1st osteotomy,
• 1 kidner, 3 plantar fascial releases,
• 1 middle facet coalition resection
• 1 first metatarsal cuneiform fusion (Lapidus)
• Average BMI 27.9, Average height 65.4 inches, Average weight 171.7lbs
• Average surgical time 30min
ICD10 diagnostic codes for rearfoot issues
S93.314D dislocation / m25.571 pain /M21.961 equinus R
S93.315A /m25.572 / M21.962 L,
M20.11/.12 for hallux valgus,
M72.2 for plantar fasciitis,
Q66.89 for tarsal coalition (Figure 3)
Radiographic findings
Relaxed stance weightbearing radiographs should be the gold standard in the diagnosis of a flatfoot. Pre- and postoperative radiographic examinations were performed on surgical patients, the images collected were dorsal plantar views (DP) and Lateral weight bearing (LAT). Measurements tracked included calcaneal inclination angle, lateral talocalcaneal (LTC) angle, Meary’s angles, DP view, and Kite’s angle.
In the radiographic review, the reviewer focused on
Dorsoplantar (DP) view measurements included the talar second metatarsal along with the percentage talar navicular head uncovering. Did the talonavicular joint lateral view demonstrate increased subluxation aka increased Meary’s angle. Was there lateral displacement of the medial column (hallux, 1st metatarsal, medial cuneiform, and navicular). Was the talocalcaneal angle increased; if increased it would indicate medial deviation of talus with heel valgus occurring.: Evaluation of the talonavicular joint was their lateral subluxation (talar head no longer covered medially) and graded it moderate 25% to 50%, or severe >50%
Lateral radiograph evaluation included evaluation of the sinus tarsi, was it open or closed (Sinus tarsi closes during pronation as the lateral process of the talus moves anteriorly, during supination the sinus tarsi opens), talar declination angle, talar first metatarsal angle, calcaneal inclination, or pitch angle, Meary’s angle, the level of talonavicular joint dorsal subluxation. Cyma line close to smooth S-shaped curve. The expectation of the surgeons was to see on the preoperative lateral radiograph; increased TN joint subluxation, decreased calcaneal inclination angle, (which tends to indicate longitudinal medial arch collapse), increased talocalcaneal angle demonstrating plantar deviation of talus. 85-90%TN congruity should be observed on an DP(AP) view of the loaded foot intraoperatively.
Based on the radiographic results,
• Talocalcaneal angle lateral view:
• mean preoperative = 38.3° range 35°-41°
• mean with stent postoperative= 33.02 range 30°-36°.
• Kite’s angle lateral view reduced significantly, indicating a lifting of the talus in a more horizontal position.
• Talocalcaneal angle Dorsal Plantar (Kite’s angle)
• mean preoperative = 37.6°, range= 30° -45°
• mean postoperative stent implanted 18.4° with a range of 12° - 25 (Figure 4).
• Calcaneal inclination angle
• preoperative mean is 11.5° with a range of 9° - 14°,
• mean postoperative calcaneal inclination angle = 16° with a range of 14° - 18°.
• Improved but remaining below the normal angle range of 20° to 40°,
• Indicating moderate restoration of the medial arch.
• Meary’s angle in lateral view
• Mean preoperative was 16.6° with a range of 10° -24°,
• Postoperative lateral Meary’s angle mean was 2.6° with a range of 1° -4°.
• Demonstrating a solid reduction of the dorsal subluxation Talonavicular joint complex.
• Meary’s angle in DP view
• Mean preoperative was 28.4° with a range of 17° - 44°.
• Mean postoperative was 31.6° with a range of 30° - 33°.
• In a normal foot, Meary’s angle is close to zero degrees,
• This indicates that the angle reduced significantly, solid improvement,
• With reduction of the heel valgus position.
• Talar declination angle
• Mean preoperative was 31.1° range 24° to 37°, and
• Mean postoperatively stent 17.4° range 16° to 19°,
• Talar declination angle reduced significantly, indicating talus in a more horizontal position.

The radiological findings demonstrated that the TaloTarsal stent significantly improved positioning and alignment of the subtalar and talonavicular joints, by driving the heel back to its normal neutral position, and by driving at the same time the medial foot ray (navicular, medial cuneiform, first metatarsal, great toe) medially, back to their normal alignment. The subtalar joint is a single axis joint performing as a hinge between the talus and calcaneus. With talotarsal stent, there was only a moderate improvement in the observed visual appearance of the medial arch.
Discussion
For over 50 years a variety of devices and materials have been inserted into the subtalar joint to treat the painful flatfoot. Citing just a few studies it is clear this approach has a success and merit with minimal risk. The latest iteration of utilizing lyophilized acellular human dermis in a tight cylindrical form eliminates the issues of hard stop pain and need for implant removal. Thus, this method has eliminated the complications discussed in many published papers.
To name a few author of success in treating flexible flatfoot we can look at the outcomes of these authors:
Vedantam et al. reported STA-PEG implants resulting in satisfactory outcomes in 96% of feet, in a study of 78 children with neuromuscular flexible flatfeet where 140 arthroereisis procedures were performed. Assessment was based on radiological angle improvement as well as reduction of hindfoot valgus and pain Giannini et al. reported 4-year results of subtalar arthroereisis for 21 children with bilateral flexible flatfeet using a bioresorbable implant, finding improvement in clinical results, radiological angles and footprint grades [50,51] Fernandez de Retana et al. found that the Viladot footprints and radiographic angles improved post operatively [52-57].
The Viladot 4 category footprint classification used is a simple visual model which does not allow quantifying of pre and post operative differences. Many other publications for subtalar arthroereisis include Achilles’ tendon lengthening [58,59]. Overall, these studies have demonstrated an increase in dorsiflexion, decreased foot pain, improvement of radiographic angles and improvement in footprint following this procedure [51-59].
One concern with current state of the EOTTS implant is the question of second surgery for implant removal. The stent can mechanically stabilize the hindfoot and allow activity in the early stage [60]. There is debate about device removal. Since the overall goal of treatment is to restore functioning of the joint, we propose the devices do not need to be removed until the bony structure reaches maturity. The younger the patient, functional adaptation of the joints occurs and need for implant lessens. Complications requiring the need for arthroereisis implant removal rates has been stated in the literature as one significant reason for the slow adaption of this procedure for flexible flatfoot in the pediatric population. Stated reasons for removal run the gamut from generalized discomfort,malposition or extrusion, lack of correction, overcorrection loosening, breakage, or persistent focused sinus tarsi pain or tenderness. Baker et al. [42] in a retrospective analysis of the survivability of absorbable versus nonabsorbable subtalar joint arthroereisis implants, state that overall survival rates were on average 83% for absorbable implants and 81% for nonabsorbable implants.
Zarat & Myerson [34], in 2003, reported utilizing the MBA implant on 43 feet, with 31 inserted in children and 12 in adults. They report 7 patients complained of postoperative pain and attributed this to implant impingement on the posterior facet or insertion of an incorrectly sized implant. Four patients had their implants removed. Schon in 2007, discusses complications associated with the MBA implant by reviewing the shape of the sinus tarsi on CT scan. He reports the sinus tarsi is more conical than cylindrical. Schon concludes,complications associated with such implants are attributed to the conflicting shapes causing an uneven distribution of forces, therefore, resulting in pain [35]. Several authors over the years offered alternative shapes and materials such as Viladot et al 2003 or others offered Bioabsorbable shaped devices or non-absorbable shapes that were more conical, each variation brought a variety of potential and documented complications.
If forces continue to act excessively on tissues, those tissues will create a defense mechanism in an attempt to handle those excessive forces as described by Wolff and Davis [61,62]. Eventually, a critical threshold is reached when the tissues can no longer compensate, and tissue failure occurs. Other tissues will be forced to compensate for the loss of the primary stabilizing positioning, leading to overwhelming force and pressure within the affected joint causing an inflammatory reaction.


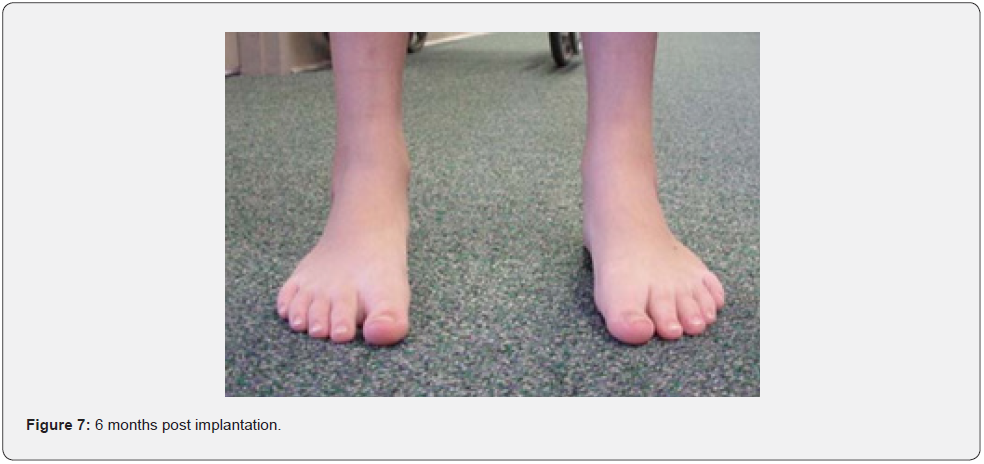
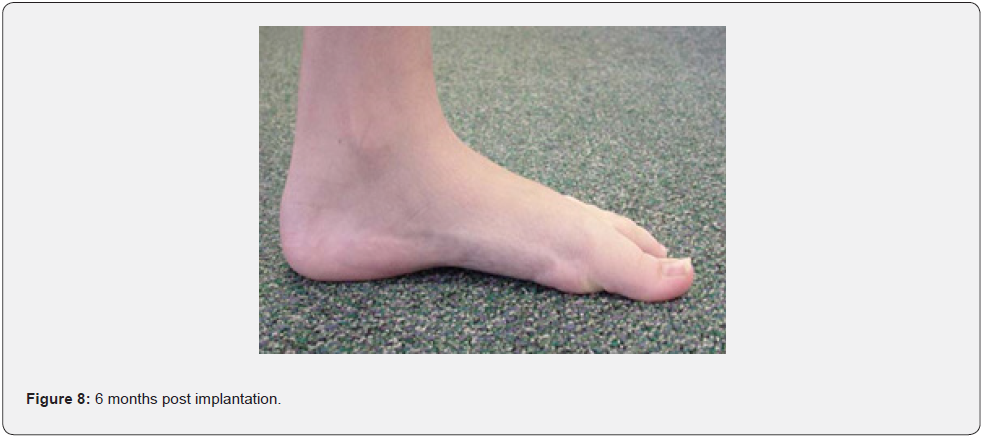
Repair of talotarsal dislocation with a sinus tarsi stent provides a powerful 3-dimensional correction of the rearfoot instability, by repositioning the talus in its physiological position, preventing it from slipping anterior, medial, and plantar. With the Spiralup™ design of human acellular dermis there is ingrowth of the talocalcaneal ligaments increasing long term sustainability of the correction. This essentially eliminates the need for implant removal. The Spiralup™ graft is configured to the shape of the sinus tarsi, its size (length, diameter) can be adjusted intraoperatively, it is available in several diameters (7,9 & 11mm), and it has no MRI restrictions. There are many advantages to utilizing a talotarsal stent. The procedure is straight forward with minimal learning curve, it is minimally invasive, patient recovery time is minimal, and it offers shorter healing time than any osteotomy or arthrodesis procedure. There is no risk of neurovascular structure damage, malunion or nonunion, and this design minimizes risk of subsidence. This procedure can be used in conjunction with other procedures to maximize positive outcomes for the patient. In simple terms the stent expands the subtalar joint vertically by elevating the head of the talus, which improves talo navicular alignment by realigning the medial longitudinal arch. This improves tendon/ligament function, reduces skeletal stress, and allows for a more normal gait cycle without inflammatory compensations. With repositioning being maintained the tibialis posterior can truly function as a supinatory stabilizer during gait (Figures 5-8)
In medicine treating any disease with early identification and intervention utilizing a method proven to achieve the desired outcome that is measurable and assumes minimal risk is most desired. If the misaligned foot is not treated and excessive forces on the tissues continue to achieve critical thresholds the tissues can no longer compensate. This ultimately leads to significant inflammation, shin splints, growing pains, knee discomfort, and hip pain. This leads to more serious conditions such as osteoarthritis, fasiopathies, posterior tibial tendon insufficiency, first ray deformities, and tarsal tunnel syndrome. These syndromes limit activity, where the patient then becomes susceptible to increased BMI advancing into metabolic syndrome due to lack of physical activity.
There is a long evolution in the flatfoot from simple malalignment to skeletal instability manifesting in a multitude of joints over years. EOTTS should be considered a conservative surgical option prior to aggressive osseous and tendon reconstruction or at the very least an adjunctive procedure to improve patient outcomes. The evidence from a plethora of peer reviewed, published studies provides significant evidence that extra-osseous talotarsal stabilization provides safe improved functional outcomes [63]. With the advent of a human dermal tissue EOTT implant, time has come to embrace this minimally invasive, early intervention for pediatric flatfeet, to reduce the long-term effects of the untreated flatfoot and provide our patients with an improved lifetime of pain free ambulation [64-69]. In the adult flexible flatfoot Posterior Tibial Tendon Dysfunction (PTTD) may develop along with the tendon pathology repairing the tendon, along with repositioning of the Talar-Calcaneal- Navicular relationship will allow for control of the rearfoot position.
Conclusion
In this retrospective review of the Acellular lyophilized dermal scaffold (SpiralUP™Anika,Inc) extraosseous implant the removal rate was zero percent 0 out of 46 implants had to be removed. Pediatric flexible flatfoot remains a poorly defined pathology with little agreement regarding treatment [58,70]. Metcalfe et al regarding treatment. Arthroereisis represents a minimally invasive procedure capable of correcting flexible flatfoot through a combination of static, dynamic and proprioceptive mechanisms. As a treatment option it continues to polarize opinion. A focus on internal joint congruency rather than simple anthropometric measures may sharpen our understanding. There is a growing body of evidence linking abnormalities in joint malalignment to the [71-74] development of osteoarthrosis. More recent observational studies have demonstrated a greater incidence of osteoarthrosis in flat feet when compared with controls [75-128].
Acknowledgement
We would like to thank the creators of this talotarsal stent implant and all of the authors who have contributed to the body of knowledge to improve patient outcomes.
Conflicts of interest statement
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. Vern Christensen DPM, and JJ VanYperen DPM. Bruce Werber DPM does have a financial interest as he is one of the inventors of the Acellular dermal scaffold stent implant and receives royalties and a financial grant to collate the data.
- Research Article
- Abstract
- Introduction
- Factors involved in development of PTOA
- Timeline of the pathogenic processes following joint injury
- Pathological Changes in Post-Traumatic OA
- Pathologic changes in articular cartilage
- Pathologic changes in synovium
- Pathologic changes in bone
- Opportunities for early intervention and Treatment
- Conflict of Interest
- References
References
- Hake D, Bregman P (2016) Economic impact of congenital/Acquired talotarsal joint dislocation and the role of extraosseous talotarsal stabilization. J Minim Invas Orthop 2(1): e13.
- Pleis JR, Lucas JW, Ward BW (2009) Summary health statistics for U.S. adults: National Health Interview Survey, 2008. Vital Health Stat 10(242): 1-157.
- DeFrances CJ, Lucas CA, Buie VC, Aleksandr Golosinskiy (2006) National Hospital Discharge Survey. Natl Health Stat Report 30(5): 1-20.
- Hing E, Hall MJ, Xu J (2008) National Hospital Ambulatory Medical Care Survey: 2006 outpatient department summary. Natl Health Stat Report 6(4): 1-31.
- Bresnahan PJ, Juanto MA (2020) Pediatric Flatfeet-A Disease Entity That Demands Greater Attention and Treatment. Front Pediatr 8: 19.
- Michael E (2017) Graham Extra-Osseous Talotarsal Joint Stabilization (EOTTS) in the Treatment of Hyperpronation Syndromes. Update in Management of Foot and Ankle Disorders.
- Deland JT (2008) Acquired flat foot deformity. J Am Acad Orthop Surg 16(7): 399-406.
- Pinney SJ, Lin SS (2006) Current concept review: acquired adult flatfoot deformity. Foot Ankle Int 27(1): 66-75.
- Myerson MS (1996) Adult acquired flatfoot deformity. J Bone Joint Surg Am 78: 780-792.
- Root ML, Orien WP, Weed JH (1977) Normal and Abnormal Function of the Foot. Clinical Biomechanics Corp, Los Angeles, CA, USA.
- Tiberio D (1987) The effect of excessive subtalar joint pronation on patellofemoral mechanics: a theoretical model. J Orthop Sports Phys Ther 9(4): 160-165.
- Graham ME, Parikh R, Goel V, Devdatt Mhatre, Aaron Matyas (2011) Stabilization of joint forces of the subtalar complex via HyProCure sinus tarsi stent. J Am Podiatr Med Assoc 101(5): 390-399.
- Brody DM (1982) Techniques in the evaluation and treatment of the injured runner. Orthop Clin North Am 13(3): 541-558.
- Kirby KA (2001) Subtalar joint axis location and rotational equilibrium theory of foot function. J Am Podiatr Med Assoc 91(9): 465-487.
- Levens AS, Inman VT, Blosser JA (1948) Transverse rotation of the segments of the lower extremity in locomotion. J Bone Join Surg Am 30A(4): 859-872.
- Nguyen AD, Shultz SJ (2009) Identifying relationships among lower extremity alignment characteristics. J Athl Train 44(5): 511-518.
- Buchbinder MR, Napora NJ, Biggs EW (1979) The relationship of abnormal pronation to chondromalacia of the patella in distance runners. J Am Podiatry Assoc 69(2): 159-162.
- Giannini S, Catani F, Ceccarelli F, M Girolami, M G Benedetti (1992) Kinematic and isokinetic evaluation of patients with flat foot. Ital J Orthop Traumatol 18(2): 241-251.
- Gross KD, Felson DT, Niu J, David J Hunter, Ali Guermazi, et al. (2011) Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care Res (Hoboken) 63(7): 937-944.
- Khamis S, Yizhar Z (2007) Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 25(1): 127-134.
- Levinger P, Menz HB, Fotoohabadi MR, Julian A Feller, John R Bartlett, et al. (2010) Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res 3: 29.
- Davitt JS, Beals TC, Bachus KN (2001) The effects of medial and lateral displacement calcaneal osteotomies on ankle and subtalar joint pressure distribution. Foot Ankle Int 22(11): 885-889.
- Campbell ST, Reese KA, Ross SD, McGarry MH, Leba TB, et al. (2014) Effect of graft shape in lateral column lengthening on tarsal bone position and subtalar and talonavicular contact pressure in a cadaveric flatfoot model. Foot Ankle Int 35(11): 1200-1208.
- Rockar PA (1995) The subtalar joint: anatomy and joint motion. J Orthop Sports Phys Ther 21(6): 361-372.
- Graham ME, Parikh R, Goel V, Mhatre D, Matyas A (2011) Stabilization of joint forces of the subtalar complex via HyProCure sinus tarsi stent. J Am Podiatr Med Assoc 101(5): 390-399.
- Wagner UA, Sangeorzan BJ, Harrington RM, Tencer AF (1992) Contact characteristics of the subtalar joint: load distribution between the anterior and posterior facets. J Orthop Res 10(4): 535-543.
- Ronneberger O, Fischer P, Brox T (2015) U-Net: Convolutional Networks for Biomedical Image Segmentation. In: Navab N, Hornegger J, Wells W, Frangi A, editors. Medical Image Computing and Computer-Assisted Intervention – MICCAI 2015. MICCAI 2015. Lecture Notes in Computer Science. Springer, Cham 9351.
- K A Kirby (2001) Subtalar joint axis location and rotational equilibrium theory of foot function. J Am Podiatr Med Assoc 91(9): 465-487.
- Hutton WC, Dehanendran M (1981) The mechanics of normal and hallux valgus feet-A quantitative study. Clin Ortho 157: 7-13.
- Graham ME, Parikh R, Goel V, Mhatre D, Matyas A (2011) Stabilization of joint forces of the subtalar complex via HyProCure sinus tarsi stent. J Am Podiatr Med Assoc 101(5): 390-399.
- Dare DM, Dodwell ER (2014) Pediatric flatfoot: cause, epidemiology, assessment, and treatment. Curr Opin Pediatr 26(1): 93-100.
- Walters JL, Mendicino SS (2014) The flexible adult flatfoot: anatomy and pathomechanics. Clin Podiatr Med Surg 31(3): 329-336.
- Vogler H (1987) Subtalar joint blocking operations for pathological pronation syndromes . Comprehensive Textbook of Foot Surgery. McGlamery (ed), Williams & Wilkins, Baltimore, USA, pp. 466-482.
- Zarat DI, Myerson MS (2003) Arthroereisis of the subtalar joint. Foot Ankle Clin 8(3): 605-617.
- Schon LC (2007) Subtalar arthroereisis: a new exploration of an old concept. Foot Ankle Clin 12(2): 329-339.
- Reiner Husain ZS, Fallat LM (2002) Biomechanical analysis of Maxwell-Brancheau J Foot Ankle Surg 41(6): 352-358.
- Maxwell JR, Carro A, Sun C (1999) Use of the Maxwell-Brancheau arthroereisis implant for the correction of posterior tibial ten-don dysfunction. Clin Podiatr Med Surg 16(3): 479-489.
- George A Arangio, Kristy L Reinert, Eric P Salathe (2004) A bio-mechanical model of the effect of sub-talar arthroereisis on the adult flexible flat foot. Clin Biomech (Bristol, Avon) 19(8): 847-852.
- Chang TJ, Lee J (2007) Subtalar joint arthroereisis in adult-acquired flatfoot and posterior tibial tendon dysfunction. Clin Podiatr Med Surg 24(4): 687-697.
- Christensen JC, Campbell N, DiNucci K (1996) Closed kinetic chain tarsal mechanics of subtalar joint arthroereisis. J Am Podiatr Med Assoc 86(10): 467-473.
- Chambers EF (1946) An operation for the correction of the flexible flatfoot in adolescents West J Surg Obstet Gynecol 54: 77-86.
- Baker LD, Hill LM (1964) Foot alignment in the cerebral palsy patient. J Bone Joint Surg 46A: 1-15.
- LiLievre J (1970) Current concepts and cor-rection in the valgus foot. Clin Orthop 70: 43-55.
- Subotnick SL (1974) The STJ lateral extraarticu-lar arthroereisis: a preliminary report. J Am Podiatr Assoc 64(9): 701-711.
- Bresnahan PJ, Chariton JT, Vedpathak A (2013) Extraosseous talo tarsal stabilization using HyProCure(R): preliminary clinical outcomes of a prospective case series. J Foot Ankle Surg 52(2): 195-202.
- Graham ME, Jawrani NT, Goel VK (2011) The effect of HyProCure((R)) sinus tarsi stent on tarsal tunnel compartment pressures in hyperpronating feet. J Foot Ankle Surg 50(1): 44-49.
- Graham ME, Jawrani NT (2012) Extraosseous talotarsal stabilization devices: a new classification system. J Foot Ankle Surg 51(5): 613–619.
- Ozan F, Dogar F, Gencer K, Koyuncu S, Vatansever F, et al. (2015) Symptomatic flexible flatfoot in adults: subtalar arthroereisis. Ther Clin Risk Manag 11: 1597-602.
- Cheng X, Deng Z, Song W, Liu J, Li W (2022) Effects of extraosseous talotarsal stabilization on the biomechanics of flexible flatfoot subtalar joints in children: a finite element study. Int J Res Orthop 8(1): 5-13.
- Xu J, Zhang Y, Muhammad H, Wang X, Huang J, et al. (2015) In vivo three-dimensional analysis of hindfoot kinematics in stage II PTTD flatfoot. J Orthop Sci 20(3): 488-497.
- Vedantam R, Capelli AM, Schoenecker PL (1998) Subtalar arthroereisis for the correction of planovalgus foot in children with neuromuscular disorders. J Pediatr Orthop 18(3): 294-298.
- Giannini S, Ceccarelli F, Benedetti MG, Catani F, Faldini C (2001) Surgical treatment of flexible flatfoot in children:a four-year follow-up study. J Bone Joint Surg Am 83: 73-79.
- Fernandez de Retana P, Alvarez F, Viladot R (2010) Subtalar arthroereisis in pediatric flatfoot reconstruction. Foot Ankle Clin N Am 15(2): 323-335.
- Gutierrez PR, Lara MH (2005) Giannini: prosthesis for flatfoot. Foot Ankle Int 26(11): 918-926.
- Cicchinelli LD, Huerta JP, Garcıa-Carmona FJ, Morato DF (2008) Analysis of gastrocnemius recession and medial column procedures as adjuncts in arthroereisis for the correction of pediatric pesplanovalgus: a radiographic retrospective study. J Foot Ankle Surg 47(5): 385-391.
- Needleman RL (2005) Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int 26: 336-346.
- Viladot A (1992) Surgical treatment of the child’s flatfoot . Clin Orthop 283: 34-38.
- Metcalfe SA, Bowling FL, Reeves ND (2011) Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int 32(12): 1127-1139.
- Scharer BM, Black BE, Sockrider N (2010) Treatment of painful pediatric flatfoot with Maxwell-Brancheau subtalar arthroereisis implant a retrospective radiographic review. Foot Ankle Spec 3(2): 67-72.
- Shin J, Yue N, Untaroiu CD (2012) A finite element model of the foot and ankle for automotive impact applications. Ann Biomed Eng 40(12): 2519-2531.
- Wolff J (2010) The classic: on the inner architecture of bones and its importance for bone growth 1870. Clin Orthop Relat Res 468(4): 1056-1065.
- Davis HG (1867) Conservative Surgery. D. Appleton & Co, New York, USA.
- Graham ME (2017) Medical necessity and evidence basis for extra-osseous talotarsal joint stabilization. Clin Surg 2: 1-8.
- Stahelin AC, Weiler A, Rufenacht H, Hoffman R, Geissmann A, et al. (1997) Clinical degradation and biocompatibi-lity of different bioabsorbable interference screws: a report of six cases. Arthroscopy 13(2): 238-244.
- Sabonghy EP, Wood RM, Ambrose CG, McGarvey WC, Clanton TO (2003) Tendon transfer fixation: comparing a tendon-to-tendon technique vs. bioabsorbable inter-ference fit screw fixation. Foot Ankle 24(3): 260-262.
- Kilicoglu O, Demirhan M, Akman S, Atalar AC, Ozsoy S, et al. (2003) Failure strength of bioabsorbable interference screws: effects of in vivo degradation for 12 weeks. Knee Surg Sports Traumatol Arthrosc 11(4): 228-234.
- Lajtai G, Schmiedhuber G, Unger F, G Aitzetmuller, M Klein, et al. (2001) Bone tunnel remodeling at the site of biodegradable interference screws used for anterior cruciate ligament recon-struction: 5-year follow-up. Arthroscopy 17(6): 597-602.
- MacDonald P, Arneja S (2003) Biodegradable screw presents as a loose intra-articular body after anterior cruciate ligament reconstruction. Arthroscopy 19(6): E22-E24.
- Martinek V, Friederich NF (1999) Tibial and pre-tibial cyst formation after anterior cruciate ligament reconstruction with bioabsorbable interference screw fixation. Arthroscopy 15(3): 317-320.
- Foot & Ankle International Copyright _ 2011 by the American Orthopaedic Foot & Ankle Society.
- Anne Reilly K, Louise Barker K, Shamley D, Sandall S (2006) Influence of foot characteristics on the site of lower limb osteoarthritis. Foot Ankle Int 27(3): 206-211.
- Harris WH (2009) The correlation between minor or unrecognized developmental deformities and the development of osteoarthritis of the hip. Instr Course Lect 58: 257-259.
- Pagenstert G, Knupp M, Valderrabano V, Hintermann B (2009) Realignment surgery for valgus ankle osteoarthritis. Oper Orthop Traumatol 21(1): 77-87.
- Viitanen MJ, Wilson AM, McGuigan HR, Rogers KD, May SA (2003) Effect of foot balance on the intra-articular pressure in thedistal interphalangeal joint in vitro. Equine Vet J 35(2): 184-189.
- Ilahi OA, Kohl HW 3rd (1998) Lower extremity morphology and alignment and risk of overuse injury. Clin J Sport Med 8(1): 38-42.
- Kaufman KR, Brodine SK, Shaffer RA, Johnson CW, Cullison TR (1999) The effect of foot structure and range of motion on musculoskeletal overuse injuries. Am J Sports Med 27(5): 585 –593.
- Menz, HB, Munteanu SE, Zammit GV, Landorf KB (2009) Foot structure and function in older people with radiographic osteoarthritis of the medial midfoot. Osteoarthritis Cartilage 18(3): 317-322.
- Staheli LT (1986) Philosophy of care. Pediatr Clin North Am 33: 1269 –1275.
- Panos Megremis, Orestis Megremis (2019) arthroereisis for symptomatic Flex flatfoot w xray assessment. J Foot Ankle Surg 58(5): 904-915.
- Wong DWC, Wang Y, Chen TL W, Leung A K L, Zhang M (2017) Biomechanical consequences of subtalar joint arthroereisis in treating posterior tibial tendon dysfunction: a theoretical analysis using finite element analysis. Comput Method Biomec 20(14): 1525-1532.
- D H, P B (2016) Economic Impact of Congenital/ Acquired Talotarsal Joint dislocation and the role of extraosseous talotarsal stabilization. Journal Minimal invasive orthopedics.
- Cheng X, Deng Z, Song W, Liu J, Li W (2021) Effects of extraosseous talotarsal stabilization on the biomechanics of flexible flatfoot subtalar joints in children: a finite element study. Int J Res Orthop 8: 5–13
- Jenkins J L (2013) Extra-osseous talotarsal stabilization and sinus tarsi impingement syndrome: case report. J Foot Ankle Res 6(1): P6–P6.
- Wong D W C, Wang Y, Niu W, Zhang M (2020) Finite element analysis of subtalar joint arthroereisis on adult-acquired flexible flatfoot deformity using customised sinus tarsi implant. J Orthop Transl 27: 139–145.
- Nevalainen M T, Roedl J B, Zoga A C, Morrison W B (2016) Imaging findings of arthroereisis in planovalgus feet. Radiol Case Rep 11(4): 398–404.
- Bresnahan PJ, Juanto M A (2020) Pediatric Flatfeet—A Disease Entity That Demands Greater Attention and Treatment. Front Pediatr 8: 19.
- Yvonne-Mary Papamerkouriou, Rohan Rajan , Samena Chaudhry, Preetham Kodumuri , Helen Evans, et al. (2019) Prospective Early Clinical, Radiological, and Kinematic Pedobarographic Analysis Following Subtalar Arthroereises for Paediatric Pes Planovalgus. Cureus 11(12): e6309.
- Baker JR, Klein EE, Weil L, Weil L S, Knight J M (2013) Retrospective Analysis of the Survivability of Absorbable Versus Nonabsorbable Subtalar Joint Arthroereisis Implants. Foot Ankle Specialist 6(1): 36–44.
- Kirby K (2001) STJ axis location rotational equilibrum theroy of foot function. J Am Podiatr Med Assoc 91(9): 465-487.
- Metcalfe SA, Bowling FL, Reeves N D (2011) Subtalar Joint Arthroereisis in the Management of Pediatric Flexible Flatfoot: A Critical Review of the Literature. Foot Ankle Int 32(12): 1127–1139.
- Fırat Ozan, Fatih Dogar, Kursat Gencer , Semmi Koyuncu, Fatih Vatansever, et al. (2015) Symptomatic flexible flatfoot in adults: subtalar arthroereisis. Ther Clin Risk Manag 11: 1597–1602.
- Kolodziej L, Summers RK, Graham ME (2019) The effect of extra-osseous talotarsal stabilization (EOTTS) to reduce medial knee compartment forces – An in vivo study. Plos One 14(12): e0224694.
- Zhu Y, Xu X (2015) Treatment of Stage II Adult Acquired Flatfoot Deformity with Subtalar Arthroereises. Foot Ankle Specialist 8(3): 194–202.
- Graham M E (2018) Update in Management of Foot and Ankle Disorders.
- Davitt JS, Beals TC, Bachus KN (2001) The effects of medial and lateral displacement calcaneal osteotomies on ankle and subtalar joint pressure distribution. Foot Ankle Int 22(11): 885-889.
- Campbell ST, Reese KA, Ross SD, McGarry MH, Leba TB, et al. (2014) Effect of graft shape in lateral column lengthening on tarsal bone position and subtalar and talonavicular contact pressure in a cadaveric flatfoot model. Foot Ankle Int 35(11): 1200-1208.
- Rockar PA (1995) The subtalar joint: anatomy and joint motion. J Orthop Sports Phys Ther 21(6): 361-372.
- Graham ME, Parikh R, Goel V, Mhatre D, Matyas A (2011) Stabilization of joint forces of the subtalar complex via HyProCure sinus tarsi stent. J Am Podiatr Med Assoc 101(5): 390-399.
- Wagner UA, Sangeorzan BJ, Harrington RM, Tencer AF (1992) Contact characteristics of the subtalar joint: load distribution between the anterior and posterior facets. J Orthop Res 10(4): 535-543.
- Dare DM, Dodwell ER (2014) Pediatric flatfoot: cause, epidemiology, assessment, and treatment. Curr Opin Pediatr 26(1): 93-100.
- Walters JL, Mendicino SS (2014) The flexible adult flatfoot: anatomy and pathomechanics. Clin Podiatr Med Surg 31(3): 329-336.
- Graham ME, Jawrani NT, Chikka A, Rogers RJ (2012) Surgical treatment of hyperpronation using an extraosseous talotarsal stabilization device: radiographic outcomes in 70 adult patients. J Foot Ankle Surg 51(5): 548-555.
- Kobayashi T, Saka M, Suzuki E, Yamazaki N, Suzukawa M, et al. (2014) In vivo kinematics of the talocrural and subtalar joints during weightbearing ankle rotation in chronic ankle instability. Foot Ankle Spec 7(1): 13-19.
- Bresnahan PJ, Chariton JT, Vedpathak A (2013) Extraosseous talotarsal stabilization using HyProCure(R): preliminary clinical outcomes of a prospective case series. J Foot Ankle Surg 52(2): 195-202.
- Graham ME (2013) Congenital talotarsal joint displacement and pes planovalgus: evaluation, conservative management, and surgical management. Clin Podiatr Med Surg 30(4): 567-581.
- Graham ME, Jawrani NT, Goel VK (2022) Effect of extra-osseous talotarsal stabilization on posterior tibial. International Journal of Research in Orthopaedics Vol 8(1): 13.
- Nelson SC, Haycock DM, Little ER (2014) Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg 43(3): 144-155.
- Badie F, Katouzian HR, Rostami M (2018) A non-invasive measurement of the knee contact force using a subject-specific musculoskeletal model to investigate osteotomy. J Med Eng Technol 42(4): 251-258.
- Ruozi B, Belletti D, Manfredini G, Tonelli M, Sena P, et al. (2013) Biodegradable device applied in flatfoot surgery: comparative studies between clinical and technological aspects of removed screws. Mater Sci Eng C Mater Biol Appl 33(3): 1773-1782.
- Camacho DL, Ledoux WR, Rohr ES, Sangeorzan BJ, Ching RP (2002) A three-dimensional, anatomically detailed foot model: a foundation for a finite element simulation and means of quantifying foot-bone position. J Rehabil Res Dev 39(3): 401-410.
- Cheung JT, Zhang M, Leung AK, Fan YB (2005) Three- dimensional finite element analysis of the foot during standing--a material sensitivity study. J Biomech 38(5): 1045-1054.
- Guiotto A, Sawacha Z, Guarneri G, Avogaro A, Cobelli C (2014) 3D finite element model of the diabetic neuropathic foot: a gait analysis driven approach. J Biomech 47(12): 3064-3071.
- Wang Z, Imai K, Kido M, Ikoma K, Hirai S (2014) A finite element model of flatfoot (Pes Planus) for improving surgical plan. Conf Proc IEEE Eng Med Biol Soc pp. 844-847.
- De Pellegrin M, Moharamzadeh D, Strobl WM, Biedermann R, Tschauner C, et al. (2014) Subtalar extra- articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop 8(6): 479-487.
- Graham ME, Jawrani NT (2012) Extraosseous talotarsal stabilization devices: a new classification system. J Foot Ankle Surg 51(5): 613-619.
- Yu JH, Wang YT, Lin CL (2018) Customized surgical template fabrication under biomechanical consideration by integrating CBCT image, CAD system and finite element analysis. Dent Mater J 37(1): 6-14.
- Brekelmans WA, Poort HW, Slooff TJ (1972) A new method to analyse the mechanical behaviour of skeletal Acta Orthop Scand 43(5): 301-317.
- Fitzgerald RH, Vedpathak A ( 2013) Plantar pressure distribution in a hyperpronated foot before and after intervention with an extraosseous talotarsal stabilization device-a retrospective study. J Foot Ankle Surg 52(4): 432-443.
- Christensen JC, Campbell N, DiNucci K (1996) Closed kinetic chain tarsal mechanics of subtalar joint arthroereisis. J Am Podiatr Med Assoc 86(10): 467-473.
- Zanolli DH, Glisson RR, Nunley JA, Easley ME (2014) Biomechanical assessment of flexible flatfoot correction: comparison of techniques in a cadaver model. J Bone Joint Surg Am 96(6): e45.
- Razak AH, Zayegh A, Begg RK, Wahab Y (2012) Foot plantar pressure measurement system: a review. Sensors (Basel) 12(7): 9884-9912.
- Chockalingam N, Healy A, Naemi R, Burgess- Walker P, Abdul Razak AH, et al. (2013) Comments and reply to: Foot plantar pressure measurement system: a review. Sensors (Basel) 13(3): 3527-3528.
- Chen WM, Park J, Park SB, Shim VP, Lee T (2012) Role of gastrocnemius-soleus muscle in forefoot force transmission at heel rise - A 3D finite element analysis. J Biomech 45(10): 1783-1789.
- Xu J, Zhang Y, Muhammad H, Wang X, Huang J, et al. (2015) In vivo three-dimensional analysis of hindfoot kinematics in stage II PTTD flatfoot. J Orthop Sci 20(3): 488-497.
- Shin J, Yue N, Untaroiu CD (2012) A finite element model of the foot and ankle for automotive impact applications. Ann Biomed Eng 40(12): 2519-2531.
- Liu Q, Zhao G, Yu B, Ma J, Li Z, et al. (2016) Effects of inferior tibiofibular syndesmosis injury and screw stabilization on motion of the ankle: a finite element study. Knee Surg Sports Traumatol Arthrosc 24(4): 1228-1235.
- Yuan CS, Chen W, Chen C, Yang GH, Hu C, et al. (2015) Effects on Subtalar Joint Stress Distribution After Cannulated Screw Insertion at Different Positions and Directions. J Foot Ankle Surg 54(5): 920-926.
- Papamerkouriou Y, Rajan R, Chaudhry S, Preetham Kodumuri, Helen Evans, et al. (2019) Prospective Early Clinical, Radiological, and Kinematic Pedobarographic Analysis Following Subtalar Arthroereises for Paediatric Pes Planovalgus. Cureus 11(12): e6309.






























