Surgical Management of Lumbar Spondylolisthesis (A Study of 25 Cases)
Oussma Eladaoui*, Sidi Elhacen, Ayoub Rahmi, Mohamed Rafai and Abdelhak Garch
Department of Traumatology and Orthopedic Surgery P32, University Hassan II, Casablanca, Morocco
Submission:June 23, 2020; Published:July 08, 2020
*Corresponding author: Oussma Eladaoui, Department of Traumatology and Orthopedic Surgery P32, University Hassan II, Casablanca, Morocco
How to cite this article: Oussma E, Sidi E, Ayoub R, Mohamed R, Abdelhak G. ISurgical Management of Lumbar Spondylolisthesis (A Study of 25 Cases). Ortho & Rheum Open Access J. 2020; 16(4): 555941. DOI: 10.19080/OROAJ.2020.16.555941
Abstract
The surgical techniques used for the treatment of spondylolisthesis have considerably evolved in the last few years. The equipements have progressed, the techniques of approaches have been better mastered and the rate of complications has seriously decreased. This work allowed the evaluation of 25 patients with spondylolisthesis operated by fusion with instrumentation, with or without intersomatic arthrodesis. It was found that the clinical and functional scores were significantly improved one year after the surgery. A75% improvement was noticed in the VAS (Visual Analog Scale) and a 68% improvement in the Oswestry score with a significantly improved quality of life. The radiological outcome was evaluated by measuring the sliding postoperative gain of 66%; The functional results are quite similar to the other literature series. The positive results on radicular compression show the effectiveness of the decompression gesture systematically associated with arthrodesis.
Keywords: Lumbar spondylolisthesis; Spinal fusion; Posterior approach; Sagittal balance
Introduction
Spondylolisthesis is defined by the sliding of a vertebra in relation to the underlying vertebra, it is a relatively frequent form of vertebral instability, L5-S1 is the most affected, this displacement is sometimes well tolerated but often responsible of mechanical lumbar pain or even sensory, motor or rarely vegetative neurological deficit [1]. The distinction between the different stages is made by Meyerding classification [2]. The surgical indication is retained only after the failure of a conservative treatment well led on a symptomatic patient or showing signs of instability and scalability, the surgical treatment aims to neurological decompression and vertebral stability. Several surgical techniques for lumbosacral arthrodesis via the anterior or posterior approach currently exist, making it possible to obtain reduction and intervertebral fusion by posterolateral and intersomatic grafting.
Materials and Methods
This is a retrospective study carried out in the orthopedic surgery and trauma departement P32 in the university hospital center (CHU Casablanca), concerning all patients operated on for spondylolisthesis (degenerative or isthmic lysis) during the period from January 2014 to the month of December 2019. Patient data was collected from our service files, and from patient monitoring to consultation. The aim of our study is to evaluate the surgical technique used for the treatment of spondylolisthesis, by comparing the preoperative clinical and radiological status with the postoperative results over an average follow-up of 38.5 months (6 months - 72 months).
Results
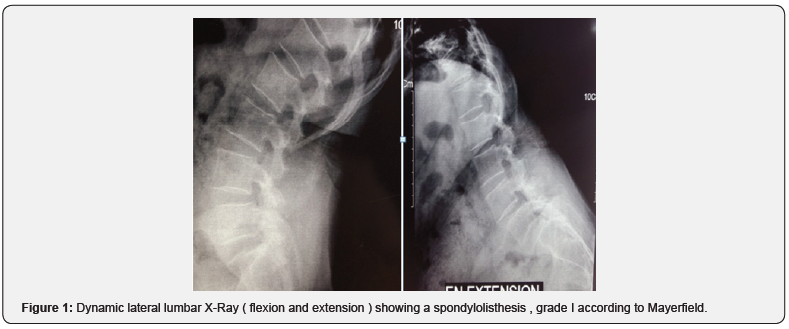
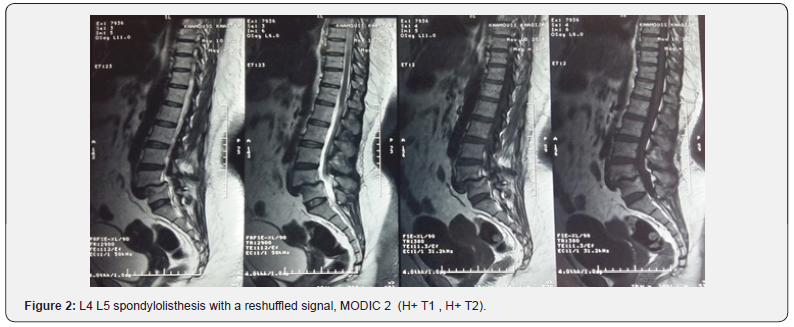
25 patients, 88% of whom were women, were included in our work, the average age was 54 years (34 to 70 years). At the time of the initial examination, all the patients had a severe mechanical low back pain which was rebellious to a well-managed medical treatment, 80% of the patients complained of radiculalgia, most often affecting the L5 and / or S1 territory. 14 patients had neurological claudications, 4 patients with motor neurological deficit; These disorders are in the form of functional impairment affecting the two lower limbs with an average rating of 3/5, 14 patients with sensory disorders : Hypoesthesia and Tingling of the lower limbs, and genito-sphincter disorders in two patients. The preoperative evaluation was based on the assessment of low back and radicular pain according to the visual analogue scale evaluation (VAS), the average score was 6 (4-9), and the patients’ quality of life evaluated according to the score d ‘Oswerstry (satisfaction index) with an average of 62 (40-80). The preoperative radiological analysis in our patients was based on x-rays of the lumbar spine (antero-posterior and lateral views) , dynamic images in flexion and extension (Figure 1), as well as magnetic resonance imaging. Isthmic lysis was the most frequent etiology of spondylolisthesis (56%), L5-S1 was its most frequent site (15 cases), the degree of slippage evaluated according to the MEYERDING classification showed that 56% of patients had a Grade I (Figure 1), and 44% had a Grade II. On MRI, stage I disc disease according to the MODIC classification was differentiated in 12 patients, stage II in 8 patients (Figure 2), 16 patients had an associated herniated disc, i.e. 64%, among the 25 cases, 14 patients had root compression i.e 56%.
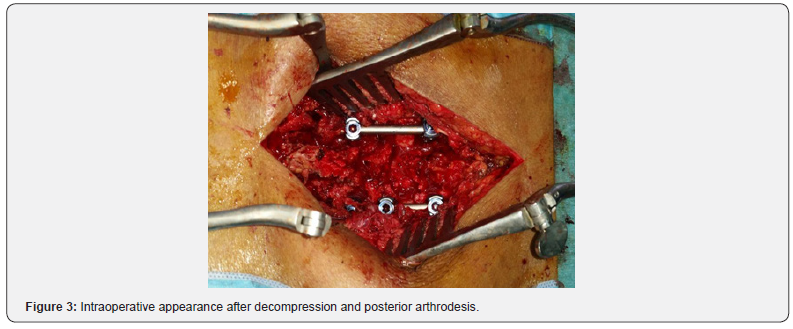
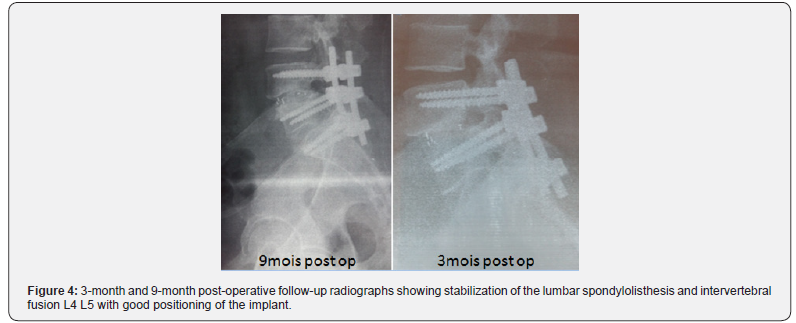
In our series, surgical treatment was indicated following resistance to medical treatment, or for the onset of a neurological disorder. The most used technique in our series was the posterior inter-somatic arthrodesis (PLIF), which consisted in resecting the mobile posterior vertebral arch and releasing the roots in the foramina with posterolateral arthrodesis and fixation by osteosynthesis (Figure 3), associated if necessary with a discectomy and placement of an intersomatic cage, the correct positioning of the implant was verified in all cases during early control radiographic examinations (Figure 4), all our patients benefited from rehabilitation postoperative with first lift allowed on the third postoperative day under cover of a lombostat, which was worn for 2 to 6 months. The average length of hospital stay was 8 days (5 to 15 days). The patients were followed regularly in consultation with an average follow-up of 38 months. The complications found in our series were: a dural breach that was sutured without any follow-up, two cases of superficial postoperative infections. The clinical (VAS) and functional (Oswestry) scores were significantly improved one year after surgery, a 75% improvement in (VAS) with a preoperative mean at 6 and postoperative at 1.5, a 68% improvement in the score of Oswestry with an average preoperative value at 62 and postoperative at 20. The radiological evolution was evaluated by measuring the postoperative gain in slip which was 66% with an average preoperative slip at 29% and postoperative at 11%.
Discussion
In our study, the average age is 54 years, consistant with the literature [3], the advanced age is not a predictor of surgical treatment failure ;Thus, there is no parallelism between the age and the results of spondylolisthesis surgery. A clear predominance of women was found in the majority of the series with a percentage of 53.1% [3], 75% [4]. In our series 88% of our patients were female, this clear predominance of women can be explained by the special status of women in our society: housework, work in the fields, demanding work throughout the day. Low back pain is the main reason for our patients consultation, our results are quite close to those found in the literature 84% for ROY-CAMILLE and AL [5]. Radiculalgia is the second symptom, it was found in 80% of our patients. These results join those of the literature with frequencies of 72% [5] and 77% [2], respectively. MRI in our series allowed us to classify disc disease; Among our patients, five had a normal signal (20%), 12 had a stage I (48%) and eight had a stage II (32%). thus joining the data from the Cervantes series [6]: stage 0 (22%), stage I (72%) and stage II (6%). It made it possible to objectify an associated disc herniation in 64% of patients, these results were increased compared to the studies of IBA BA and AL [7] and Benallel [8] with a respectively 38% and 32% frequency, and to seek a radicular compression which was present in 56% of our patients, with results close to the series of IBA BA and AL [7] (52%). Surgical treatment was indicated only in the presence of symptomatic spondylolisthesis, who were resistant to wellmanaged medical treatment for at least three months, or as a firstline treatment in the event of significant neurological deficit [9], the aim of the treatment is to suppress the pain by decompressing nervous elements, surgery is also indicated in the event of the glide worsoning by more than 50%, spinal static disorder, and in the presence of ponytail syndrome [7].
It was Cloward who first described posterior interbody fusion in 1953, a technique which combines direct and indirect root decompression with interbody fusion by autologous graft (posterior lumbar interbody fusion), but the practice of this technique has gradually decreased due to the significant rates of complications and the non-union reported. Several modifications were subsequently added to it. Steffee and Sitkowski have described for the first time the addition of a posterior osteosynthesis to the intersomatic arthrodesis [10]. This technique is currently the most used since it has allowed a wider decompression without a risk of destabilization; Therefore , a better visualization of the nervous elements and a decreased the rate of complications [11- 13]. The combined arthrodesis (intersomatic and posterolateral) associated with an osteosynthesis allows a more lasting reduction in sliding compared to a simple posterolateral arthrodesis associated with an osteosynthesis, even if the difference in reduction is not significant in immediate postoperative, it is much greater distance from the intervention [12]. In addition, it offers a better fusion rate (95%) than interbody fusion alone (86%), as well as posterolateral arthrodesis (69%) [14].
Lumbar pain, a key parameter for the evaluation of postoperative clinical results, as this is a subjective sign, its evaluation must take into account certain physical and psychological factors which can influence the results [15]. Haefeli [16] estimates that, for the surgical treatment, to be beneficial for low back pain, variations on the VAS scale of 20% for chronic pain and 12% for acute pain must be obtained for a real clinical modification be felt. In our series, the VAS was significantly improved one year after surgery (75%). Neurological recovery was the rule in all patients with a neurological deficit previously in our series, which joins the series of IBA BA et al. [7] with a frequency of 93.7%. We have chosen to compare the pre and postoperative results with the percentage of slip, in our series, the average gain percentage is 66%, our results are close to those of Omidi-Kashani [16], decreasind percentage to 52, 2%. Although vertebral decompression with fusion and posterior instrumentation in the surgical treatment of patients with LDS results in a satisfactory result, vertebral reduction cannot significantly improve clinical improvement [17].
Conclusion
This work allowed the evaluation of 25 patients with operated LPS. It turns out that at the last follow-up the functional results are quite similar to the other series in the literature. The positive results on radiculalgia, witnesses of the effectiveness of the decompression gesture systematically associated with arthrodesis. The management of these patients must integrate rigorous monitoring, good education to understand the evolutionary risks and the choice of the “right time to operate” before the posture becomes disorganized, especially in the sagittal plane.
Conflict of Interest
The authors of this article declare that they have no conflict of interest affecting this study.
References
- Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equili-brium of pelvis and spine. Eur Spine J 11(1): 80–88.
- Meyerding HW (1932) Spondylolisthesis. Surg Gynecol Obstet 54: 371–377.
- Shakeel Ahmad, Syed Hasan Danish, Farah Ahmad, Sahira Naz, Ayesha Tahir, et al. (2013) Frequency of Spondylolisthesis among Patients of Chronic Low Back Pain in Karachi. Journal of the Dow University of Health Sciences Karachi 7(3): 101-106.
- Watters WC, Baisden J, Gilbert TJ, Bono CM, Kreiner DS, et al. (2008) An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spondylolisthesis. Spine 8: 305-310.
- Roy-Camille, JY Lazennec, Ch Garreau, G Saillant (1998) Les spondylolisthesis L5-S1 A propos de 29 cas opérés par voie postérieure pure pour réduction et fixation. Rachis 3(2): 147-157.
- Elodie Cervantes (2016) Précision du vissage trans-isthmique sous guidage scanner et scopique : a propos de 50 cas. These d’exercice de Médecine Faculté de Médecine de Nice Le 8 avril.
- J Iba Ba, l Mwanyombet, D Nkoche, Y Assengone Zeh, PY Chouteau, et al. (2006) Traitement chirurgical du spondylolisthésis au gabon Neurochirurgie 52(4): 339-346.
- Benallel Noureddine (2015) Prise en charge chirurgicale du spondylolisthésis lombaire. Thèse de Médecine université Aboubekr Belkaid faculté de médecine le 11 juin.
- Agabegi SS, Fischgrund JS (2010) Contemporary management of isthmic spondylolisthesis: pediatric and adult. Spine J 10(6): 530-543.
- Steffee AD, Sitkowski DJ (1988) Posterior lumbar interbody fusion and plates. Clin Orthop Relat Res 227: 99-102.
- S Freppel, S Colnat-Coulbois, T Civit (2008) Traitement chirurgical du spondylolisthésis de l’adulte. Techniques chirurgicales - Orthopédie-Traumatologie, pp. 44-179.
- P guigui, E Ferrero (2017) Surgical treatement of degenerative spondylolisthesis. Orthop Traumatol Surg Res 103(1): 11-20.
- Endler P, Ekman P, Möller H, Gerdhem P (2017) Outcomes of Posterolateral Fusion with and without Instrumentation and of Interbody Fusion for Isthmic Spondylolisthesis: A Prospective Study. J Bone Joint Surg Am 99(9): 743-752.
- Ghosez JP (2002) Spondylolisthésis lombaire chez l’adulte. In: Conférences d’enseignement 2002. Cahiers d’enseignement de la SOFCOT n° Paris, Elsevier p. 1-20.
- Haefeli M, Elfering A (2006) Pain assessment. Eur Spine J Suppl 1: S17-S24.
- Omidi-Kashani F, Hassankhani EG, Shiravani R, Mirkazemi M (2016) Surgical Outcome of Reduction and Instrumented Fusion in Lumbar Degenerative Spondylolisthesis Iran J Med Sci January 41(1): 13-18.
- Farzad Omidi-Kashani, Ebrahim Ghayem Hassankhani, Reza Shiravani, and Masoud Mirkazemi, Surgical outcome of reduction and instrumented fusion in lumbar degenerative spondylolisthé Iran J Med Sci 41(1): 13–18.






























