Outcome of PRP Therapy in Rheumatoid Arthritis - An Analysis Done in a Tertiary Care Hospital
K Satya Kumar1*, Vamsi Krishna V2, Harsha M3, Sravya L2 and A Kaushik4
1Department Of Orthopedics, NRI Academy of Sciences, India
2Assistant Professor, Department of Orthopaedics, NRI Academy of Sciences, India
3Senior resident, Department of Orthopaedics, NRI Academy of Sciences, India
4Junior Resident, Department of Orthopaedics, NRI Academy of Sciences, India
Submission: January 03, 2022; Published: January 18, 2022
*Corresponding author: Dr K Satya Kumar Prof & Head, Department of Orthopaedics, NRI Academy of Sciences, Andhra Pradesh, India
How to cite this article: K Satya Kumar, Vamsi Krishna V, Harsha M, Sravya L, Kaushik. Outcome Of PRP Therapy in Rheumatoid Arthritis - An Analysis Done in a Tertiary Care Hospital. Ortho & Rheum Open Access J. 2022; 19(4): 556019. DOI: 10.19080/OROAJ.2022.19.556019
Abstract
Introduction:Among Rheumatoid Arthritis Patients (RA), general disease activity is well regulated by disease-modifying Anti-Rheumatic Medications (DMARDs), but sometimes local inflammation persists among a few joints. Adjuvant modern molecular interventions as Platelet Rich Plasma (PRP) with a suggested down regulating effect on inflammatory mediators has a proven effect in the management of RA.
Aim: To Evaluate the outcome of PRP therapy in Rheumatoid Arthritis especially in pain control & disease progression
Methodology: Total 34 cases were analyzed after treatment with autologous Platelet Rich Plasma Injections. All the cases were given 3 to 5 cc of PRP depending on the area of involvement. Total duration of treatment depended on the number of injections. One injection once in 2 weeks was the protocol followed. Analyzed at 6 weeks, 12 weeks and 24 weeks after the final PRP Injection. Final analysis to know the outcome was done at the end of 1 year after final PRP therapy to avail the results. Hematological, radiological evidence of arthritis was made prior to treatment. Outcome analysis was done for the reduction in pain, decrease in stiffness, and improvement in physical function using the WOMAC Scale. The patients were also assessed for reduction in pain using visual analog scale.
Results: Over all 26 out of 34 cases had satisfactory to good results with platelet rich plasma therapy for more than 14 months which encouraged us to take up this treatment as one more option along with medical management.
Conclusion: PRP can be a safe and effective treatment in patients with RA who failed to respond to conventional treatment options with progression of disease.
Introduction
Rheumatoid Arthritis (RA) is a chronic inflammatory joint disease that involves damage to the cartilage. RA shares features such as cartilage matrix degradation and progressive joint remodeling with osteoarthritis (OA), while OA joints exhibit predominant inflammation. This suggests a shared underlying pathology in RA and OA [1]. Several cytokines, chemokines, proteases, cell adhesion molecules, and angiogenic factors are common in the pathological processes in RA and OA [2]. Macrophages and macrophage-derived growth factors such as Vascular Endothelial Growth Factor (VEGF) are increased in the inflamed synovium of both RA and OA joints [2,3]. Active angiogenesis is evident in the synovium of affected joints in both RA and OA [3,4], and the redistribution of blood vessels in the synovial tissues may compromise cartilage metabolism and exacerbate chondropathy. RA may often coexist with OA.
Response to therapies differs in RA and OA. Though nonsteroidal anti-inflammatory drugs (NSAIDS), analgesics, and steroids are used in both conditions, biological agents such as Anti Tumor Necrosis Factor (anti-TNF) therapies more convincingly reduce inflammation and angiogenesis in RA than in OA [2]. Biologic Disease-Modifying Anti Rheumatic Drugs (BDMARDS) that target key immunological components of disease pathology have transformed the management of RA. However, clinical and immunological response to BDMARDS is variable and inconsistent [5]. There remains an ongoing quest for therapies that target articular inflammation and inhibit synovial angiogenesis and prevent damage to healthy cartilage. Platelet-Rich Plasma (PRP) is an autologous blood sample that has highly concentrated platelets and several cell-growth factors. PRP may help to restore cartilage morphology and microarchitecture due to its action on synovial cell proliferation and differentiation and inhibition of inflammatory factors in joints [6–8]. Though PRP has shown good efficacy in OA and other musculoskeletal conditions such as epicondylitis and tendinopathy [9–12], there is limited experience for the use of PRP in patients with RA. Our study is aimed at evaluating the outcome of PRP therapy in Rheumatoid Arthritis.
Materials and Methodology
Inclusion Criteria
Seropositive & Seronegative Rheumatoid Arthritis not involving more than 4 Joints.
Exclusion Criteria
Previous Steroid/ LA Injections. More than 4 joints involvement. Skin lesions around the joint.
Uncontrolled diabetic patients. Infection elsewhere in the body.
Methodology
Total 34 cases of which, 16 knees, 6 wrists, 4 elbows, 2 ankles, 6 shoulders were analyzed after treatment with autologous platelet rich plasma injections. Analyzed at 6 weeks, 12 weeks & 24 weeks after the final PRP injection. Final analysis to know the outcome was done at the end of 1 year after final PRP therapy to avail the results.
Hematological, radiological evidence of arthritis was made prior to treatment. Prior CBP, RBS, ESR & CRP were advised to all the patients. Platelet more than 200,000 were selected, random blood sugar below 180 & hemoglobin above 10gm% were selected. If elevated ESR & CRP were the findings, we have postponed the therapy. If ESR is more than 30 & CRP more than 0.6 with elevated polymorphs were assessed for the route cause & treated the condition which caused elevation & then took up for therapy. All the cases were given 3 to 5 cc of PRP depending on the area of involvement. Total duration of treatment depended on the number of injections. One injection once in 2 weeks was the protocol followed. For all the knee joints 3 PRP injections were given. For remaining areas 2 PRP injections were given. Rehabilitation protocol was advised for 2-3 weeks after final injection of PRP physical therapy was mainly in the form of exercise therapy, no machines were used. No NSAIDS were used. Patients were given paracetamol 1gm on SOS basis for the pain relief.
Results
14 out of 16 knees had good pain relief for 18 months. 6 out of 6 shoulder cases had good relief of pain for 14 months. 1 out of 2 ankle joints had good relief of pain for 16 months. 4 out of 6 wrists had very good pain relief for 20 months. 1 elbow case had satisfactory outcome for 20 months. 2 knees, 2 wrists & 1 ankle cases didn’t obtain relief of pain with the designed protocol. So, we had to repeat the treatment and final result was not satisfactory at all. Over all 26 out of 34 cases had satisfactory to good results with platelet rich plasma therapy for more than 14 months which encouraged us to take up this treatment as one more option along with medical management.
Outcome Analysis
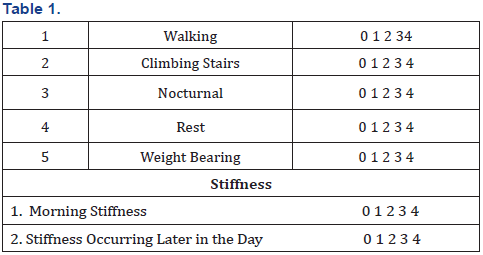
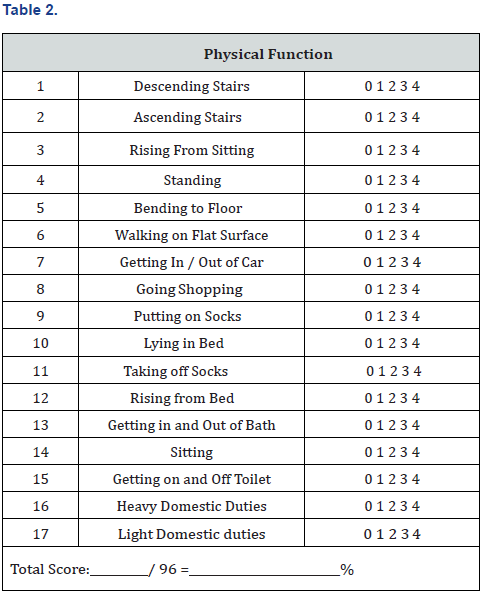
The patients were advised to follow up at 6 weeks, 12 weeks & 24 weeks. Outcome analysis was done for the reduction in pain, decrease in stiffness, and improvement in physical function using the WOMAC scale. The patients were also assessed for reduction in pain using visual analog scale.
WOMAC (Western Ontario and McMaster Universities)Index of Osteoarthritis 5, 17
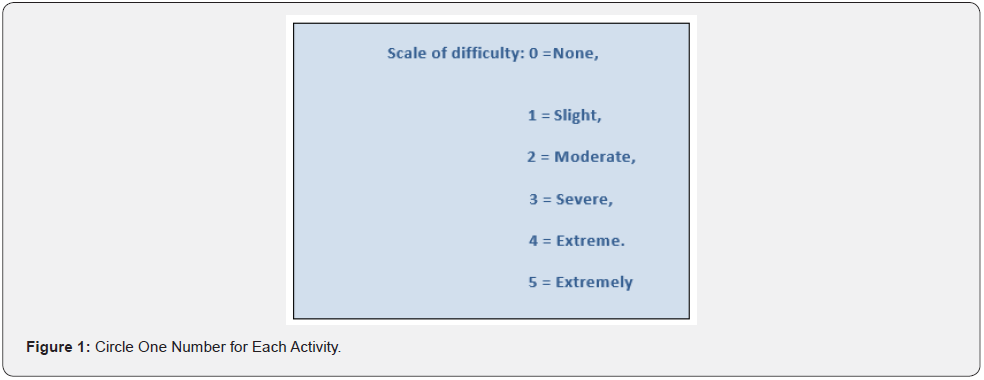
The WOMAC index is used to assess patients with osteoarthrosis of the hip or knee using 24 parameters. It can be used to monitor the course of the disease or to determine the effectiveness of therapy (Figures 1 & 2) (Tables 1 & 2).
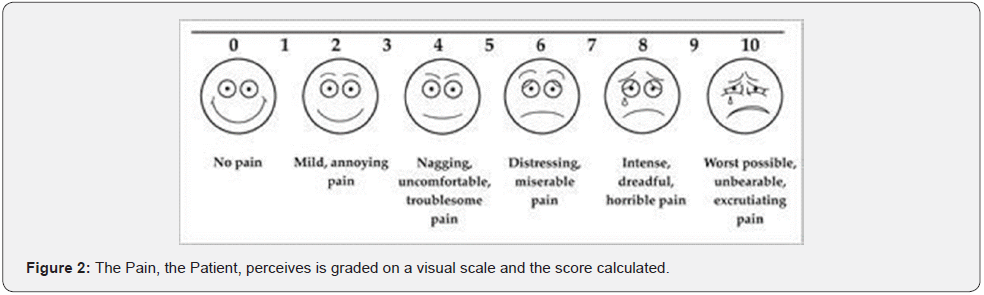
Visual Analog Scale for Pain
The pain, the patient, perceives is graded on a visual scale and the score calculated.
Discussion
The use of biological agents, including PRP and mesenchymal stem cells (MSCS) in orthopedics, has increased exponentially over the last few years due to its autologous nature, lack of side-effects, and supposed effectiveness. Platelet-rich plasma is an autologous blood product with platelet concentrations above baseline. Tissue repair is a complex process comprising chemotaxis, angiogenesis, cell proliferation, and matrix formation. Platelets are involved in all these functions by the release of growth factors.
High concentrations of proteins such as Platelet-Derived Growth Factor (PDGF), Vascular Endothelial Growth factor (VEGF), endothelial cell growth factor, and the fibroblast growth factor have led to suggestions that PRP may be useful in conditions requiring tissue healing. Conversely, the other protein in PRP, Transforming Growth Factor (TGF-b1), has an inhibitory effect and can lead to non-predictable results.
Preparation of PRP can result in four products:
i i.Pure PRP (p-PRP) with a low content of leucocytes. This can be injected as a liquid or a gel.
ii ii. Leucocyte-rich PRP (l-PRP) has a higher concentration of platelets than p- PRP. Similarly, to p-PRP, it can be used as an activated gel or in a liquid form to be injected intra-articular.
iii iii. Pure Platelet-Rich Fibrin (p-PRF). This is obtained by double-spinning centrifugation without adding anticoagulants. The product is a platelet-rich fibrin scaffold, which is stiffer than the conventional PRP and takes the form of a gel and can be used for the healing of wounds.
iv Leucocyte- and Platelet-Rich Fibrin (l-PRF), which is a leucocyte-rich gel which is non-injectable and is applied locally. platelets are regarded as the primary mediators of hemostasis. they contain alpha granules enriched with growth factors. platelets also have anti-bacterial and fungicidal agents, which provoke the synthesis of interleukins and chemokines. when platelets get activated, this causes the release of growth factors. among them, important ones include Transforming Growth Factor-Beta family (TGF-beta1), Platelet- Derived Growth Factor (PDGF), Insulin-like Growth Factor (IGF), and Fibroblast Growth Factor (FGF), etc. in the presence of calcium chloride, the platelet concentrate is activated, which causes the release of these growth factors, eventually promoting healing.
PRP has also been found to have anti-inflammatory actions. The inflammatory cascade generated by cyclooxygenase family can be inhibited by anti-inflammatory mediators present in PRP. PRP has an influence on all structures of joint. Chemotactic assays have revealed that the PRP stimulated the differentiation of typeii collagen cells and the production of prostaglandins along with the migration of cortico spongious bone cells.
We, in our study, had 34 cases with classic findings of RA. They were comparable to baseline characteristics of age, weight, and pre-injection, and post- injection WOMAC score. All the patients received intraarticular injections. The efficacy of platelet rich plasma (PRP) in decreasing pain, stiffness, physical function was assessed and scored on the WOMAC index. Age distribution revealed a mean age in to be 49.92. Gender distributions were comparable in both groups, with 66.6 % being female 33.3% being male. Thus, the study of platelet-rich plasma ensured that all patients were comparable to base.
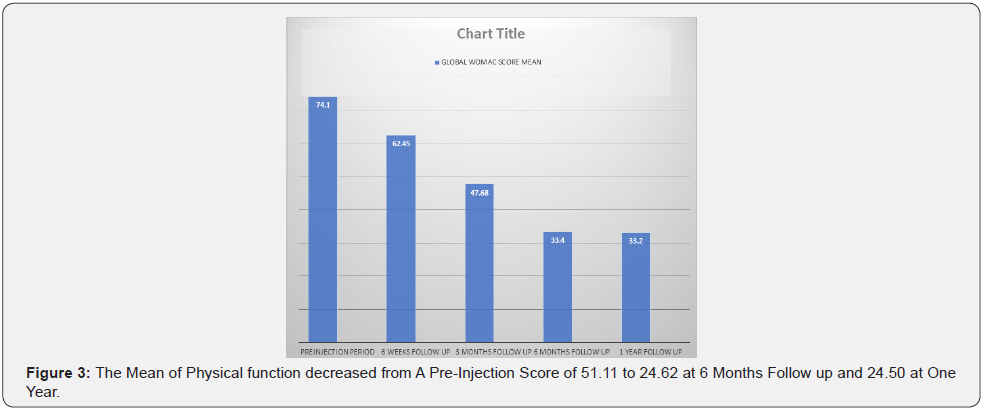
The global WOMAC score showed a mean of 74.1 at the preinjection period, which decreased to 62.45 at 6 weeks follow up and 47.68 at 3 months and declining to 33.40 at 6 months and 33.20 at one year (Figure 3). Individual variables such as pain, physical function, etc. Were assessed. The mean score for pain showed a decrease from 16.57 to 11.31 at 6 weeks post-injection. At the end of 1 year follow up, the mean was 5.34. The mean of physical function decreased from a pre-injection score of 51.11 to 24.62 at 6 months follow up and 24.50 at one year (Figure 3).
Conclusion
The epidemic of modernization, along with adequate health care delivery, has led to an expanded lifespan of human beings. The focus of health care providers is undergoing a drift towards noncommunicable and degenerative disorders. PRP can be a safe and effective treatment in patients with ra who failed to respond to conventional treatment options with progression of disease. Intra-articular PRP is easier to adopt in patients with ra as this is administered in out- patient department and do not require hospitalization. PRP can evolve as a non-surgical option in patients with ra. However, PRP preparations must be done with caution to avoid any uneventful transmission of infections. PRP should be analyzed in clinical trials for improvement in joint structure and composition and restoration of function and quality of life in patients with ra. Treatment with NSAIDS and steroids have efficacy for pain relief, but these does not influence disease progression. DMARDS gained importance for attenuation of disease progression though long-term remissions have not been adequately achieved in patients with RA. Long-term, well-planned studies are required to confirm if PRP treatment can check progressive disability in RA.
References
- T Pap, A Korb-Pap (2015) Cartilage damage in osteoarthritis and rheumatoid arthritis-two unequal siblings. Nature Re- views Rheumatology 11(10): 606–615.
- I MacDonald, S C Liu, C M Su, Y H Wang, C H Tsai, et al. (2018) Implications of angiogenesis involvement in arthritis. Int J Mol Sci 19(7): 2012.
- A Giatromanolaki, E Sivridis, N Athanassou, E Zois, P E Thorpe, et al. (2001) The angiogenic pathway ‘vascular endothelial growth factor/flk- 1(KDR)-receptor’ in rheumatoid arthritis and osteoarthritis. J Pathol 194(1): 101–108.
- M S Zhao, R H Xia, Y H Wang, L X Ding, L Guan, et al. (2012) Characteristics of vascular morphology and vascular endothelial growth factor in patients with osteoarthritis and rheumatoid arthritis. Beijing Da Xue Xue Bao Yi Xue Ban 44(6): 927–931.
- V C Romao, E M Vital, J E Fonseca, M H Buch (2017) Right drug, right patient, right time: aspiration or future promise for biologics in rheumatoid arthritis? Arthritis Re- search & Therapy 19(1): 239.
- J Chahla, M E Cinque, N S Piuzzi, Sandeep Mannava, Andrew G Geeslin, et al. (2017) A call for standardization in platelet-rich plasma preparation protocols and composition reporting. J Bone Joint Surg Am 99(20): 1769–1779.
- N A Smyth, A M Haleem, K A Ross, Charles P Hannon, Christopher D Murawski, et al. (2016) Platelet-rich plasma may improve osteochondral donor site healing in a rabbit model. Cartilage 7(1): 104–111.
- W D Murrell, A W Anz, H Badsha, W F Bennett, R E Boykin, et al. (2015) Regenerative treatments to enhance orthopedic surgical outcome. PM & R 7(4): S41–S52.
- B J Cole, V Karas, K Hussey, D B Merkow, K Pilz, et al. (2017) Hyaluronic acid versus platelet-rich plasma: a prospective, double-blind randomized controlled trial com- paring clinical outcomes and effects on intra-articular biology for the treatment of knee osteoarthritis. Am J Sports Med 45(2): 339–346.
- H N Sadabad, M Behzadifar, F Arasteh, M Behzadifar, H R Dehghan, et al. (2016) Efficacy of platelet-rich plasma versus hyaluronic acid for treatment of knee osteoarthritis: a systematic review and meta-analysis. Electronic Physician 8(3): 2115–2122.
- R A Mlynarek, A W Kuhn, A Bedi (2016) Platelet-rich plasma (PRP) in orthopedic sports medicine,” The Am J Orthop (Belle Mead NJ) 45(5): 290–326.
- A K Mishra, N V Skrepnik, S G Edwards, Grant L Jones, Steven Sampson, et al. (2014) Efficacy of platelet-rich plasma for chronic tennis elbow. Am J Sports Med 42(2): 463–471.






























