Radiographic Analysis of Cemented versus Uncemented Humeral Stem of Reverse Total Shoulder Arthroplasty for Proximal Humerus Fractures
Om V Patel1, Alexander C Wendling1, Bradley M Saunders1,2 and Shang-You Yang1*
1Department of Orthopedic Surgery, University of Kansas School of Medicine-Wichita, Wichita KS, United States
2Ascension Via Christi Medical Groups, Wichita, KS, United States
Submission:August 20, 2021; Published:August 30, 2021
*Corresponding author: Shang-You Yang, MD PhD, Department of Orthopedic Surgery, University of Kansas School of Medicine-Wichita, 929 N Saint Francis, Wichita, KS 67214, United States
How to cite this article:Om V Patel, Alexander C Wendling, Bradley M Saunders, Shang-You Yang*. Radiographic Analysis of Cemented versus Uncemented Humeral Stem of Reverse Total Shoulder Arthroplasty for Proximal Humerus Fractures. Ortho & Rheum Open Access J. 2021; 19(1): 556004.DOI: 10.19080/OROAJ.2021.19.556004
Abstract
The aim of this study is to compare radiographic outcomes of cemented and uncemented stem fixation for reverse total shoulder arthroplasties (RTSA) performed in the setting of fracture. A retrospective chart review was performed on 64 shoulders in 63 consecutive patients (mean age 75 years, range 61 to 88) who underwent RTSA for proximal humerus fracture between 2014 and 2017. This series consisted of 28 cemented and 36 uncemented stems with an average radiographic follow up of 12 months (range 3-37 months). Postoperative radiographs were evaluated for lucency, subsidence, scapular notching, and endosteal erosion or sclerosis. The results indicated no statistical significance in radiographic lucency (19% vs 11%) or scapular notching (44% vs 25%) between the uncemented and cemented prostheses. There was no radiographic evidence of subsidence, endosteal erosion, or endosteal sclerosis in any of our subjects. When comparing patients who exhibited lucencies to those without lucencies, a lower body weight (65kg vs 86kg), increased follow up time (13.9 months vs 7.8 months), and scapular notching (90% vs 25%) were significantly associated with developing zones of lucency (p<0.05). In conclusion, there was no difference in radiographic outcomes in patients who underwent uncemented RTSA compared to cemented RTSA for treatment of proximal humerus fractures. Patients with a lower body weight, increased follow up time, and scapular notching are more likely to develop zones of lucency.
Keywords:Reverse total shoulder arthroplasty; Proximal humerus fracture; Bone cement; Stem fixation
Introduction
Proximal humeral fractures account for approximately 5% of fractures seen in the Emergency Department that often pose difficult challenges for the treating physicians [1]. Treatment options include non-operative management, osteosynthesis, hemiarthroplasty, total shoulder arthroplasty and, more recently, reverse shoulder arthroplasty [2]. A study evaluating the outcomes of complex humeral fractures in the elderly resulted in a 51% early failure rate and 26% need for reoperation [3]. Neer was the first to introduce hemiarthroplasty as a treatment alternative for comminuted Neer 3 and 4-part fractures which offered desirable pain relief but varying functional results [4]. Functional outcome seemed to correlate with tuberosity healing (resorption, nonunion, malunion), although tuberosity healing was found to be compromised in 39% to 50% of patients with these fractures [5].
A successful outcome with reverse total shoulder arthroplasty (RTSA) for fracture is far less dependent on tuberosity healing and is thus gaining in popularity. Several studies have demonstrated its utility in severely comminuted, 3 or 4-part proximal humerus fractures in the elderly. For example, George et al. [2] recently concluded that RTSA resulted in improved range of motion and functional outcome scores with no difference in rate of complications as compared to hemiarthroplasty. This was based on a meta-analysis of 5 studies comparing RTSA to hemiarthroplasty for comminuted fractures. Indeed, other investigators also demonstrated similar results with increase in constant scores over a 33- and 22-month period, respectively, for comminuted fractures treated with RTSA [6,7].
Joint registry data indicates that surgeons are moving towards uncemented stems for RTSA although the available literature is insufficient to support this transition [8]. Moreover, the data is non-existent in the context of proximal humerus fracture. It is generally believed that glenohumeral arthroplasty in the setting of fracture is best performed with a cemented humeral component as osseous stability is thought to be compromised. However, this is not clearly shown in any literature. Our primary aim in this study was to retrospectively compare radiographic data of cemented stem fixation vs uncemented stem fixation for reverse total shoulder arthroplasties performed specifically in the setting of fracture in a community orthopaedic practice. By performing an analysis of radiographs, we hope to support our hypothesis that patients undergoing reverse total shoulder arthroplasty as treatment for proximal humerus fractures with a uncemented humeral stem will have similar radiographic success as do reverse total shoulder arthroplasties with cement fixation of the humeral stem. Secondarily, we hope to report on any known complications among these subjects.
Materials and Methods
This retrospective study was approved our institutional IRB. All RTSAs were performed by a single fellowship-trained shoulder surgeon between May 2014 to September 2017 were reviewed in order to isolate those performed for the diagnosis of proximal humerus fracture. We isolated 63 consecutive patients with 64 shoulders. Of these 64 shoulders, 28 shoulders had cemented stems and 36 had uncemented stems as identified by chart review. The decision to use cemented vs uncemented humeral fixation was at the discretion of the surgeon based on fracture pattern and bone quality at the time of surgery. Of note, the surgeon tended to use cemented humeral fixation early in the study period moving to primarily uncemented towards the end of the study period. Clinical records and radiographs were then reviewed on these 63 patients to extract the necessary information.
The inclusion criteria consisted of all primary RTSAs performed as definitive treatment for acute proximal humerus fractures by this surgeon during the indicated time period. In addition, they required immediate post-operative AP shoulder radiograph along with a comparable AP shoulder radiograph at the minimum 3-month follow-up. Exclusion criteria consisted of RTSAs performed for any other reasons including but not limited to cuff tear arthropathy (with or without osteoarthritis), shoulder instability, chronic dislocations, or revision cases.
Operative technique remained similar between the two study groups. A standard delto-pectoral approach was used with a subscapularis release and subsequent repair if not already dissociated by lesser tuberosity fracture. After exposing the fracture, the surgeon then decided whether internal fixation was reasonable based on fracture patterns and available bone stock. If not, a decision was then made to perform a reverse shoulder arthroplasty, total shoulder arthroplasty or hemiarthroplasty. This decision was made based on fracture pattern, bone quality, remaining rotator cuff, preoperative shoulder function, baseline physical functional level, and age. Lastly, the decision for cemented vs uncemented was at the discretion of the surgeon based on available bone stock and quality. The humeral shaft was reamed and broached in a similar fashion in both groups. When cement was used, it was impregnated with tobramycin. The glenosphere was fixated in a standard fashion utilizing the baseplate with 4 screws in the glenoid vault. Before closure, an attempt was made in each case to anatomically reattach tuberosities and/or remaining cuff to either available bone or directly to the implant. However, excision of tuberosity fragments was performed if irreparable. At the completion of the case, vancomycin powder was placed in the deltopectoral interval and a hemovac drain was placed prior to closure. Routine post-operative radiographs were taken to include an AP and lateral of the shoulder.
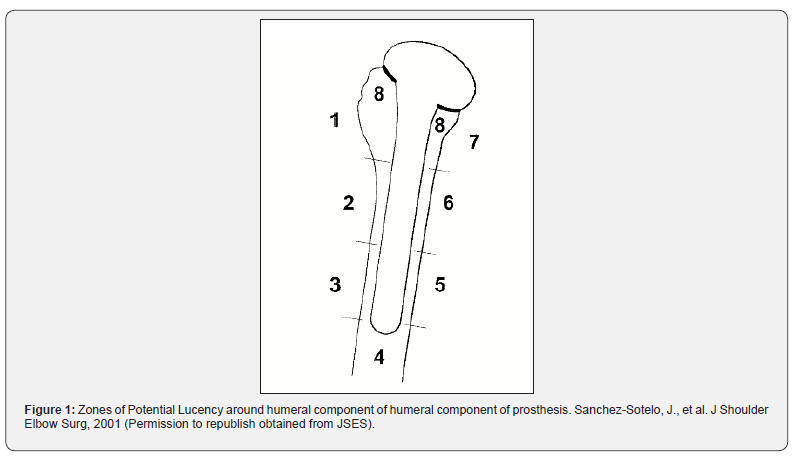
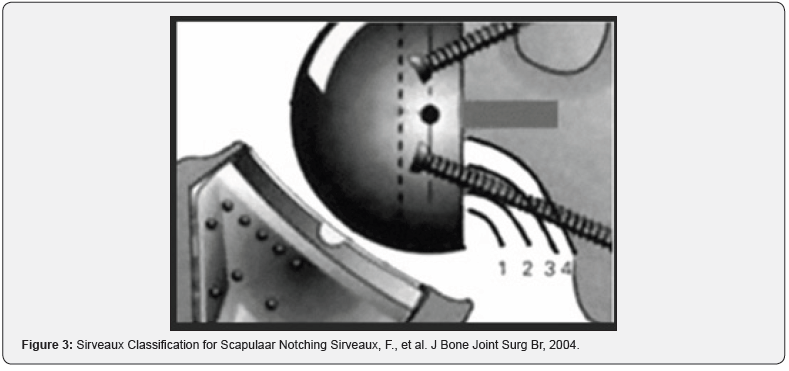
Radiographic analysis of the humeral stem was performed by comparison of immediate post-operative AP radiograph with the latest follow-up imaging available. This analysis was performed by a single examiner to avoid interobserver variability. Radiographic analysis as described by Sanchez-Sotelo, et al was used to evaluate the films for radiolucencies [9,10]. This technique identifies 8 separate zones around the humeral stem with significant lucencies considered to be >2mm (Figure 1). Lucent lines were measured using Synapse’s standard digital measuring tool to within 0.5mm (Figure 2). If lucencies were found in 3 or more zones, the stem was considered “at risk” for clinical loosening [9,10]. We also recorded the presence of subsidence, scapular notching, and endosteal erosion or sclerosis. Subsidence was measured as any change in vertical distance between the superior most margin of the greater tuberosity (or proximal edge of lateral cortex in our fracture scenario) and the superior margin of the implant between images [10]. Scapular notching was classified from 0-4 based on the Sirveaux Classification (Figure 3) [11].

Potential complications were recorded based on chart review included deep infection, superficial skin infection, dislocation, intraoperative fracture, periprosthetic fracture, thromboembolism, post-operative DVT, hematoma, neurologic complications, and complex regional pain syndrome (CRPS) [2,8,12]. Statistical correlations between radiographic changes or implantation type and various patient demographics were assessed by Student’s T test or Fisher’s exact test as determined by the characteristic of the variable being assessed. A significance level of p ≤ 0.05 was used for all comparisons.
Results
Sixty-three (63) consecutive patients with 64 reverse total shoulder arthroplasties were identified as treatment procedures for proximal humerus fracture. Of these 64 shoulders, 28 shoulders had cemented stems and 36 had uncemented stems. The decision to use cemented vs uncemented humeral fixation was at the discretion of the surgeon based on fracture pattern and bone quality at the time of surgery. The surgeon tended to use cemented humeral fixation early in the study period, whereas largely switched to uncemented fixation the end of the study period. Three different RTSA implant companies were used including Tornier (47 shoulders), Integra (5 shoulders), and DonJoy (12 shoulders). The average age was 75 years (range 61- 88 years) and the average time to surgery was 14.5 days (range 1 to 82 days). Greater than 80% of fractures were due to falls. Sixty of the 64 RTSAs (94%) were deemed to be a 3 or 4-part fracture based on the Neer classification system. Minimum follow-up for radiograph review was set at 3 months post-operatively with respect of the average radiographic follow-up at 12 months (range 3-37 months).
There were no differences with regards to age, sex, body mass index (BMI), sidedness of surgery, or time from injury to operative fixation between uncemented and cemented humeral components (Table 1). Notably, the rate of lucency, scapular notching, and proximal bone resorption was not significantly different between uncemented and cemented stems however they did tend be higher in the uncemented group.
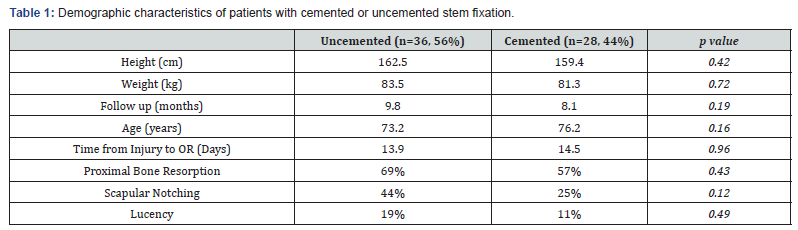
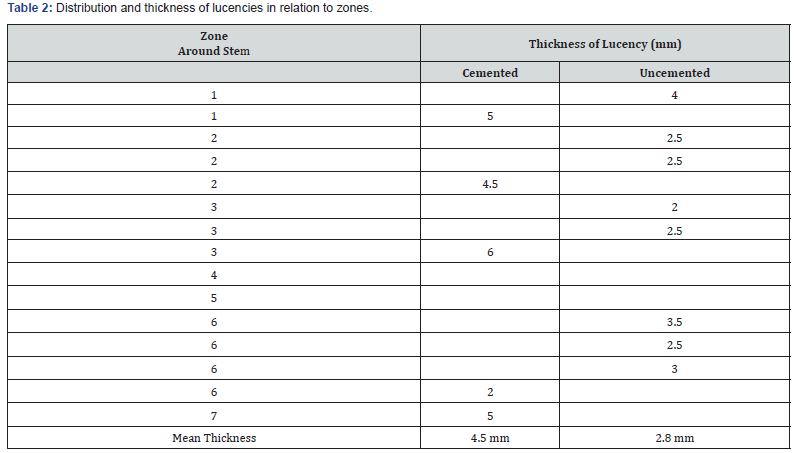
Overall, only 10 of 64 prostheses (15%) had any lucencies at a mean follow up of 12 months. Of these 10 prostheses, 7 were uncemented and 3 were cemented. Radiolucent lines were limited to 1 zone (6 shoulders) and 2 zones (4 shoulders). None of the RTSAs with lucent zones had more than 2 zones of involvement, thus implying that all stems were free from risk of clinical loosening based on the Sanchez-Sotelo technique [12]. The overall mean lucency thickness was found to be 3.4mm (range 2-6mm). The Average thickness was 4.5mm for cemented and 2.8mm for uncemented stems. The 3 most common zones of lucencies in order were zone 2, zone 6, and zone 3 (Table 2).
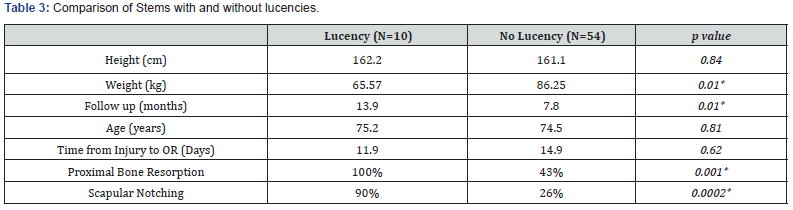
When directly comparing the subset of patients with lucencies vs without lucencies (Table 3), a lower body weight (65 kg vs 86 kg) and increased follow-up time (13.9 months vs 7.8 months) were factors significantly correlated with lucencies (p = 0.01). Scapular notching was seen in 23 of 64 shoulders. Sixteen [7] were grade 1 and the remaining 7 shoulders were grade 2 based on the Sirveaux grading system. Radiographic scapular notching was found to be associated with humeral lucencies (p = 0.0002). Lastly, proximal bone resorption was found more commonly in stems with lucencies than without (100% vs 43%, p = 0.001). Of note, there was no radiographic evidence of diaphyseal endosteal erosion, diaphyseal endosteal sclerosis, or subsidence found in any of our study subjects. Lastly, we did not identify any major complications as a direct result of our surgical intervention based on our available chart review. We also did not identify any patients that necessitated a revision surgery at the time of chart review.
Discussion
The use of uncemented humeral stems as opposed to cemented stems for reverse total shoulder arthroplasty in the setting of Neer 3 or 4-part proximal humerus fractures is becoming more popular, although there is insufficient literature supporting this shift [8]. The clinical significance of an uncemented humeral stem as opposed to a cemented stem is multifaceted. Theoretical advantages include shorter operative time, biologic ingrowth potential, and easier revision of the humeral component [13]. Furthermore, the use of cement has been implicated with thermal nerve injury, increased risk of thromboembolism from cement pressurization, and increase in infection rates due to increased OR time8. However, these potential benefits must be correlated with outcomes and complications.
A systematic review by Phadanis et al. in a meta-analysis reviewed 41 clinical studies including 1,455 cemented and 329 uncemented shoulders. They concluded no significant difference in functional outcomes and a better complication profile associated with uncemented stems. Cemented stems had a greater relative risk of infection, nerve injury, and thromboembolism. On the other hand, the uncemented stem had a higher incidence of early stem migration and non-progressive radiolucent lines [8]. This study provides insight to the benefits of uncemented fixation but also reports the higher incidence of stem radiolucencies and migration. It is also important to mention that this study was comparing RTSAs not in the setting of fracture. Our literature review did not identify any other studies comparing radiographic findings of cemented vs uncemented stems in RTSA performed for proximal humerus fractures.
Our study of 64 reverse shoulder arthroplasties demonstrated no increased risk of radiographic complications with a uncemented stem at mean 12-month follow-up. Radiographs were analyzed utilizing a technique described by Sanchez-Sotelo, et al to determine if stems were considered “at risk” for clinical loosening. Lucencies were defined as >2mm in any given zone. A stem with greater than 3 zones of involvement was considered at risk for clinical lucency. In our study, lucencies were seen in 19% of uncemented and 11% of cemented stems which was not a statistically significant difference (p=0.49). More importantly, none of the stems in our study exhibited risk for clinical loosening by having greater than 3 zones of lucencies.
The factors for which there were statistically significant correlations with radiolucent defects around the implant stems included lower body weight, longer follow-up period, proximal bone resorption, and scapular notching. Time to follow-up was anticipated as lucencies tend to develop as a function of time. The significance of decreased body weight and scapular notching to the presence of humeral lucencies is uncertain.
Although proximal bone loss was notably higher in the stems with lucencies, it is important to note that there was no significant difference in proximal bone resorption between uncemented and cemented stems (69% vs 57%, respectively). These relatively high incidences of proximal bone resorption may be attributed to the types of fractures in this study. Ninety-four percent were Neer 3 or 4-part fractures involving tuberosities with comminution. Thus, many of these proximal bone fragments were either excised during the index procedure or demonstrated natural resorption over time from devascularization and are completely unrelated to the stem.
This brings up the question of whether fracture-specific implant choices should be developed and used based on the available proximal bone stock. Current fracture stems are designed for proximal diaphyseal fit (or sometimes distal metaphyseal fit) so more proximal bone resorption would theoretically be independent of stem stability. If metaphyseal bone is still available, then a more proximal engaging stem design could be of benefit to obtain more stable fixation and possibly decrease proximal stress shielding. The question then becomes is if proximal stress shielding and resorption has any clinical correlation to stem fixation and outcomes. If not, this may be clinically irrelevant.
Lastly, none of stems exhibited radiographic evidence of diaphyseal endosteal erosion, diaphyseal endosteal sclerosis, or subsidence which, if present, would have raised concern for stem fixation. The systematic review published by Phadnis et al. [8] concluded that uncemented stems had a higher incidence of early stem migration and non-progressive radiolucent lines8. This was not seen in our study as we had no stems showing subsidence and no statistical difference in radiolucent lines/lucencies. Furthermore, their systematic review also found a relative risk of 2.2 for intraoperative fracture with uncemented stems. We did not demonstrate any evidence of procedure related fracture either intraoperatively or postoperatively.
Limitations of this study include the relatively short followup period, relatively limited number of study subjects, and the inconsistencies of radiographs for comparison (rotation, penetrance, etc.). Nevertheless, our study still demonstrated statistically equivalent short-term radiographic outcomes. We hope to continue this study by correlating radiographic and clinical outcomes using validated outcome measures.
Conclusion
In conclusion, our study demonstrates no difference in radiographic complications between uncemented and cemented stems during reverse total shoulder arthroplasty in the setting of proximal humerus fracture. Moreover, our results showed no statistically significant evidence that a cemented stem is necessary in fracture applications based on radiographic review. Careful selection of implant design must be considered based on the variable amounts of proximal bone available for fixation. We still believe the choice of cemented vs uncemented stem is at the discretion of the treating surgeon on a case-by-case basis.
Acknowledgement
This study was carried out at University of Kansas School of Medicine-Wichita, USA
References
- Horak J, Nilsson BE (1975) Epidemiology of fracture of the upper end of the humerus. Clin Orthop Relat Res 112: 250-253.
- George MS, Khazzam M, Chin P, Guillaume Dumont, Robert Russell (2014) Reverse Shoulder Arthroplasty for the Treatment of Proximal Humeral Fractures. JBJS Rev 2(10): 01874474-201410000-00003.
- Smith AM, Mardones RM, Sperling JW, Robert H Cofield (2007) Early complications of operatively treated proximal humeral fractures. J Shoulder Elbow Surg 16(1): 14-24.
- Neer CS 2nd (1970) Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am 52: 1090-1103.
- Boileau P, Trojani C, Walch G, S G Krishnan, A Romeo, et al. (2001) Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elbow Surg 10(4): 299-308.
- Klein M, Juschka M, Hinkenjann B, Bernhard Scherger, Peter A W Ostermann, et al. (2008) Treatment of comminuted fractures of the proximal humerus in elderly patients with the Delta III reverse shoulder prosthesis. J Orthop Trauma 22(10): 698-704.
- Bufquin T, Hersan A, Hubert L, P Massin (2007) Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 89(4): 516-520.
- Phadnis J, Huang T, Watts A, J Krishnan, G I Bain (2016) Cemented or cementless humeral fixation in reverse total shoulder arthroplasty? a systematic review. Bone Joint J 98-B: 65-74.
- Sanchez-Sotelo J, Wright TW, O'Driscoll SW, R H Cofield, C M Rowland (2001) Radiographic assessment of uncemented humeral components in total shoulder arthroplasty. J Arthroplasty 16(2): 180-187.
- Sanchez-Sotelo J, O'Driscoll SW, Torchia ME, R H Cofield, C M Rowland (2001) Radiographic assessment of cemented humeral components in shoulder arthroplasty. J Shoulder Elbow Surg 10(6): 526-531.
- Sirveaux F, Favard L, Oudet D, D Huquet, G Walch, et al. (2004) Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br 86(3): 388-395.
- Gallinet D, Adam A, Gasse N, Severin Rochet, Laurent Obert (2013) Improvement in shoulder rotation in complex shoulder fractures treated by reverse shoulder arthroplasty. J Shoulder Elbow Surg 22(1): 38-44.
- King JJ, Farmer KW, Struk AM, Thomas W Wright (2015) Uncemented versus cemented humeral stem fixation in reverse shoulder arthroplasty. Int Orthop 39(2): 291-298.






























