External fixation for proximal humerus fractures in elderly patients
Ricardo Monreal*
Medica Vial Orthopedic Clinic, Mexico City, Mexico
Submission:July 01, 2021; Published: July 20, 2021
*Corresponding author: Ricardo Monreal, Medica Vial Orthopedic Clinic, Mexico City, Mexico
How to cite this article: Ricardo M. External fixation for proximal humerus fractures in elderly patients. Ortho & Rheum Open Access J. 2021; 18(5): 555996. 10.19080/OROAJ.2021.18.555996
Abstract
Background: Proximal humeral fractures account for 4-6% of all fractures and 25% of humeral fractures. Proximal humerus fractures are very common and often accompanied by osteoporosis in elderly population. The external fixation is one of the surgical options to treat proximal humeral fractures. The aim of this study is to evaluate the clinical and radiological results of osteosynthesis by close reduction and external fixation in the management of displaced proximal humerus fractures in elderly population.
Material and Methods: From Jan 2012 through December 2015, five elderly adult patients (≥60 years) with displaced proximal humeral fracture were treated by close reduction and external fixation using the FERN ™external fixation frame. Radiograph was used to evaluate bony union, wires migration, and fragment displacement. Clinical outcomes were evaluated the 1-10 visual analog score (VAS), and the American Shoulder and Elbow Surgeons Shoulder Score (ASES).
Results: Regarding the clinical outcomes at the final follow up, the means of the visual analogue scale (VAS), and the American Shoulder and Elbow Surgeons Shoulder Score (ASES) of the injured shoulders were 0.8 (range, 0–2), and 90.6 (range, 81–97) respectively. Radiographic bony union were noted, and external fixators were removed at 47,3± 2,9 days (range 40-63). Nonunion, implant failure, or avascular necrosis of the humeral head were observed during the follow-up.
Conclusion: Osteosynthesis with external fixator can be considered today as a valid treatment for proximal humeral fractures in elderly patients. The results in terms of functional recovery are encouraging with a reduced risk of complications.
Keywords: External Fixation; Proximal Humeral fractures; Neer classification
Introduction
Proximal humerus fractures are very common and often accompanied by osteoporosis in elderly population. They are the third most common fracture in patients older than 60 years and are the third most frequent osteoporotic fractures after wrist and hip fractures in the general population [1]. In the adult population, proximal humeral fractures have a unimodal distribution. The incidence of proximal humerus fractures fluctuates with ages. Females have the highest risk of suffering a proximal humerus fracture [1]. As with other osteoporosis-related fractures, additional risk factors for proximal humeral fractures include low bone mass and an increased risk of falls [2]. Approximately half of all proximal humeral fractures occur at home with the majority occurring because of falls on level ground. In individuals 60 years or older, over 90% of proximal humeral fractures result from a fall from a standing height. Poor vision, use of hearing aid, diabetes mellitus, cardio-vascular disease, cerebral-vascular accident, depression, alcohol consumption, use of anticonvulsive medication have been identified as being at increased risk of sustaining a proximal humeral fracture [3]. Although some studies have compared the treatments results between intramedullary pinning, plate fixation and percutaneous fixation, no consensus has been reached [4].
Plate fixation tends to achieve better biomechanical stability but requires extensive surgical exposure, therefore it is prone to complications of soft tissues as well as aseptic necrosis of the humeral head [5]. Antegrade intramedullary pinning can provide fracture reduction fixation with minimal invasion, but it may induce rotator cuff injury [6]. Percutaneous pinning is characterized by minimal invasion and low cost, but its biomechanical stability is not satisfactory. Screw pin fixation has more remarkable advantages, although patients may still display loss of fracture contraposition, which is mainly caused by fixation failure due to old age and osteoporosis [7]. The choice of the treatment depends upon various factors, must be considered: age, bone quality, fracture pattern (degree of comminution and number of main fragments), involvement of the articular surface and, somewhat, surgeon’s preference. In the elderly conservative treatment remains the treatment of choice for most proximal humeral fractures, but approximately 20% requires surgical management [8]. External fixation is generally thought to be burdened by complication as pin tract infection and loosening. The rate of pin tract infection in the literature is reported around 2 – 9 %; for this reason, in the surgical planning, it is important to evaluate patient comorbidities such as diabetes, which is a known risk factor for infection [9,10].
The aim of this study is to evaluate the clinical and radiological results of osteosynthesis by close reduction and external fixation in the management of displaced proximal humerus fractures in elderly population.
Materials ad Methods
Patients and study design
From Jan 2012 through December 2015, five elderly adult patients (≥60 years) with displaced proximal humeral fracture were treated by close reduction and external fixation using the FERN external fixation frame ™ [11].
Surgical Technique
After general anesthesia or brachial plexus block, the patient was placed in the beach-chair position. Fluoroscopy is carried out in anteroposterior and, when possible, axillary view to define fragment configuration, position, and size (Figure 1).

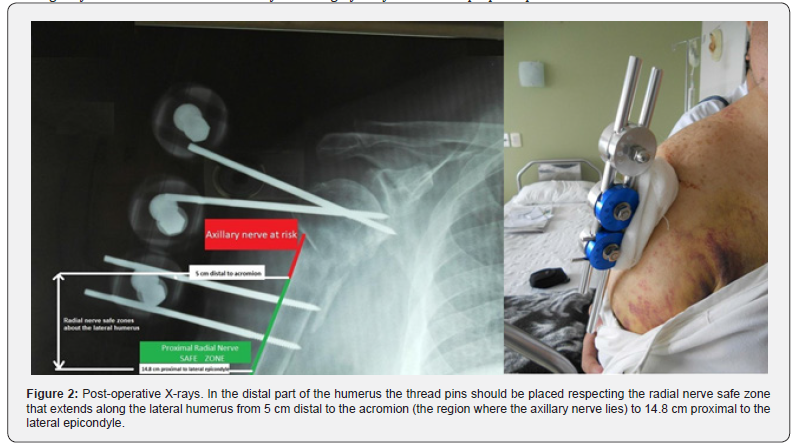
Close reduction of the fracture was achieved by manual traction and gentle manipulation; and when the desired reduction is achieved (fragment distance to <45° or decrease displacement to <1 cm), a percutaneous fixation begins. If the closed reduction is impossible, a trans deltoid 2-3 cm. incision is performed to obtain a satisfactory reduction. The fixation technique was performed using two or three threaded K-wires (diameter 2–2.5mm), depending on the size of the fragments. Two crossed threaded K-wires are inserted into the proximal fragment along the neck engaging the subchondral bone of humeral head. In distal part of the humerus, two or three more thread pins were passed parallel to engage both the cortices of the humeral shaft* [12]. All the pins related to an external rod (Figure 2).
*Attention: Radial nerve safe zone extends along the lateral humerus from 5 cm distal to the acromion (the region where the axillary nerve lies) to 14.8 cm proximal to the lateral epicondyle (Figure 2).
Postoperative Management
The limb has been placed in a triangular sling. Alternate day pin tract dressing was done. Patients were encouraged to begin active use and mobilization, mainly pendulum movement from postoperative day one to three depending upon postoperative pain. After 2weeks all movement exercises were encouraged progressing to unrestricted full range of motion except abduction initially supine position, gradually to sitting and standing position. The patients were examined thoroughly clinically and radiologically at two weeks interval. At 35 day from surgery x-ray examination is performed. The external fixator is planned to be removed at about 6 weeks. After removal patients start full active exercises in all range of motions, rotator cuff strengthening, closed chain and proprioceptive exercises.
Outcome Measures
We used following radiograph to evaluate bony union, wires migration, and fragment displacement. Postoperative clinical outcomes were evaluated using range of motion of affected glenohumeral joint, a 1–10 visual analogue score (VAS) for pain assessment, and the American Shoulder and Elbow Surgeons Shoulder Score (ASES) [13]. Outcomes were evaluated during the 2-month follow up and at the final follow up.
Results
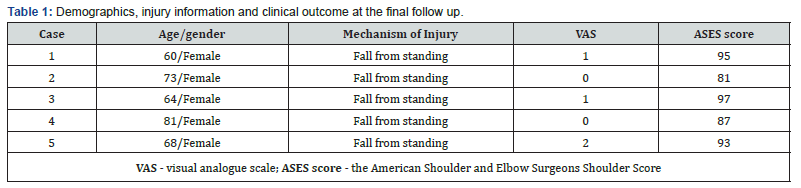
We identified 5 consecutive patients (5 women; mean age 69.2 years; age range 60–81 years) with displaced proximal humeral fracture received close reduction and external fixation. All 5 patients had been injured in a simple fall (Table 1). The mean surgical time was 32 minutes ± 3,8 (range 18-45 min) and the estimated blood loss was so low to be undetectable. Radiographic bony union were noted, and external fixators were removed at 47,3± 2,9 days (range 40-63) (Figure 3). Regarding the clinical outcomes at the final follow up, the means of the visual analogue scale (VAS), and the American Shoulder and Elbow Surgeons Shoulder Score (ASES) of the injured shoulders were 0.8 (range, 0–2), and 90.6 (range, 81–97) respectively (Table 1). Only one patient with superficial pin tract infection were observed and treated with dressings. There were no wire migrations or fracture displacements noted in our cases. Nonunion, implant failure, or avascular necrosis of the humeral head were observed during the follow-up.

Discussion
Treatment of proximal humerus fractures may be conservative or operative. A major disadvantage of non‑operative treatment is failure to obtain early mobilization, which results in a high rate of shoulder stiffness and pain and malunion or nonunion [14,15]. Disadvantage of open internal fixation is difficulty in achieving rigid fixation in the osteoporotic bone of proximal humerus. Internal fixation has been reported to have increased complication rates related with hardware loosening and pullout of the screws in elderly patients due to osteoporosis, internal fixation device prolongs, the operative time, increases intraoperative blood loss, and increases the risk of avascular necrosis of humeral head [14]. The use of external fixators in the management of proximal humeral fractures has become popular in the past decade. The principles of management for complex proximal humeral fractures are minimal soft tissue dissection to avoid the occurrence of avascular necrosis of the humeral head, adequate fixation to provide good stability for early rehabilitation. The results of our study confirm that the treatment of proximal humeral fracture in elderly patients by external fixation is a good choice thanks to the minimally invasive technique and provides good functional outcomes. Limitations of this study includes the retrospective nature, the small number of participants, and the short follow-up.
Conclusion
Osteosynthesis with external fixator can be considered today as a valid treatment for proximal humeral fractures in elderly patients to stabilize the fracture, preserve the humeral head vascularization and early mobilize the shoulder. The results in terms of functional recovery are encouraging with a reduced risk of complications.
Declarations
Disclosure of potential conflicts of interest and funding
The author declares that there is no conflict of interest related to the subject of this paper. No external source of funding was used for this study.
Statement of Human and Animal Rights
Procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- T Maluta, A Amarossi, A Dorigotti, Francesco Bagnis, Elena Manuela Samaila, et al. (2020) External fixation for proximal humerus fractures Neer type 3 and 4: results of 17 cases. Acta Biomed 91(14): e2020017.
- Lee SH, Dargent- Molina P, Breart G (2002) Risk factors for fractures of the proximal humerus: results from the EPIDOS prospective study’ J Bone Miner Res 17(5): 817-825.
- Klaus J Burkhart, Sven O Diet, Leonard Bastian, Ulrich Thelen, Reinhard Hoffmann, et al. (2013) The Treatment of Proximal Humeral Fracture in Adults. Dtsch Arztebl Int 110(35-36): 591–597.
- Karataglis D, Stavridis SI, Petsatodis G, Papadopoulos P, Christodoulou A (2011) New trends in fixation of proximal humeral fractures: a review. Injury 42(4): 330–338.
- Matziolis D, Kaeaeb M, Zandi SS, Perka C, Greiner S (2010) Surgical treatment of two-part fractures of the proximal humerus: comparison of fixed-angle plate osteosynthesis and Zifko nails. Injury 41(10): 1041–1046.
- Zhu Y, Lu Y, Shen J, Zhang J, Jiang C (2011) Locking intramedullary nails and locking plates in the treatment of two-part proximal humeral surgical neck fractures: a prospective randomized trial with a minimum of three years of follow-up. J Bone Joint Surg Am 93(2): 159–168.
- Fenichel I, Oran A, Burstein G, Perry Pritsch M (2006) Percutaneous pinning using threaded pins as a treatment option for unstable two- and three-part fractures of the proximal humerus: a retrospective study. Int Orthop 30(3): 153–157.
- Wang MQ, Youssef T, Smerdely P (2018) Incidence, and outcomes of humeral fractures in the older person: Osteoporosis Int 29(7): 1601-1608.
- Blonna D, Castoldi F, Scelsi M, Rossi R, Falcone G, et al. (2010) The hybrid technique: Potential reduction in complications related to pins mobilization in the treatment of proximal humeral fractures: J Shoulder Elb Surg 19(8): 1218–1229.
- Kazmers Nikolas H, Fragomen Austin T, Rozbruch S Robert (2016) Prevention of pin site infection in external fixation: a review of the literature. Strat Traum Limb Recon 11(2): 75–85.
- Fernandez Caycho Jose (1992) Fijación externa tubular. Acta Traumatológica Militar 1(1): 9-10.
- Plucknette B F, Tennent D J, Hsu J R, Taylor Bates, Travis C Burns, et al. (2020) Lateral External-fixation Adjacent to Radial Nerve. Cureus 12(3): 2-9.
- Michener LA, McClure PW, Sennett BJ (2002) American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg 11(6): 587–594.
- Patil YM, Patil AB, Balemane S (2012) A prospective study to study the surgical outcomes in three‑ and four‑part proximal humerus fracture with PHILOS plate. J Sci Soc 39(1): 12‑1
- Gupta AK, Gupta M, Sengar G, Nath R (2012) Functional outcome of closed fractures of proximal humerus managed by Joshi’s external stabilizing system. Indian J Orthop 46(2): 216‑2






























