Prediction of Dento-Skeletal Effects Changes in Skeletal Class II Division I In Early Adolescents and Young Adults Treated with Herbst Appliance
Davide Apicella* and Salvatore Sansalone
Calabrodental Hospital, Marrelli Health, Italy
Submission:May 02, 2021; Published: May 25, 2021
*Corresponding author: Davide Apicella, Calabrodental Hospital, Marrelli Health, Italy
How to cite this article: Davide A, Salvatore S. Prediction of Dento-Skeletal Effects Changes in Skeletal Class II Division I In Early Adolescents and Young Adults Treated with Herbst Appliance. Ortho & Rheum Open Access J. 2021; 18(3): 555986. DOI: 10.19080/OROAJ.2021.18.555986
Abstract
The present courts study investigated the effect of an orthopedic oro-facial appliance in the treatment of skeletal class II malocclusions, sagittal mandible retrusione with respect to the maxillary complex or sagittal protrusion of the maxillary complex with respect to mandible. Appliance effectiveness is recorded by radiographs films before and after treatment. The effectiveness of a bone growth and facial growth predictive method is investigated as well.
Keywords: Mandible bones; Skeletal malocclusion; Orthopedic appliances; Orthognathic surgery
Introduction
On the sagittal plane of the cranium the relative spatial position and proportion of maxillary and mandible bones are factors influencing facial profiles and the oral functions. Alteration of the normal maxillary-mandibular relationship determines skeletal dental malocclusions [1]. Growth imbalances due to genetic and environmental factors determines maxillary-mandible spatial and dimensional anomalies [2]. A protrusive position of the mandible with respect to the maxillary bone is namely classified as class II° maxillary-mandibular relationship [3]. The normal sagittal maxillary-mandibular relationship is classified as class I° such condition exists when the angle formed by sottospinale, nasale and supramental points assume values in the interval of 0° to 4° (referring to Stainer cephalometric analysis). Class II° skeletal relationships are due to a retruded position of the mandible with the respect to the Anterior Cranial Base (ACB) [4]. Or a protruded maxillary complex with respect to the ACB. In most of the causes a coexistence of the two spatial and dimensional alterations causes the class II° skeletal relationship [5]. The treatment of class II° skeletal malocclusion consists of a set of interventions aimed to re-establish a correct spatial position of maxillary and mandibular bones [6].
In adults’ patients the treatment of class II° skeletal malocclusion is achieved by orthognathic surgery or by dental compensation. In young patients (growing subject) class II° skeletal malocclusion can be treated using the orthopedic intra-oral and/or extra-oral appliances [7]. Orthopedic appliances use external forces as well as oral functions to redirect maxillary and mandibular bones growth. External forces are applied on the maxillary complex to withstand an excessive protrusive maxillary growing pattern. On the other hand, functional orthopedic appliances are aimed to enhance mandibular bone growth [8]. Most functional appliances are designed to implement mandibular length modifying mandibular condyle neck morphology and dimensions or to induce modifications of the temporal bones glenoid fossa to obtain a forward reposition of the mandible [9]. The limit of removable appliances is that their corrective potential is strongly influenced by patient compliance to therapeutic procedures [10]. On the other hand, fixed functional appliances significantly reduce the influence of patient’s compliance on therapy efficiency but are more sensible to breakage [11]. Among fixed-functional-appliances, the Herbst appliance has been re-introduced by Pancherz and is the widely used fixed-functional-appliance in the United States. Baccetti, Pancherz etc. demonstrated that timing of intervention is a key factor in the successful treatment of skeletal class II° malocclusions [12].
Timing of intervention is a fundamental factor since maxillary and mandibular bone growing rates (i.e., mm of length per year) are not linearly related to the patient ageing. In particular mandibular growth rate increases in a time interval of the growing period defined as circumpubertal period. Mandible growing rate has been related to characteristic changes of cervical vertebre morphology during the growing period. Modifications of vertebral morphology from childhood to the adulthood form is used as a skeletal maturation index to estimate the occurrence time of the mandibular growing rate peak in retro-gnatic mandible skeletal class II° malocclusions the use of a functional appliance during the mandible growing rate peak lead to an improved efficiency of the therapy and improved correction of the malocclusion. The aim of the present study is to assess the effectiveness of Petr˜vic analysis in the prediction of skeletal effects induced by Herbst appliance in skeletal class II division I early adolescents and young adults. Additionally, the efficiency of Herbst treatment in adolescents and young adults is compared.
Materials and Methods
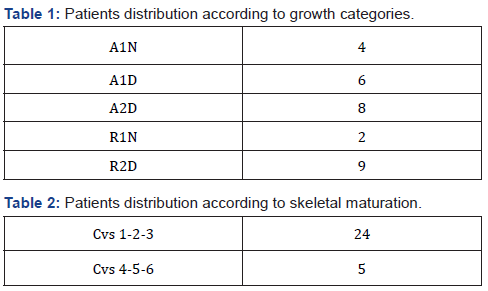
all class II division I patients with full secondary dentition who had been treated at the orthodontic department of the Calabrodental Clinic with a Herbst appliance between 2008 and 2010 where considered. For all 29 subjects lateral head films before pre-treatment (T0) and after removal of the appliance (T1) were available. All films were analyzed by standard cephalometrics analysis. According to their skeletal maturity, assessed by the Cervical Vertebral Maturazion (CVM), subjects were divided in an Adolescents Group (AG, CVM 1 to CVM 5, n=24, mean age: 13,7 years; S.D.: 1,2 years) and Young Adults (YA, CVM 6, n=5, mean age: 16,4 years; S.D.: 0,7 years). Subjects in AG and YA groups were divided in sub-groups according to Petrovic growth categories as follows: group AG (A1D, n=5; A2D, n=8; R2D, n=6; R1N, n=2; A1N, n=3), group YA (A1D, n=1; R2D, n=3; A1N, n=1).
Young subject applying for treatment at the Calabrodental Private Clinic in 2008 and meeting the following inclusion criteria:
a) Class II^ maxillary-mandibular relationship (ANB > 4.5) due to retrognatic mandible
b) Class II^, division I^ malocclusion
c) Skeletal maturation stages CVMS 1 to CVMS (according to the Baccetti’s index)
were prospectively selected for Herbst treatment.
The patients were divided in two groups according to their skeletal maturity stage. Group 1 comprises patients belonging to CVMS 1 while group 2 pooled patients belonging to CVMS 2. The mean pre-treatment age for groups 2 was…
At the starts of the treatment, the mandible was advanced to incisal edge to edge position in all subjects. For all subject treatment time was 12 months. Lateral head-film in habitual occlusion from before and after Herbst treatment was evaluated. Tracings were made and linear and angular measurement were performed to the nearest 0.5 mm and 0.5 degrees, respectively. All registration were done twice. For the final evaluation, the mean value of the duplicate registration was used. No correction was made for linear enlargement (approximately 6% in the median sagittal plane).
Dentoskeletal changes
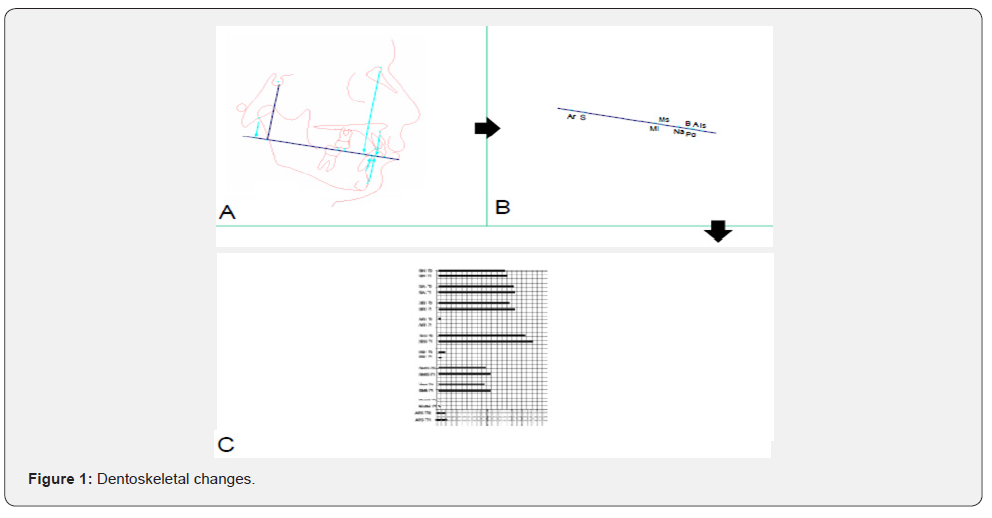
Pre-and post-treatment lateral headfilms were analyzed according to the method of Pancherz (Figure 1A). For all the recording on pre- and ost-treatment radiographs, the occlusal line (OL, defined by the incisal tip of the most protruted mandibular incisor and the ditobuccal cusp of the of the first permanent mandibular molar) and the occlusal line perpendicular (OLp) from the first headfilm were used as a reference grid (Figure 1B). Superimposition of the radiographs was performed on the stable bone structure of the anterior cranial base. The roentgenographic analysis comprises the following linear variables.
is/OLP minus ii/OLP = Overjet
a) ms/OLP minus mi/OLP = Molar relationship (positive value indicates distal relationship, negative value indicates normal or mesial relationship)
b) is/OLP = Position of the maxillary central incisor
c) ii/OLP = Position of the mandibular central incisor
d) ms/OLP = Position of the maxillary permanent first molar
e) mi/OLP = Position of the mandibular first molar
f) ss/OLP = Position of the maxillary jaw base
g) pg/OLP = Position of the, andibolar jaw base
h) ar/OLP = Position of the condyle
i) pg/OLP plus ar/OLP = Mandibular length
Changes in the different measuring points in relation to OLP during treatment were calculated as the “after-minus-before” difference in landmark position. Changes in variables 3 to 6 represent a composite effect of skeletal changes. Variables for dental changes within the maxilla and mandible were obtained by the following calculations (variables 11 to 14)
j) is/OLP (d) minus ss/OLP(d) = Changes in position of the maxillary permanent first molar within the mandible
k) ii/OLP (d) minus pg/OLP (d) = Changes in position of the mandibular incisor within the mandible
l) ms/OLP (d) minus ss/OLP (d) = Changes in position of the maxillary permanent first molar within the maxilla
m) mi/OLP (d) minus pg/OLP (d) = Changes in position of the mandibular permanent first molar.
Statistical Methods
The arithmetical mean (mean) and standard deviation (SD) were calculated for the different variables. Student’s t-tests for unpaired samples were performed to assess skeletal maturity group differences. The statistical significance was determined at the 0,1% and 5% levels of confidence. A confidence level larger than 5% was considered statistically not significant (n.s.) (Figure 1C).
Results
a t-test was used to evaluate variations between pre- and post-treatment chephalometric measures. AG and YA groups patients were treated successfully to class I occlusal relationships with normal overjet and overbite. Skeletal changes contributing to overjet and molar relationships was smaller in YA group (10% and 16% respectively) with respect to the AG group (63% and 55% respectively). Mandibular base advancement, decrease in the ANB angle, Wits appraisal and facial convexity observed in group AG were significantly higher than those observed in group YA. No statistically significant differences were observed among A1D, A2D, R2D, R1N and A1N sub-groups in AG groups; statistically significant differences were observed between R2D - AG and R2D-YA sub-groups (Tables 1 & 2).
Conclusion
good treatment results were achieved in both adolescent and young adults’ groups, however more skeletal effects were observed in adolescent’s groups. Within the limits of the present study Petr˜vic analysis was found not predictive of the changes induced by the Herbst appliance.
References
- Pancherz H (1982) The mechanism of Class II correction in Herbst appliance treatment. A cephalometric investigation. Am J Orthod 82(2): 104-113.
- Wieslander L (1984) Intensive treatment of severe Class II malocclusions with a headgear-Herbst appliance in the early mixed dentition. Am J Orthod 86(1): 1-13.
- Pancherz H (1985) The Herbst appliance--its biologic effects and clinical use. Am J Orthod 87(1): 1-20.
- Pancherz H, Hägg U (1985) Dentofacial orthopedics in relation to somatic maturation. An analysis of 70 consecutive cases treated with the Herbst appliance. Am J Orthod 88(4): 273-287.
- Woodside DG, Metaxas A, Altuna G (1987) The influence of functional appliance therapy on glenoid fossa remodeling. Am J Orthod Dentofacial Orthop 92(3): 181-198.
- Pancherz H, Fackel U (1990) The skeletofacial growth pattern pre- and post-dentofacial orthopaedics. A long-term study of Class II malocclusions treated with the Herbst appliance. Eur J Orthod 12(2): 209-218.
- Hansen K, Pancherz H, Petersson A (1990) Long-term effects of the Herbst appliance on the craniomandibular system with special reference to the TMJ. Eur J Orthod 12(3): 244-253.
- Pancherz H (1991) The nature of Class II relapse after Herbst appliance treatment: a cephalometric long-term investigation. Am J Orthod Dentofacial Orthop 100(3): 220-233.
- Hansen K, Pancherz H, Hägg U (1991) Long-term effects of the Herbst appliance in relation to the treatment growth period: a cephalometric study. Eur J Orthod 13(6): 471-481.
- Hansen K (1992) Post-treatment effects of the Herbst appliance. A radiographic, clinical and biometric investigation. Swed Dent J Suppl 88: 1-49.
- Hansen K, Pancherz H (1992) Long-term effects of Herbst treatment in relation to normal growth development: a cephalometric study. Eur J Orthod 14(4): 285-295.
- Schiavoni R, Grenga V, Macri V (1992) Treatment of Class II high angle malocclusions with the Herbst appliance: a cephalometric investigation. Am J Orthod Dentofacial Orthop 102(5): 393-409.c






























