Evaluation of Normal and Pathological Patellar Tendon by Real- Time Shear Wave Elastography
Ahmed Abu-Awwad1, Cosmin Ioan Faur1*, Mariana Tudoran1, Pompiliu Horatiu Petrescu1, Roxana Folescu2, Andrei Motoc3, Mirela Loredana Grigoras3, Cristina Tudoran1, Ion Lucian Ghiga1, Jenel Marian Patrascu1 and Alexandru Popa4
1Department of Orthopedics and Traumatology, “Victor Babeş” University of Medicine and Pharmacy, Romania
2Department of Balneology, Clinical Recovery and Rheumatology; “Victor Babeş” University of Medicine and Pharmacy, Romania
3Department of Anatomy and Embriology, “Victor Babeş” University of Medicine and Pharmacy, Romania
4Department of Internal Medicine, Centre of Elastography, “Victor Babeş” University of Medicine and Pharmacy, Romania
Submission:April 20, 2021; Published: April 30, 2021
*Corresponding author: Cosmin Ioan Faur, Department of Orthopedics and Traumatology, “Victor Babeş” University of Medicine and Pharmacy, Eftimie Murgu Sq. Nr.2, 300041, Timis, Timisoara, Romania
How to cite this article: Ahmed A-A, Cosmin I F, Mariana T, Pompiliu H P, Roxana F, et al. Evaluation of Normal and Pathological Patellar Tendon by Real- Time Shear Wave Elastography. Ortho & Rheum Open Access J. 2021; 18(2): 555982. DOI: 10.19080/OROAJ.2021.18.555982
Abstract
Tendinopathy covers a range of several tendon conditions, mostly caused by overuse but at least in patellar tendon pathology, increased by obesity, diabetes, inflammatory and autoimmune conditions. Subclinical tendon pathology is difficult to diagnose, as magnetic resonance imaging (MRI) examinations are sometimes inconclusive and non-cost-effective. Elastography is an ultrasound examination method that uses mechanical impulses to produce shear waves in the tissue of interest, than measures the tissue displacement and calculates the shear wave speed or the elastic modulus of the examined tissue. We have used B-mode ultrasonography and share wave elastography on 52 patellar tendons from healthy volunteers with or without tendon pathology history, and correlated the data obtained with the clinical parameters of the volunteers, such as age, body mass index (BMI) and sports practice. We have shown that there is no significant correlation between the elastic modulus of the patellar tendon and age, sports practice and BMI. Share wave elastography has proved to be cost- effective for the patellar tendon in healthy volunteers and was able to monitor evolution of one patient with old knee problems treated conservative. It can complete investigation and it can replace B-mode ultrasonography particularly in monitoring the post-surgery evolution.
Keywords: Patellar tendon; Tendinopathy; Share wave elastography; knee pathology
Introduction
By definition, the patellar tendon is a ligament that connects patella to tibial tubercle. It is approximately 30 mm wide by 50 mm long and have a thickness of 5-7 mm [1]. The patellar ligament has the origin in the patellar apex, but it is considered the distal part of the quadriceps tendon, and the insertion on tibial tuberosity, being a part of the extensor mechanism of the knee [2]. The development of patellar tendon pathology is influenced by several risk factors, which may increase the strain of the patellar tendon. The main risk factors that contribute to patellar tendinopathy are weight, body mass index, leg length difference, quadriceps flexibility and strength, hamstring flexibility and vertical jump performance [3].
Patellar tendinopathy usually affects athletes involved in jumping sports, but also in older people, because of degenerative process which results from repetitive micro-damages over time. Tendinopathy is a generic term comprising a whole area of different pathologies, ranging from degenerative to post- traumatic, metabolic or inflammatory conditions of the tendon, such as paratenonitis, bursitis, tendinosis [4-6]. Patellar tendinopathy is a common condition manifested by anterior knee pain. The diagnosis is established by a thorough history and physical examination, but imaging is the gold standard. Most cases are resolved with nonsurgical treatment, like eccentric exercises, cryotherapy, anti-inflammatory drugs, corticosteroid injections, platelet-rich plasma injections or ultrasound-guided sclerosis. Once patients pass the first inflammatory phase and remain symptomatic, surgical treatment becomes a necessary option [5-8].
The evaluation of the elastic properties of a tissue was firstly reported in 1991 by ultrasound image [9], but the development of magnetic resonance imaging (MRI) made this imaging technique the gold standard for the evaluation of soft tissue lesions, particularly tendons and muscles [10]. A new method used to evaluate tissue elasticity based on differences in stiffness between different biological tissues is the ultrasound elastography (USE) [11]. The main advantage of USE consists in an increased sensitivity to detect the modifications of the viscoelastic properties of the tendon, that appear in tendinopathy [12], and can be early detected even before the abnormalities are being visible on conventional B-mode ultrasonography [13]. There are two major techniques used in USE: Compression elastography (CE) and Shear wave elastography (SWE). Comparing to SWE, conventional B-mode ultrasonography has severe limitations in tendon elastography because the transducer must be held in the same position relative to the tendon fibers during compression and it depends on the ability of the examiner [14]. In tendon elastography, the most often used are shear-wave speed measurements. The transducer can capture high frame rate images of the tissues, therefore assessing the shear wave propagation speed very accurately and reducing the variability observed in axial strain elastography [15].
Materials and Methods
This study includes a group of 52 healthy young volunteers without any preexistent tendon pathology. The inclusion criteria were the age of the patients – all subjects were between 19-29 years old, and the absence of previous knee pathology. Body mass index (BMI) and information regarding the activity level of the subjects were recorded. Patellar tendon length and diameter were measured by Q-Box Mode, then mid-tendon longitudinal elastographic valid measurements were performed for each tendon using an Aixplorer system (SuperSonic Imagine Inc., France) with a linear high-resolution transducer 15-4 MHz, subjects at the edge of the bed, with the foot at 90 degrees.
Three valid measurements were performed for each tendon, then an average value of the elastic modulus was obtained, expressed in kPa. The values obtained were statistically processed using the statistical expansion of Microsoft Office software pack, to assess the feasibility of the method in evaluation of the tendon state, at healthy subjects between 19-29 years old. With subjects sitting in the dorsal decubitus, at the edge of the bed with the knee at 90 degrees, 5 values were elastographically measured, starting with the proximal portion and ending at the tibial insertion level. Following the 5 elastographic measurements, the median of the 5 values was calculated, this being practically the elastographic reference value of the analyzed patellar tendon. After calculating the median of the 5 values, an average of the respective value was achieved, both for male and female patients, this being: 273,6862745 kPa.
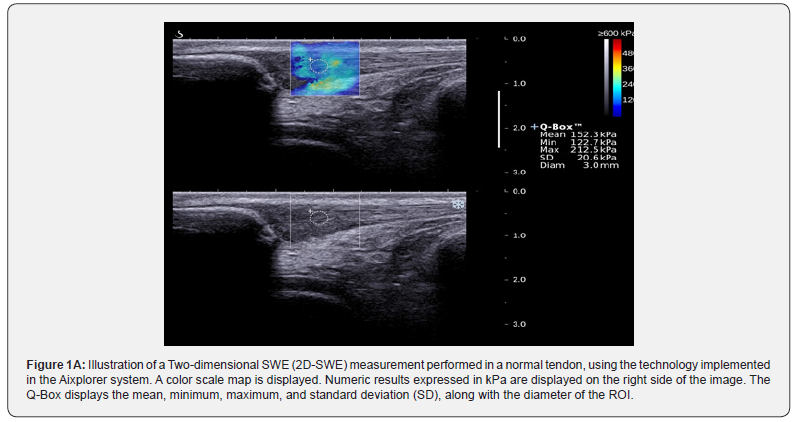
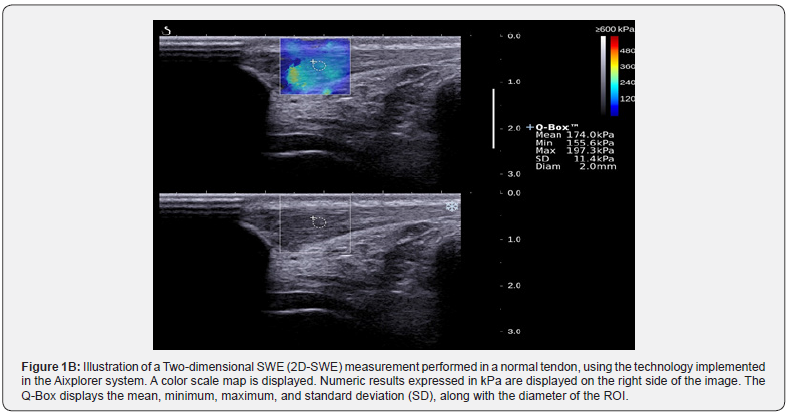
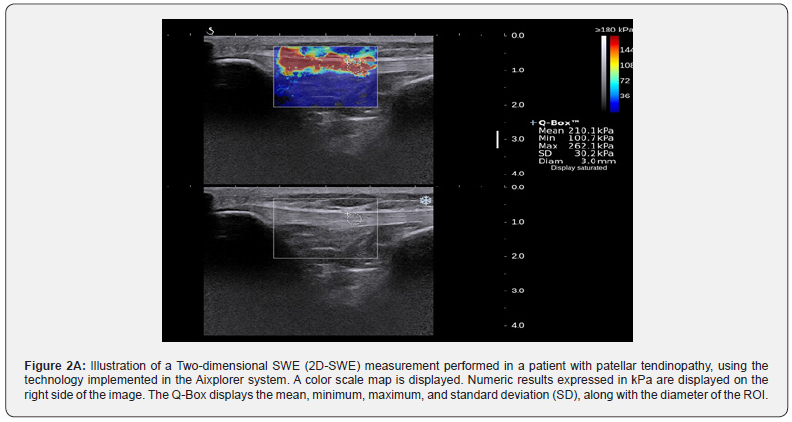
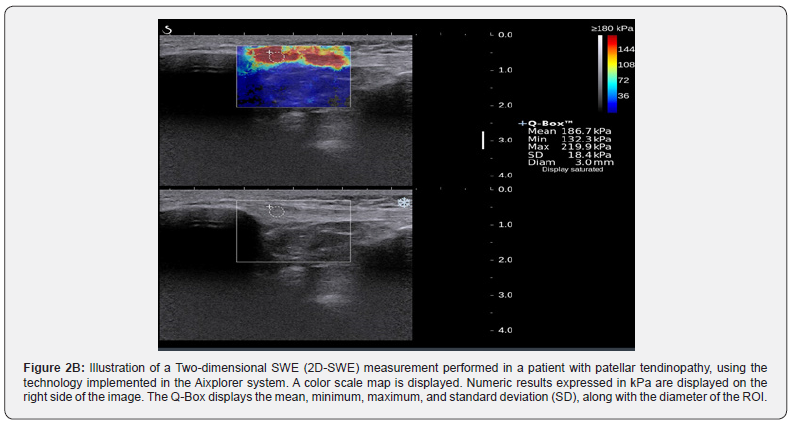
The elastographic ultrasound images were displayed in parallel with the B-mode ultrasound images, allowing for the region of interest (ROI) selection of the tendon part that undergoes elastographic measurements. In normal patients without history of tendon lesions, the tendon was stiff, with relatively uniform color-coded blue image on the elastogram. Areas of soft tissue, color-coded red, could be identified in another volunteer, with possible diagnostic significance of a preclinical lesion. The person will be performed follow-up by ultrasound imaging coupled with elastography, to perform early diagnosis of a tendinopathy, particularly if the volunteer is a sport practitioner. The elastographic evaluation of the patellar tendon were performed using different ROI than in the images depicted, and yielded values of the elastic modulus ranging between 122 and 498kPa. The study protocol was approved by the institutional board.
Results
The men vs women ratio of the volunteers in this study was 1: 3.63, body weight of 40-65 kg in women and 60-90 kg in men, respectively, with a BMI of 18.71-27.4 and 16.19- 26.74 in men and women, respectively. The mid-tendon area was calculated by the formula A=πD1D2/4, where D1 represents the antero-posterior diameter, while D2 represents the transversal diameter. The tendon area was calculated along his insertion and ranged in men and women volunteers ~ 273,6862745 kPa. The elastographic ultrasound images were displayed in parallel with the B-mode ultrasound images, allowing for region of interest (ROI) selection of the tendon part that undergoes elastographic measurements. In normal patients, without history of tendon lesions, the tendon was stiff, with relatively uniform blue color-coded image on the elastogram, with values between 165.44 and 178.67 kPa (Figures 1A & 1B). Areas of soft tissues, color-coded red, were identified in another volunteer, with possible signification of preclinical lesion (Figures 2A & 2B). The elastographic evaluation of the patellar tendon was performed using different ROI than in images depicted and yielded values of the elastic modulus ranging between 112.002 and 163kPa.
Discussion
Ultrasound elastography is a recent technology that has a major development in the past two decades [16]. In this study there were analyzed the two major techniques used in musculoskeletal ultrasound (conventional B-mode ultrasonography and shearwave elastography) in the context of tendon pathology. Ultrasound elastography is a new method used to evaluate the tissue elasticity based on differences in stiffness between different biological tissues. Elastographic imaging of soft tissue is one of the major improvements of the ultrasound investigation, so it can give us important diagnostic and prognostic information, is non-invasive, requires less expensive equipment than MRI, it is equally sensitive and specific, and does not require significant training. SWE can give morphological information and can quantify the absolute elasticity value of soft tissue structures [17]. Shear waves can be induced through various methods, such as US push beams (supersonic shear imaging) or by external mechanical vibrations (transient elastography). These waves can be either longitudinal, where the particles oscillate in the direction of wave propagation, or transversal, in which particles oscillate perpendicular to the direction of wave propagation. The transverse wave propagation speed is called the shear-wave velocity(Vs) [16-19]. One of the mechanical properties of tissues, musculoskeletal elasticity, is mostly affected by age, BMI, sex and muscle strength, and some neuromuscular and orthopedic disorders [16]. When is properly performed, this method can be used to evaluate the healing progress of the tendon after surgery or to detect preclinical tendon lesions [17,20]. Because most tendons are formed by different collagen fibers bundles/fascicles and with different insertions/origins, examination of the tendons can be difficult and elastographic images and data could differ significantly, it is necessary to have an exam standardization.
In our study we have obtained values of the elastic modulus like other published studies, but also with some differences concerning the correlation with age or tendon thickness in symptomatic patients. We questioned pubmed.ncbi.nlm.nih. gov. by the keywords “patellar tendon by real-time shear wave elastography” and found five studies using USE (two using CE and three using SWE), whose results were discrepant concerning elasticity features. Two studies, for example, using SWE, described an increase of Vs (shear-wave velocity) and, therefore, stiffness in patellar tendinopathy; there are important methodological differences that can explain this distinctions, like the regions of the same tendon were assessed and different sizes of ROIs were used. In the article published by Dirrichs et al. [21] measurements of Vs using an ROI of 1 mm in diameter placed at the most rigid area of the tendon were performed; the second study realised by Coombes et al. used a larger ROI and measured Vs at the middle and proximal parts of the tendon [22]. In another study, Zhang et al. measured Vs at a proximal part of the tendon; Also, in the research realized by Zhang et al., by using SWE, was evaluated 13 athletes with unilateral patellar tendinopathy and was found a correlation between increased stiffness of painful tendon and the intensity of pain and degree of dysfunction [23]. The conclusion was that the elastic modulus is influenced directly proportional by the size of the ROI (Kot et al. [24,25] and by the assessed tendon portion [26].
Conclusion
Ultrasound elastography is a new method used to evaluate the tissue elasticity based on differences in stiffness between different biological tissues. Elastographic imaging of soft tissue is one of the major improvements of the ultrasound investigation, so it can give us important diagnostic and prognostic information, is noninvasive, requires less expensive equipment than MRI, it is equally sensitive and specific, and does not require significant training. SWE has been proved as a reliable and cost-effective method for the evaluation of patellar tendons in healthy volunteers and can be used to monitor post-surgery evolution of the patients with knee pathology, caution must be taken during image acquisition as the patellar tendon is a highly anisotropic medium and this might alter the results obtained.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Morton WS, Valle X, Diaz-Cueli D, Malliaras P, Morris ey,D (2017) Patellar Tendinopathy and Potential Risk Factors: An International Database of Cases and Controls. Clin J Sport Med 27(5): 468-474.
- Basso O, Johnson DP, Amis AA (2001) The anatomy of the patellar tendon. Knee Surg Sports Traumatol Art 9(1): 2-5.
- Worp H, Ark M, Roerink S, Pepping GJ, Akker-Scheek I, et al. (2011) Risk factors for patellar tendinopathy: a systematic review of the literature. Br J Sports Med 45(5): 446-452.
- Oystein B Lian, Lars Engebretsen, Roald Bahr (2005) Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med 33(4): 561-567.
- Schwartz A, Watson JN, Hutchinson MR (2015) Patellar Tendinopathy. Sports Health 7(5): 415-420.
- Oana Suciu, Radu Prejbeanu, Horia Haragus, Cosmin Faur, Roxana Ramona Onofrei(2020) Cross Cultural Adaptation and Validation of the Romanian Marx Activity Rating Scale for Anterior Cruciate Ligament Reconstruction. Healthcare 8(3): 318.
- Terry A Adirim, Tina L Cheng (2003) Overview of injuries in the young athlete. Sports Med 33(1): 75-81.
- Roald Bahr, Bjorn Fossan, Sverre Loken, Lars Engebretsen (2006) Surgical treatment compared with eccentric training for patellar tendinopathy (jumper’s knee). A randomized, controlled trial. J Bone Joint Surg Am 88(8): 1689-1698.
- J Ophir, I Cespedes, H Ponnekanti, Y Yazdi, X Li (1991) Elastography: a quantitative method for imaging the elasticity of biological tissues. Ultrason Imaging 13(2): 111–134.
- Niculescu B, Faur CI, Tataru T, Diaconu BM, Cruceru M (2020) Investigation of Biomechanical Characteristics of Orthopedic Implants for Tibial Plateau Fractures by Means of Deep Learning and Support Vector Machine Classification. Appl Sci 10(14): 4697.
- LaPrade, Kallenbach SL, Aman ZS, Moatshe G, Storaci HW, et al. (2018) Biomechanical Evaluation of the Medial Stabilizersof the Patella. Am J Sports Med 46(7): 1575-1582.
- Aubry S, Nueffer JP, Tanter M, Becce F, Vidal C, et al. (2015) Viscoelasticity in Achilles tendonopathy: quantitative assessment by using real-time shear-wave elastography. Radiology 274(3): 821–829.
- Hsiao MY, Chen YC, Lin CY, Chen WS, Wang TG (2015) Reduced patellar tendon elasticity with aging: in vivo assessment by shear wave elastography. Ultrasound Med Biol 41(11): 2899–2905.
- Shiina T, Nightingale KR, Palmeri ML, Hall TJ, Bamber JC, et al. (2015) WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 1: basic principles and terminology. Ultrasound Med Biol 41(5): 1126–1147.
- Buck AR, Verstraete N, Li Y, Schweizer A, Snedeker JG, et al. (2012) Detection of small tendon lesions by sonoelastographic visualization of strain profile differences: initial experiences. Skeletal Radiol 41(9): 1073–1079.
- Prado-Costa R, Rebelo J, Monteiro-Barroso J, Preto AS (2018) Ultrasound elastography: compression elastography and shear-wave elastography in the assessment of tendon injury. Insights Imaging 9(5): 791-814.
- Docking SI, Ooi CC, Connell D (2015) Tendinopathy: is imaging telling us the entire story? J Orthop Sports Phys Ther 45(11): 842–852.
- Bercoff J, Tanter M, Fink M (2004) Supersonic shear imaging: a new technique for soft tissue elasticity mapping. IEEE Trans Ultrason Ferroelectr Freq Control 51(4): 396–409.
- Gehmert S, Jung E M, Kugler T, Klein S, Gehmert S, et al. (2012) Sonoelastography can be used to monitor the restoration of Achilles tendon elasticity after injury. Ultraschall Med 33(6): 581–586.
- De Zordo T, Fink C, Feuchtner GM, Smekal V, Reindl M, et al. (2009) Real-time sonoelastography findings in healthy Achilles tendons. AJR Am J Roentgenol 193(2): W134– W138.
- Dirrichs T, Quack V, Gatz M, Tingart M, Kuhl CK, et al. (2016) Shear wave elastography (SWE) for the evaluation of patients with tendinopathies. Acad Radiol 23(10): 1204–1213.
- B K Coombes, K Tucker, B Vicenzino, V Vuvan, R Mellor , L Heales, et al. (2018) Achilles and patellar tendinopathy display opposite changes in elastic properties: a shear wave elastography study. Scand J Med Sci Sports 28(3): 1201–1208.
- Zhang ZJ, Ng GY, Lee WC, Fu SN (2014) Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS One 9(10): e108337.
- Kot BC, Zhang ZJ, Lee AW, Leung VY, Fu SN (2012) Elastic modulus of muscle and tendon with shear wave ultrasound elastography: variations with different technical settings. PLoS One 7(8): e44348.
- Ozcan AN, Tan S, Tangal NG, Saliha Cıracı, Savas Kudas, et al. (2016) Real-time sonoelastography of the patellar and quadriceps tendons: pattern description in professional athletes and healthy volunteers. Med Ultrason 18(3): 299–304.
- Tsuchida W, Yamakoshi Y, Matsuo S, Asakawa M, Sugahara K, et al. (2020) Application of the novel estimation method by share wave elastography using vibrator to human skeletal muscle. Sci Rep 10(1): 22248.






























