Review of Synovial Fluid Properties and Measurement
Bader E Alabkary* and Mohammad A Zohdy
Department of Computer Science & Engineering, Oakland University, USA
Submission:July 01, 2022; Published: July 11, 2022
*Corresponding author: Bader E Alabkary, Department of Computer Science & Engineering, Oakland University, Rochester, MI 48309, USA
How to cite this article: Bader E A, Mohammad A Z. Review of Synovial Fluid Properties and Measurement. Ortho & Rheum Open Access J. 2022; 20(2): 556033. DOI: 10.19080/OROAJ.2022.20.556033
Abstract
Arthritis is an inflammation in one or more of the body joints. Its chief symptoms are pain and stiffness in the affected area. The accompanying pain in knee joints occurs due to stiffening joint fluids which are known as synovial fluids. Its kinematics identifies the compressive load and articular cartilage characteristics. This paper highlights synovial fluid properties and explores the lubrication mechanisms of synovial fluid for age-related changes while accounting for gender differences. Further, this paper reviews extant studies that were conducted on automated detection based on deep learning and acoustic monitoring of joint health and response to measurement by new methods such as electromechanical impedance (EMI) of a piezoelectric torsional transducer.
Keywords: Synovial fluids; Arthritis; Synovial Aging and Gender; Synovial measurement; Piezo sensor; Joints lubricants
Introduction
Arthritis is one of the major health problems that the world face. US center for diseases prevention and control predicts that there will be more than 67 million arthritic patients by 2030 [1]. Arthritis is an inflammation in one or more of the body joints. Its chief symptoms are pain and stiffness in the affected area. The disease tends to manifest itself mostly older people and requires specific remedies to control its spread. The accompanying pain in knee joints occurs due to stiffening joint fluids which are known as synovial fluids. Its kinematics identifies the compressive load and articular cartilage characteristics. For human beings and animals, the derived markers of synovial fluid are commonly referenced in patients suffering from joint diseases, the most common of which are rheumatoid arthritis and osteoarthritis. By closely tracking a single index joint through scrutiny of joint fluid volume, the total biomarker in the joint can be arrived at easily [2].
To arrive at such estimations of the total volume of synovial fluid, there are certain common tests such as blood work, pathology, pertinent radiology tests such as X-rays and MRIs as well as ultrasound, CT scans and the synovial fluid check. In instances where the patient is at an early stage of the disease, a basic blood test and x-ray may suffice. However, those suffering from an advanced form of the issue require more rigorous tests, such as MRI, synovial fluid test or even an ultrasound of the affected area [3]. It needs to be noted that the standard viscometers that are used in laboratories for testing are often bulky, expensive machinery that are prone to non-continuous measurement. Moreover, the fluid is manually drawn from the joint and remains incompatible with the actual environment [4]. This means that such synovial fluid tests are never 100% foolproof [5]. So, what may be the alternative, and more viable, solution? The most encouraging possibility is offered by resonant sensors such as thickness-shear mode (TSM) and the piezoelectric cantilevers. As well, nowadays the usage of the electromechanical impedance (EMI) method has become quite common to particular structural health monitoring (SHM) [6].
This paper highlights synovial fluid properties and explores the lubrication mechanisms of synovial fluid for age-related changes while accounting for gender differences. Further, this paper reviews extant studies that were conducted on automated detection based on deep learning and acoustic monitoring of joint health and response to measurement by new methods such as electromechanical impedance (EMI) of a piezoelectric torsional transducer.
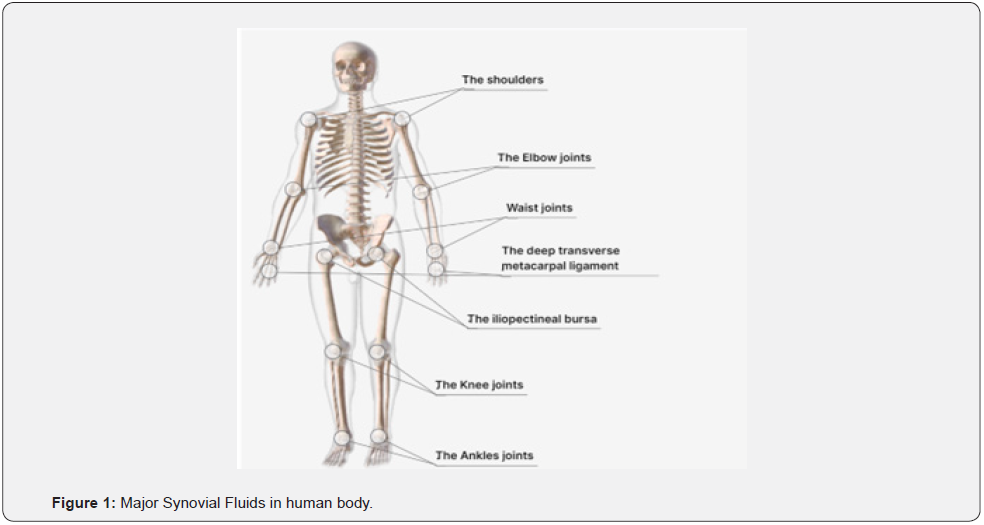
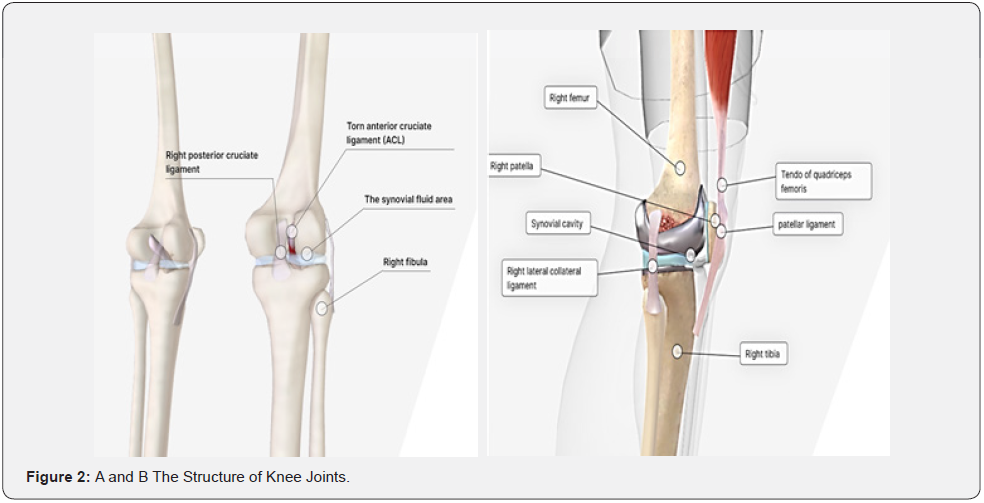
Synovial Fluid Analysis
The term synovia is a reference to its similarity with the white part of eggs [7]. Synovial fluid may be elucidated as the collection of fluid that remains constricted to particular joint spaces. It is an ultrafiltrate of blood plasma and comprises mainly of hyaluronan, lubricin, proteinase, collagenases, and prostaglandins. Such fluid is physiologic, working as a joint space lubricator of articular cartilage. It also diffuses requisite nutrients to its neighboring structures such as cartilage, meniscus and labrum [6]. Synovial fluid resides in different parts of the human body such as knees, waist joint, ankle joints, shoulder joints, hip joints, and other small joints. Figure 1 highlights the presence of the fluid in the human body. Articular cartilage contains an inner liner membrane known as a synovial membrane, which is responsible for the production of synovial fluid for the joints. The synovial membrane contains micro folds that manage inner articular pressure and joint movements [1]. Since the synovial fluid surrounds joints and lubricates them, its analysis detects the source of joint pain and swelling. The working of the knee joint system is tested through its synovial fluid properties [8]. Synovial fluid presence in the joints was first investigated by the Greek Hippocratic text, “Of the Places of Man”. A Roman physician also provides an earlier reference to synovial fluid in his text, “On the functions of parts of the human body”. The estimated quantity of synovial fluid in knee joints varies from 0.5 to 2 ml. [1]. Figure 2 showcases presence of synovial fluid in the knee.
In their research paper, Prekasan & Saju [1] explained that synovial fluid is composed of hyaluronic acid and is identical to blood plasma with 2% protein content. It is utilized for the natural lubrication of elbow and knee joints. It contains surfaceactive phospholipids, proteoglycan 4, and hyaluronic acid. Chondrocytes secreted in these lubricants are synoviocytes and articular cartilage. Synovial spaces in the joints are responsible for the concentration of synovial fluid. Lubricating system deficiencies contribute to the erosion of articular cartilage which creates arthritic conditions. The molecular concentration of hyaluronic acid is 1-4 mg/ml, proteoglycan is 0.05-0.35 mg/ml, and active phosphor lipids is 0.1 mg/ml. Synovial fluid interacts with the joint surfaces in relative motion to reduce friction effects during joint movements.
Synovial fluid plays a diagnostic role in the detection of potential causes of joint pain. Specific conditions that are recognized for the use of synovial fluid include septic arthritis, joint bleeding, autoimmune disorder, and pseudogout. The testing process comprises three categories - microscopic assessment, gross assessment, and chemical analysis. Changes in synovial fluid concentration in the joints leads to joint pain, bleeding, and infectious diseases [8].
Seidman & Limaiem [6] asserted that during synovial fluid gross assessment, doctors examine viscosity level, clarity, volume, and color of the fluid. This helps identify symptoms that cause infection in the joints. During chemical testing of synovial fluid, experts examine the concentration of uric acid in joints. This is done via glucose testing, protein testing, and lactose quantity tests that may explain the reason for joint infection and other health diseases in patients. The microscopic testing of synovial fluid is supported by crystal examination of infection-causing elements. During microscopic testing, doctors examine bacterial culture that have accumulated in the joints by testing individual immune systems (WBCs). Gram stain is also calculated and is used to identify the causes of infections, factors resulting in synovial fluid changes in the body as well as treatment required.
Research Focused on Synovial Fluids and Joint Health
The issue of knee health problems is critical to specialists and medical researchers. There is much ongoing investigation in knee health being conducted by researchers who work in the electric field. They focus on electrical devices that measure and determine the level of knee health, especially synovial fluids and joint health. Human beings are exposed to varying loads on their joints while moving, especially their knee joints. Such loads on joints contributes to tissue damage due to the development of degenerated medical conditions and cartilage damage [9]. These conditions are known as osteoarthritis (OA). Spain & Cheneler [9] studied the acoustic monitoring of joint health. The researchers identified the classification methods that demonstrate the severity of knee damage. Lawrence and Kellgren’s system identified radiographic evidence of OA concentration and scaled it from 0 to 4. However, the information obtained through radiographic evidence is not enough to define cartilage damage since this method had low inter-observer precision. The researchers also viewed other methods that quantify OA development effectively, including radiation-free methods and non-invasive ones. They defined the clinical settings and developed different therapies that would be effective in limiting and reducing OA. Variation of knee sounds during loading conditions and movements are an indicator of structural changes in knee joints and are linked with OA. The researchers also viewed the vibroarthrography and acoustic emission from knee joints. Monitoring the knee joints for OA enabled the researchers to demonstrate synovial fluid needs for joints.
On the other hand, Morea et al. [7] reviewed the rheological properties of synovial fluid and explained OA remedy options. They discussed the lubricative properties of synovial fluid and related it with an electrolytic solution that assists the joints in proper movement. They identified the interaction between the different components of synovial fluid and connected this to the complex rheological properties of the fluid. Their analysis of inflammatory rheumatoid and osteoarthritis diseases demonstrated the significant efficiency of synovial fluid and its lubrication capabilities. They argued that viscosupplementation cases replenish the synovial fluid concentration, affect its molecular weight, and rheological properties of the fluid. They also revised the rheological properties and polymetric properties of synovial fluid and noted the challenges related to its clinical effectiveness and viscosupplements. The rheological properties of synovial fluid detail the viscosity of fluid that is critical in lubricating joint tissues for proper movement.
Mairan et al. [10] explored the mechanism of synovial fluid for joint longevity. It has already been noted multiple times in this paper that the fundamental function of synovial fluid is to lubricate the joints. The constituents of synovial fluid include active phospholipids, hyaluronic acid, and surface-active protein. Mairan et al. [10] also identified its other protein components such as gamma globulin seric protein and human serum protein which assist the synovial fluid in lubricating joints. They identified the bio tribological system of synovial fluid and reviewed the current knowledge of lubrication. The prospective usage of synovial fluid enabled the researchers to identify its ability to combat osteoarthritic. The major focus of their research was to identify the role of protein on prosthetic lubrication, physical variable effects in prosthetic lubrication, and optimal material combination for prosthetics. They tested the wear mechanism of synovial fluid to identify prosthetic lubrication characteristics. Synovial fluid was studied under bio tribology conditions to identify certain prosthetic components and also discuss superior lubrication properties of the fluid. It lubricated the knee and elbow joints and prevented uric acid accumulation in the joints. The prosthetic testing of synovial fluids demonstrated the exact chemical composition of different components and their lubrication mechanism for the development of an effective lubricative mechanism.
Liao et al. [11] evaluated pathological changes in the fluid to develop a numerical understanding in their research. They investigated the roughness of cartilage surface to understand synovial fluid characteristics. The significant focus of the researchers was osteoarthritic conditions of synovial fluid and cartilage contact gap. Initially, they evaluated the cartilage surface topography in healthy as well as osteoarthritic conditions. They developed connections between the healthy and sick stages through a numerical approach with consideration of horizontal and vertical roughness of cartilage surface. Calibration against existing experimental data about the synovial fluid provided constitutive equations for the viscosity of synovial fluid. The results showed cartilage surface reduced its gap permeability by around 30-60%. They tested the gap permeability for discrete cartilage surface sizes. The testing process resulted in the gap permeability of different cartilage surfaces decreasing and becoming more significant. Gap permeability resulted from early fluid ultrafiltration into joint tissues. The gap permeability of the cartilage surface was highly affected by pathological synovial fluid. OA cartilage surface increased the size of gap permeability up to a few hundred times. The pressure gradient remained always less than 106 Pa/m which resulted in fluid ultrafiltration in the tissues. The function of articular joints was highly affected by a change in OA conditions and cartilage contact gaps.
Age-related Changes and Gender Differences in Synovial Fluids
As the human body ages, it affects changes in the level of growth in varied stages and different places of the body. The term aging denotes the various physiological transformations bodies go through from adulthood till death. The bones in the body are remodeled throughout life as older bone tissues are replaced by newer ones. This systematized remodeling ensures a balance between bone resorption and formation which, in turn, maintains skeletal integrity. Like most things, such balance also alters as people age [12]. It needs to be enumerated here that bones are not in direct contact with each other within joints. Indeed, the articular cartilage that lines joints have a cushioning effect. The joints are also protected by synovial membranes while the synovial fluid acts as the lubricant to ensure seamless movement of the joints. However, the synovial fluid reduces as people age, the cartilages thin out – resulting in stiffness around the joints which causes them to stiffen, adding to the woe, ligaments become shorter with age and lose flexibility which also causes the joints to feel stiff [13].
It may be reasonably expected that when these shifts occur, they result often in biological function decline, causing corresponding mental changes such as psychological and behavioral ones. Sometimes, such transformation is evident, while at other times, these may not be clearly perceivable. As bones age, their mineral content also starts depleting. This makes people susceptible to osteoporosis, wherein bones lose density, become more fragile and, thus, likely to suffer from fractures. As human beings age, bone resorption rate by osteoclast cells becomes greater than the speed at which bone forms. Since the aforementioned multinucleated cells comprise mitochondria and lysosomes that aid in bone resorption, bones weaken as the process reverses [12].
With all these references to synovial fluid in this paper, it is necessary at this point to expound on the crucial role this plays in joint health. It has already been noted that this fluid lubricates joints to ensure smooth movement. Further, healthy joints have greater quantities of high molar mass hyaluronic acid (HA) molecules within the synovial fluid which ensures perfect viscosity in its role as a lubricant. As people grow older, the size of HA molecules declines, causing its function ability as a cushioning support and lubricant to lessen [8,14].
Uesaka et al. [15] investigated sex differences and age-related changes in HA and chondroitin sulfate (CS) isomer in regular synovial fluid. This research yielded the result that older people and gender profoundly affected the knee joint tissues, resulting in osteoarthritis. They determined HA and CS isomer levels in normal synovial fluid to test the influence of age and sex on its concentration. They tested a sample population comprising healthy subjects of different ages that informed data on the influence of age on knee joints lubricants’ concentration. The 187 healthy volunteers tested ranged in age between 14 and 89. The results of the study showed that most synovial fluid components had a negative correlation with the age factor. There were no sexrelated differences in synovial fluid concentration. However, CS isomer in the normal synovial fluid was significantly affected by sex-related differences. The affected concentration also varied among women and men.
Temple-Wong et al. [16], in their study, analyzed size distribution and hyaluronan concentration in human knee synovial fluid. They identified synovial fluid variations with cartilage degeneration and age factors. The potential criteria identified in cartilage wear for normal knee joints was an alternative to synovial fluid quantity and lubricant content. They made specific correlations between synovial fluid and age factor. They analyzed the synovial fluid of donors (age range 23–91 years) who were not suffering from osteoarthritis. The researchers also investigated the healthy communities to identify molecular weight of synovial fluid hyaluronan and protein components. Concentration was checked for both left and right knees of the people sampled. Bland-Altman and T-test were implemented to test the synovial fluid concentration. Regression analysis was then performed to define the relationship between each biochemical component. The results highlighted that at older ages cartilage wear is related to the quality of synovial fluid and hyaluronan content of joints. The study authors identified the concentration of all biochemical components of synovial fluid. Healthy joints contain a protein concentration range of 2.5–7 MDa (–9.4 %/decade), 1–2.5 MDa (–11.3 %/decade), 0.5–1 MDa (–12.5 %/decade), and 0.03– 0.5 MDa (–13.0 %/decade). They concluded that hyaluronan concentration was more strongly related to age than joint grade.
Measuring the Viscosity of Synovial Fluids
In order to monitor the health of fluid in human beings, measurement is very important. The reason for synovial fluid measurement is to expostulate explanations for joint pain and dysfunction. Assessing synovial fluid can help doctors reduce or analyze one of the many causes of joint pain. There are many traditional methods to measure synovial fluid such as blood test, pathology, X-ray, MRI, ultrasound, and CT [3]. However, certain medical studies have propounded discrete new methods to measure synovial fluid.
Wang & Li [4] designed an online viscosity measurement method that is based on piezoelectric torsional transducer and electrochemical impedance. The test of the ring array of piezoelectric patches share mode and actuated the diagnostic system according to torsional resonance. They developed quantitative EMI-based measurement equivalence that assists online viscosity measurements, and derived viscous damping through fluid contact and tracking piezoelectric impedance of synovial fluid. They also tested the viscosity of glycerol-water which is a concentrated solution of various components. The results of viscosity measurements agree well with those given by standard laboratory viscometers. The device was highly sensitive toward viscous materials and had high-quality features to measure viscosity of any material. These methods of EMI-based measurement impedance are highly effective and valuable in measuring viscosity of any fluid.
Krishnan et al. [3] stated that by measuring the variation in density of synovial fluid, arthritis can be diagnosed. In their research, the authors used electrical bio-impedance, which is a non-invasive way to measure density of synovial fluid. This was done by calculating the opposition a tissue gives when an electric signal is applied to it. The values were thus recorded as drops in voltage in the area surrounding the joint tissue; it was by nature a resistance and capacitive reactance. The resultant numbers would differ from a normal person to someone suffering from arthritis since a fixed frequency and voltage is applied to the joints. Certain hardware was necessary to execute signal generator circuit compatible with variable frequency and voltage. Since the procedure was non-invasive, voltage drop was calculated by placing four electrodes that record signals and responses. The results showed resistance and reactance varied from normal person to an arthritis-afflicted patient when administered the same fixed frequency and amount of voltage. When such input voltage or frequency was changed, the corresponding measured voltage drop as calculated in bio-impedance also changed.
On their part, Iqbal et al. [17] researched automated detection of human knee joint synovial fluid. They analyzed the magnetic resonance image and developed deep learning-based automated detections with transfer learning. Deep learning is beneficial in understanding analytical tools that help diagnostic teams evaluate synovial fluid concentration in knees more closely. Analytical tools in radiology and medicine provide labeled diseases in detail and reduce ensuing medical field challenges. Transfer learning makes the knowledge process easier, focusing on the needs of relevant diseases, locating accurate solutions with discrete resolution parameters. In the study under reference, transfer learning started from the pre-training stage to move large-scale databases for certain tasks. The researchers tested the synovial fluid concentration in human knees through a deep learning process through magnetic images. They proposed a neutral architecture that specializes in automated detection of fluid through resonance images. This research covered the training, evaluation, and development stages of the proposed model. Independent database structures were utilized to diagnose the fluid level. The experimental model of testing was highly sensitive and specific to synovial fluid evaluation. It was specifically designed to bring accuracy to the experiments and make significant perceptions about testing the fluid level. The proposed structure provided a feasible way for expediting and automating synovial fluid analysis. The annotated database of the research comprised small tunes that comprehensively transferred the understanding of synovial fluid with magnetic resonance images. These images detailed the disease’s causes and made the treatment process easier.
Jun Fu et al. [5] performed the viscosity test of synovial fluid to diagnose periprosthetic joint infection (PJI). The main purpose of this research was to identify an accurate testing methodology that provides authentic results for PJI testing. The researchers examined 45 patients suffering from PJI - PJI (n 1⁄4 15), revision for aseptic failure (n 1⁄4 15), and primary arthroplasty (n 1⁄4 15). The researchers argued synovial fluid viscosity varies in patients with periprosthetic joint infection. They identified the sensitivity of viscosity difference to develop an accurate testing framework. They utilized the musculoskeletal infection criteria to identify the viscosity level of synovial fluid. They also measured the plasma D-dimer level, c-reactive protein, and erythrocyte sedimentation rate of each patient. The result indicated synovial fluid viscosity level was 0.0011, which was significantly lower in patients with PJI as opposed to those with no such infection. Synovial fluid viscosity level exceeded on CRP, ESR, and plasma D-dimer, with a sensitivity of 93.33% and specificity of 66.67%.
Conclusion
From the perusal of extant research and our derived understanding of the same, this paper offers certain solutions to issues concerning synovial fluid. The basic role of synovial fluid is to lubricate joints. It consists of powerful phospholipids, hyaluronic acid, and surfactant protein. Assessing provocative rheumatoid and osteoarthritis conditions shows the critical presence of synovial fluid and its lubricating abilities for joints. Viscos supplementation events round out the synovial fluid focus, affecting its atomic weight and the rheological properties of the fluid. Such properties of synovial fluid are demonstrated by its thickness; however, there was no known procedure to analyze the consistency phase of synovial fluid. It has been established that imbalances in this intracellular fluid causes many health problems, and its considerations are disturbed inside the joint. Each joint in the casing is combined with synovial fluid as a guide for joint oil. As well, this synovial fluid is called synovial lamina because it resembles proteins. The primary task of this fluid is to lubricate joints and allow for additional linear motion. Such lubrication helps ensure smooth movement and less stress on the joints. Age has a significant effect on the volume of synovial fluid in the body. This research concludes that there are different new methods to measure volume of synovial fluids. One such method discussed was Piezoelectric which is characterized by miniaturization, use of small power, self-excitation, and selfdiscovery qualities. The other process enumerated in this paper is the electrical bio-impedance concept, wherein synovial fluid measures are taken to accord fast results that can ensure quality care to patients suffering from joint mobility issues.
References
- D Prekasan, K K Saju (2016) Review of the Tribological Characteristics of Synovial Fluid. Procedia Technology 25: 1170–1174.
- T Stabler, J Kong, G Varju, G McDanie, V B Kraus (2006) P79 Measurement of Synovial Fluid Volume Using Urea. Osteoarthritis and Cartilage 14: S54–S55.
- G H Krishnan, A Nanda, A Natarajan R (2014) Synovial Fluid Density Measurement for Diagnosis of Arthritis. Biomedical & Pharmacology Journal 7(1): 221–224.
- G Wang, F Li (2018) An Online Viscosity Measurement Method Based on the Electromechanical Impedance of a Piezoelectric Torsional Transducer. IEEE Sensors Journal 18(21): 8781–8788.
- J Fu, M Ni, W Chai, X Li, L Hao, et al. (2019) Synovial Fluid Viscosity Test is Promising for the Diagnosis of Periprosthetic Joint Infection. J Arthroplasty 34(6): 1197–1200.
- Seidman AJ, Limaiem F (2022) Synovial Fluid Analysis. In: StatPearls [Internet]. Treasure Island StatPearls Publishing, FL, USA.
- S More, A Kotiya, A Kotia, S K Ghosh, LA Spyrou, et al. (2020) Rheological properties of synovial fluid due to viscosupplements: A review for osteoarthritis remedy. Computer Methods and Programs in Biomedicine 196: 105644.
- Walker W (2022) Effects of Ageing on Joints.
- A Watson Anatomy Knee Joint | Anatomy. Geeky Medics.
- Spain L, Cheneler D (2020) Acoustic monitoring of joint health”. InData Acquisition-Recent Advances and Applications in Biomedical Engineering IntechOpen.
- M Marian, Raj Shah, Blerim Gashi, Stanley Zhang, Kiran bhavnani, et al. (2021) Exploring the lubrication mechanisms of synovial fluids for joint longevity – A perspective,” Colloids and Surfaces B: Biointerfaces 206: 111926.
- J Liao, S Miramini, X Liu, L Zhang (2020) Computational study on synovial fluid flow behaviour in cartilage contact gap under osteoarthritic condition. Computers in Biology and Medicine 123: 103915.
- Abdullzaher, et al. (2020) Effects Ageing on Bone.
- Better Health Channel (2012) Home. Vic.gov.au.
- S Uesaka, K Miyazaki, H Ito (2004) Age-related changes and sex differences in chondroitin sulfate isomers and hyaluronic acid in normal synovial fluid. Mod Rheumatol 14(6): 470–475.
- M M Temple-Wong, Shuwen Ren, Phu Quach, Bradley C Hansen, Albert C Chen, et al. (2016) Hyaluronan concentration and size distribution in human knee synovial fluid: variations with age and cartilage degeneration. Arthritis Res Ther 8(1).
- I Iqbal, G Shahzad, N Rafiq, G Mustafa, Jinwen ma (2019) Deep learning based automated detection of human knee joint’s synovial fluid from magnetic resonance images with transfer learning. IET Image Processing 14(10): 1990-1998.






























