Real Time Ultrasound Elastography in Musculoskeletal Manifestations of Mucopolysaccharidosis
Rosendo Ullot Font1, Pilar Rovira Martí1, Emilio J Inarejos Clemente2, Mar O’Callaghan Gordo3, Ramón Huguet Carol1 and Mercè Pineda Marfa3
1Department of Pediatric Orthopedics, Sant Joan de Déu Hospital, Spain
2Department of Radiology, Sant Joan de Déu Hospital, Spain
3Department of Neurology, Sant Joan de Déu Hospital, Spain
Submission: November 08, 2019;Published: November 26, 2019
*Corresponding author: Pilar Rovira Martí, Department of Pediatric Orthopedics, Sant Joan de Déu Hospital, Passeig de Sant Joan de Déu, 2. Esplugues de Llobregat. 08950, Barcelona, Spain
How to cite this article: Rosendo Ullot Font, Pilar Rovira Martí, Emilio J Inarejos Clemente, Mar O’Callaghan Gordo, Ramón Huguet Carol, Mercè Pineda Marfa. Real Time Ultrasound Elastography in Musculoskeletal Manifestations of Mucopolysaccharidosis. Ortho & Rheum Open Access J. 2019; 15(2):555908. DOI: 10.19080/OROAJ.2019.15.555908
Abstract
Background: Mucopolysaccharidosis (MPSs) are a group of metabolic disorders caused by several different enzyme deficiencies that cause multi-systemic affection.
Aim: The aim of this study was to assess the capability of ultrasound elastography (SE) in evaluating the tendons stiffness in patients with diagnosis of MPSs correlating with clinical and physical examination.
Method: We evaluated 15 patients affected of MPS during a year and a half (6 men and 9 women, median age of 10 years, range 3-39). General data such as the type of mucopolysaccharidosis, the enzymatic deficiency, storage product, genetic defect, treatments and general symptoms were recorded. Exhaustive orthopedic examination has been performed and orthopedic surgeries have been recorded. The functional exercise capacities were evaluated with the Six-Minute Walk Test. For Sanfilippo disease we used a disability scale that measures ambulation, behavior, speech, swallowing, and epilepsy with a score in each category. One paediatric radiologist with specific training in musculoskeletal disorders performed the ultrasound elastography examinations in all subjects.
Results: We have found echographic alterations in different locations of patients with mucopolysaccharidosis that correspond to what is found in the elastography.
Conclusion: The results of this work are promising as to the usefulness of elastography in the assessment of tissue stiffness in deposit diseases such as MPSs. Their greater sensitivity to detect deposits may be useful for us to evaluate the enzymatic treatments, the BMT or the surgical treatments that we perform to these patients. Level III of evidence
Keywords: Elastography; Mucopolysaccharidosis; Tendon stiffness; Ultrasound; Orthopedics
Abbrevations: Mucopolysaccharidosis (MPSs); Glycosaminoglycans (GAGs); 6-min walk test (6MWT); Replacement enzymatic treatment (ERT); Bone marrow transplant (BMT)
Introduction
Mucopolysaccharidosis (MPSs) are a group of inborn metabolic disorders caused by several different enzyme deficiencies that lead to progressive lysosomal storage of glycosaminoglycans (GAGs). MPS is a group of disorders with multi-systemic affection (nervous, skeletal, respiratory, cardiovascular, gastrointestinal, ocular, dental and auditory systems). They present slow clinical progression of the symptoms that may cause severe morbidity and early mortality depending on the molecular genetic mutation. A delay in the final diagnosis in some of these patients frequently occur, especially in those with more attenuated forms of disease.
MPSs were described in 1917 when Charles Hunter reported that two young male siblings presented similar characteristics, a large abdomen, and bone dysplasia. In 1919, Dr. Gertrud Hurler described the visceromegaly and bone abnormalities present in two unrelated boys with similar features [1]. In 1929, Luis Morquio described a form of “familial skeletal dystrophy” affecting four out of five children born to consanguineous parents [2]. In 1962, an attenuated form of hurler syndrome was described by Scheie et al. [3] and another form of mental retardation associated with mucopolysacchariduria, but with less pronounced visceral and skeletal manifestations, was identified by Sanfilippo et al. [4]. In 1963, Maroteaux et al. described a new form of dysostosis with mucopolysacchariduria, but without cognitive impairment [5]. In 1973, Sly syndrome was described and the most recent MPSs was described by Natowicz et al. in 1996 [6,7].
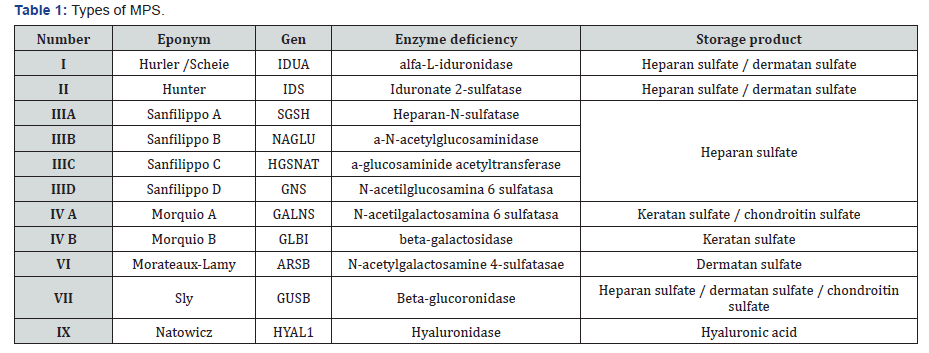
The seven major types of MPS are categorized based on the specific enzyme deficiency present, the major clinic manifestations or both [8]. All are progressive and autosomal recessive inheritance diseases, except MPS type II that is sexually inherited (X chromosome). Clinical features and severity of symptoms vary widely both among and within the seven major types of MPS Table 1. The accumulation of partially degraded GAGs in the lysosomes of connective tissue cells and chondrocytes is thought to be responsible for most of the musculoskeletal manifestation seen in the different types of MPS [9].
Ultrasonography is a useful imaging tool to characterize soft tissues, such as tendons, ligaments and synovial membranes [10] Recently, the ultrasound elastography has become commercially available for further assessment of tissues, in addition to the standard B-mode and Doppler imaging. The elastic properties of tissues are different from the acoustic impedance used to create B-mode imaging and the flow properties used within Doppler imaging, hence elastography provides a different form of tissue assessment and possibly showing pathology before it can be detected on B-mode imaging. This may be of particular use in the musculoskeletal system of the mucopolysaccharidosis patients [10].
The term elastography was described by Ophir et al. [11] as a method of portraying the strain properties of biological tissue. In medical usage, elastography requires the application of a mechanical stress to the tissues and then measurement of the displacement before and immediately after the stress as an estimate of the strain [12]. There are currently two main elastography methods in general clinical usage, namely compression/strain elastography and shear wave elastography.
Strain Elastography (SE)
In strain, or compression elastography, a force (i.e., stress) is applied from the transducer by repetitive manual pressure and the displacement (strain) is calculated from the return velocities of the tissues with respect to time. Motion intrinsic to the subject can also be used as the stress generator, such as aortic pulsation, however this is less useful in the musculoskeletal system where more superficial structures are of interest.
Measuring the displacement (strain) of the tissues secondary to an applied force (stress) gives a qualitative map of the elastic modulus distribution, termed an elastogram. This elastogram is colour coded and often superimposed on a greyscale B mode image for anatomical localization. True quantitative measures cannot be taken from this elastogram, as the applied force is unknown. A semiquantitative evaluation, however, can be determined from the ratio of the displacement of the tissue of interest and an adjacent structure, such as subcutaneous fat. Strain elastography has many potential disadvantages, including the variability in the pressure applied to the tissue. This can be partly compensated for by a graphical representation of the adequacy of the compression, however, the potential for interobserver and intraobserver variation remains [13].
Shear Wave Elastography
Shear wave elastography applies a vibration to tissues through a focused ultrasound pulse, generated by the transducer. This deposition of energy within the tissues creates transverse waves, or shear waves, which are perpendicular to the push pulse. The shear wave velocities can be measured from Doppler frequency modulation of simultaneously transmitted probing ultrasound waves. Young’s modulus can then be estimated as a function of the shear wave velocity. The stiffer the tissue is (the less compliant to shear forces), the faster the propagated shear waves within it. Although shear wave elastography is likely to be more reproducible than strain elastography owing to the standardized applied stress, it still has limitations. Shear waves are attenuated at depth and thus very deep tissues (> 9 cm from the skin) cannot be assessed. Axial-strain sonoelastography and share-wave elastography are relatively new, non-invasive, real-time techniques that evaluate the mechanical properties of tissues.
Materials and Methods
This study evaluated 15 patients affected of MPS of our hospital database (4 Hurler-Scheie (26’6%), 5 Sanfilippo (33,3%) [2 type A, 2 Type B, 1 Type C], 3 Morquio A (20%), 3 Maroteaux-Lamy (20%)) during a year and a half (6 men and 9 women, median age of 10 years, range 3-39). The hospital ethics board committee approved the study. Voluntary informed consent was obtained from all patients included in protocol. The patients’ characteristics were summarized with frequencies and percentages or as mean or median and range. General data such as the type of mucopolysaccharidosis, the enzymatic deficiency, storage product, genetic defect, treatments and general symptoms were recorded. Exhaustive orthopedic examination has been performed and orthopedic surgeries have been recorded.
Multiple values have been collected for orthopedic assessment, including height, body proportions, angular deviations, foot and hand alterations, deviations and affections in the vertebral column. Ambulation and joint stiffness or laxity have been assessed. The most frequent surgeries presented by patients with MPS have been collected. Recording the age and date of surgeries for carpal tunnel release, trigger finger release, hemiepiphysiodesis, hip and knee osteotomies and surgeries on the spine. The functional exercise capacities were evaluated with the Six-Minute Walk Test. For Sanfilippo disease we used a disability scale that measures ambulation, behavior, speech, swallowing, and epilepsy with a score in each category [14].
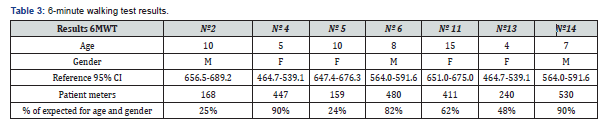
The 6-min walk test (6MWT) has gained importance in the assessment of functional exercise capacity in patients with chronic disease [15,16]. It has proved to be reliable, inexpensive, safe and easy to apply. In addition, it correlates well with important outcomes including death [17]. The 6MWTs were performed following ATS guidelines [18]. The evaluated parameters were six-minute walking distance in meters and changes in oxygen saturation and heart rate during exercise measured using a lightweight portable pulse oximeter. Pre-and post-6MWT dyspnoea were measured using the Borg scale [19].
One paediatric radiologist with specific training in musculoskeletal disorders performed the ultrasound elastography examinations in all subjects. The B-mode and elastographic images were shown simultaneously side by side on a split-screen display. Images in SE were performed by applying mild compression with the transducer. We used a scale (1-normal, 2-minimum deposit, 3-moderate deposit, 4-severe deposit) to be able to analyse the results in the 2 types of ultrasound. All patients included in the study undertook US of the lower limbs, evaluating the Achilles tendon, patellar tendon and anterior rectus and US of the upper limbs, evaluating the carpal tunnel and flexor tendons of all fingers. The statistical analysis was performed using the SPSS software package program (SPSS, Chicago, IL, USA) version 20. 0..
Results
Consanguinity was detected in 4 (26,6 %) patients of our study (1 Morquio, 2 Sanfilippo, 1 Hurler). From the clinical perspective we can distinguish three types of presentation according to the predominant affection: classical storage disease (MPS I, II, VI and VII), neurodegenerative disease (MPS I, II and III) and bone dysplasia (MPS IV). A short stature was detected in all patients except patients with Sanfilippo disease and in a patient with Hurler-Scheie disease, 3 years-old, who was in enzymatic treatment for more than 1 year. As regards the otorhinolaryngology alterations (otitis, deafness, adenoid and amygdalin hypertrophy), were found in all patients with Hurler- Scheie and Maroteaux-Lamy disease, two of five Sanfilippo and one of three Morquio. Corneal opacities were found in two of four Hurler/Scheie, two of three Morquio and two of three Maroteaux-Lamy. Cardiac valvopathy only was detected in one Morquio, one Maroteaux-Lamy and two Hurler-Scheie and hepatoesplenomegaly only was found in a Hurler-Scheie and in a Morquio disease. Neurological impairment was detected in all Sanfilippo patients.
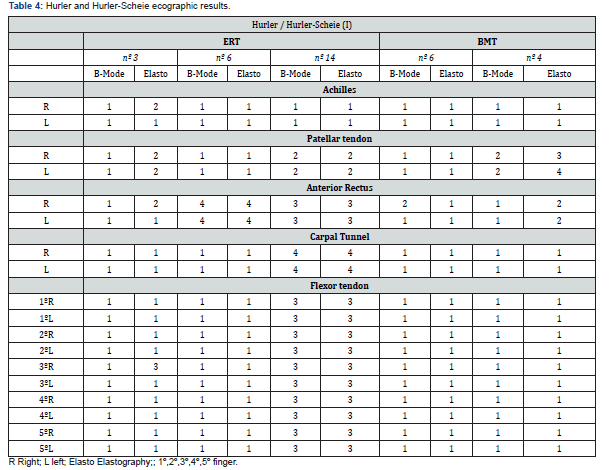
Bone marrow transplant (BMT) only was performed in two patients with MPS I (patient nº 4 and nº 6), patient number 6 had received replacement enzymatic treatment (ERT) with laronidase (Aldurazyme®) before the transplant. Patient 3 and 14 with MPS I had received the same ERT. All the patients with MPS VI (nº 5, nº 11, nº 12) were receiving ERT with galsulfase (Naglazyme®). Patient nº 1 and nº 2, with MPS IVA were treated with elosulfase alfa (Vimizim®) and patient nº 13 with the same diagnosis were pending to start the ERT. The patients with Sanfilippo disease didn’t have a replacement enzymatic treatment or bone marrow transplant.
An orthopedic assessment was made up of several items (short neck, short trunk, kyphoscoliosis, subluxation C1-C2, cervical myelopathy, cervical stenosis, platyspondylea, pectus carinatum, genu valgus, genu varum, coxa valga, acetabular dysplasia, femoral dysplasia, hip dislocation, flatfoot, clubfoot, clinical Madelung and ambulation). The patients with more orthopedic involvement were Morquio type and the least affected were Sanfilippo disease. In the 5 patients Sanfilippo we only found one flatfoot and one patient with coxa valga, four of five of these patients use wheelchair-bound and the average age of them was 33 years. Clumsiness were present in all Hurler-Scheie patients. In Morquio disease, one patient walked awkwardly, another had an assisted walk outside and the other was in a wheelchair. In the three patients with Maroteaux-Lamy, one patient walks awkwardly, another had an assisted walk outside and third was in a wheelchair for a cervical myelopathy. Patients with MPS IVA had joint laxity, hip dislocation and Madelung deformity didn’t found in the other types of MPS. Cervical myelopathy and C1- C2 subluxation were found in MPS IV and VI. Pectus carinatum was detected in MPS I and MPS IV. Genu valgus, short neck, short trunk, kyphoscoliosis, platyspondylea and acetabular dysplasia were diagnosed in all types of MPS analysed less Sanfilippo type.
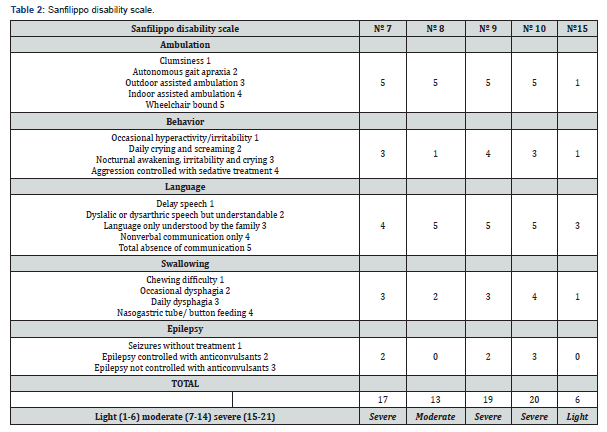
For Sanfilippo disease we used the Sanfilippo disability scale described by Delgadillo et al. [14] detailed in Table 2. There were three patients with severe disability, one moderate and one light. We present de results of the 6MWT and use the graphics of Geiger et al. [20] to compare it with normal population of same age and gender (Table 3). In the rest of the patients the test could not be performed because they could not walk. The surgeries performed in the patients were carpal tunnel release and trigger finger release in all patients with MPS I and in almost every MPS VI, knee hemiepiphysiodesis in 2/3 MPS IV and 1/3 MPS VI, a hip osteotomy in a patient with Morquio disease and in other patient with the same disease a knee osteotomy. All the patients with Maroteaux-Lamy required a cervical decompression and a patient with Morquio required an occipitocervical fusion.
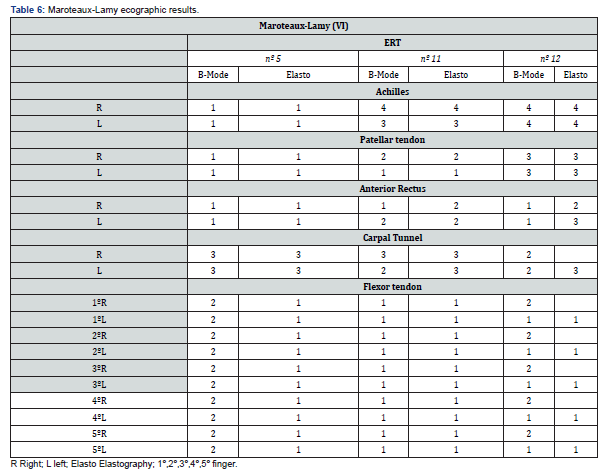
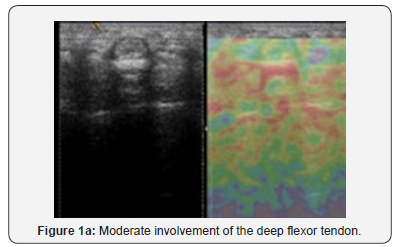
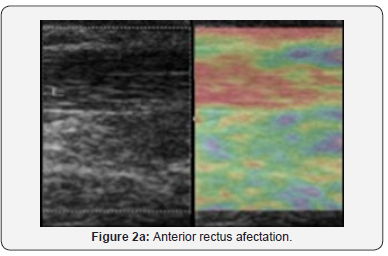
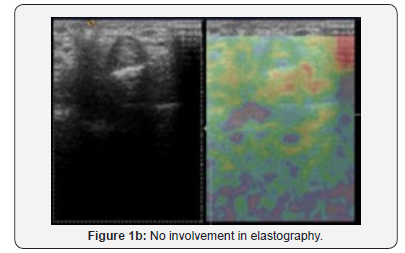
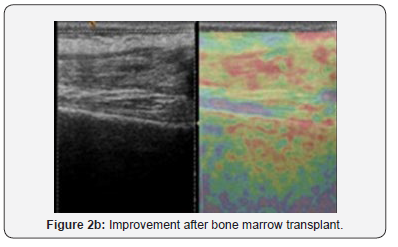
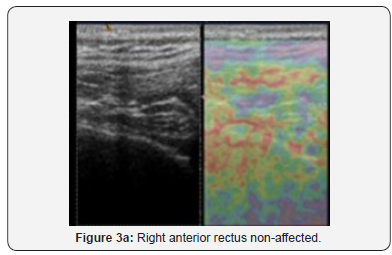
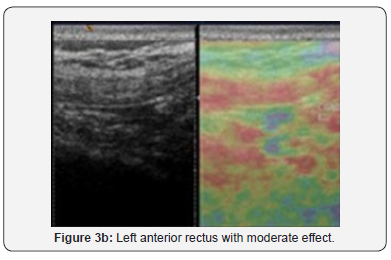
The results of ultrasonography have been represented in the following (tables 4-7), dividing patients by type of MPS and whether they have received treatment. Patient number 7 is a patient with MPS type IIIB of 35 years with a very severe musculoskeletal affection in which it was not possible to perform elastographs of all segments. In Figure 1 we can see how a B-mode without affectation can have two different representations with elastography. In the images, we can see different flexor tendons of the hand of the same patient with a Hurler’s disease. To the patient number 6 with Hurler mucopolysaccharidosis, an ultrasound was performed initially with ERT and after the BMT. In figure 2 we present the improvement in deposits in both b-mode and elastography after treatment. Figure 3 shows the different degree of involvement of the anterior rectus in the same patient.


Discussion
We found short stature in all patients with Morquio and Maroteaux-Lamy disease, and all but one patient with Hurler- Scheie disease of 3 years with ERT since 2 years-old. Short stature, may be due to a disruption in the programmed maturation of the chondrocyte at the level of the growth plate [21], is a common feature in all types of MPS, except in Sanfilippo disease where we did not find any short stature, although it may be mild or under-recognized in the attenuated forms. Axial growth is usually more affected than appendicular growth resulting in disproportionately short stature [22].
Joint stiffness and contractures can be found in all types of MPS, except for MPS IV (Morquio syndrome), in which there is laxity, and MPS IX [22]. We found laxity in all patients with Morquio. These abnormalities are felt to arise secondary to infiltration by GAGs of the ligaments, tendons, joint capsules and other soft tissues in combination with epiphyseal and metaphyseal deformities owing to defective skeletal remodeling [9]. Stiffness and contractures preferentially affect the phalangeal joints; however, all joints can be affected, especially in the more severe forms. When the interphalangeal joints of the hands are affected, the characteristic claw hand deformity develops; often resulting in impaired hand function. The hypermobility results from metaphyseal deformities, hypoplasia of bones and degradation of connective tissues around the joint.
The most frequent musculoskeletal procedures were carpal tunnel and flexor release that is performed very early age 5.9 years (3.2-9.5 years), hemiepiphysiodesis, osteotomies, and spinal cord decompression surgeries. Carpal tunnel syndrome is uncommon in childhood. The median nerve compression occurs as a result of thickening of the flexor retinaculum and the tissues around the tendon sheaths [23]. All patients with MPS I and MPS VI were operated on for carpal tunnel release and all but one for flexor release. Trigger fingers in association with carpal tunnel syndrome are well recognized in patients with MPS [9]. Trigger occurs as a result of GAGs deposits in the capsular tissues of joints or flexor tendons [24]. The diagnosis of a trigger digit is usually made clinically; however, there may be role for high-resolution ultrasonography in determining the underlying cause for triggering [25]. The patient nº14 with MPS I, was the most affected echographically and was pending a second release intervention.
Patients with MPS have an increased incidence of hypoplasia of the odontoid process that predisposes them to atlantoaxial instability. Spinal cord compression may occur as a result of atlanto-axial subluxation and lead to neurological complications, most commonly spastic tetra paresis; however, paraparesis and hemiparesis have also been reported [26]. Patients with Hurler syndrome (MPS I) and Morquio syndrome (MPS IV) appear to have the highest risk of developing odontoid hypoplasia, although it can occur in other types as well [27]. The combination of joint hypermobility of MPS IV and odontoid hypoplasia in these patients is the possible responsible for very high incidence of atlanto-axial subluxation. We found a cervical stenosis in a half of the patients of Hurler and subluxation C1- C2 and cervical myelopathy in Morquio and Maroteaux-Lamy. All MPS VI needed cervical decompression and one MPS IV needed an occipitocervical fusion.
We have found echographic alterations in different locations of patients with mucopolysaccharidosis that correspond to what is found in the elastography. One of the most affected was anterior rectus tendon. In MPS I, we found a patient with severe deposits on B-Mode and elastography that improve to normal/ minimum deposit after the bone marrow transplantation. Only one of four patients with MPS I had moderate/severe affectation of tendons (except Achilles tendon), this patient, however, had a 90% of the result in 6MWT for age and gender. In Morquio disease we found only minimum deposit in anterior rectus of 2/3 patients and moderate deposits in Achilles of 2/3 patients. Although the patient with Morquio were the least affected in b-mode and elastography, they had poor results in 6MWT (25% and 48% of expected for age and gender) and were the patient with greater orthopedic involvement. In Maroteaux- Lamy disease we found quite affectation in echographic findings. Achilles tendon was affected moderate/sever in 3/4 patients. All patients had minimum or moderate deposits in carpal tunnel and 2/3 in patellar tendon and anterior rectus tendon, the flexor tendons of the hand were less affected. Instead the patients with Maroteaux-Lamy disease with less echographic affectation had a bad result (24% of expected for age and gender) in 6MWT. In Sanfilippo disease we found minimum or moderate deposits in Achilles tendon in 3/4 patients and in patellar tendon 4/5. The anterior rectus tendon was the most affected and carpal tunnel and flexor tendons of the hands the least. The patient most affected was nº8 that had a moderate affectation in Sanfilippo disability scale.
The first effective therapy for these severe and progressive disease was reported in 1980, when BMT was performed on an MPS I patient [28]. The first specific therapy approved for MPS was intravenous ERT for MPS I, followed by MPS VI [29], MPS II, and, recently MPS IVA [1]. BMT can prevent cognitive decline, improve upper airway disease, reduce hepatosplenomegaly, and improve mobility in severe form of MPS I before the age of 2.5 years; however, the cornea is not cleared, cardiac valve disease persists and skeletal changes progress. BMT dos does not seem to be an option for patients with MPS III and MPS IV, and its efficacy is controversial for patients with MPS type II [1]. ERT has arisen as an effective approach to alleviate some of the symptoms of MPS I [30], MPS II [31], and MPS VI [32], and more recently, for MPS IVA [33]. Presently approved treatments are unable to appropriately address, such as the neurological and skeletal manifestations [1].
Currently, to confirm de efficacy of the enzyme replacement therapy for mucopolysaccharidosis, the 6-minute walk test (6MWT) is used. Faced with the need to find a biomarker that is objective and may evaluate the evolution of these diseases and the therapeutic responses we consider that the elastography in musculoskeletal could be a good method to follow-up response to different treatments that exist for these patients. Extensive research has demonstrated the effectiveness of the use of elastography in differentiating malignant from benign lesions of the breast, thyroid, prostate and lymph node [34-37].
Conclusion
In conclusion we found that the most affected tendon in elastography and B-mode was anterior rectus tendon. We found an improvement in elastography finding after a BMT in one patient in which we were able to perform the test before and after the transplant. Patient least affected in echography were patients with Morquio disease and they had joint laxity, they had poor results in 6MWT and were the patient with greater orthopedic involvement. We are aware that functional test like 6MWT encompasses more capabilities than just tendinous deposits, but we were hopeful that elastography can have a role, for their greater sensitivity, to detect deposits and may be useful for us to evaluate the enzymatic treatments, the BMT or the surgical treatments that we perform to these patients. The results of this work are promising as to the usefulness of elastography in the assessment of tissue stiffness in deposit diseases such as mucopolysaccharidosis. Also, its comparison in healthy population to be able to carry out its validation and to evaluate its usefulness in the follow-up of the disease. To be able to perform a work with scientific and statistical quality it is imperative to be able to quantify the values obtained by the elastography with an echograph with specific software for it.
Acknowledgement
Acknowledgements to Biomarin for their assistance in this study.
Conflict of Interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. “Informed consent was obtained from all individual participants included in the study.
References
- Wong JML, Khan T, Jayadev CS, Khan W, Johnstone D (2012) Anterior cruciate ligament rupture and osteoarthritis progression. Open Orthop J 6: 295-300.
- Noyes FR, Basset RW, Grood ES, Butler DL (1980) Arthroscopy in acute traumatic hemoarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Joint Surg 62(5): 687-695.
- Balkfors B (1982) The course of knee ligament injuries. Acta Orthop Scand 198: 1-99.
- Noyes FR, Barber-Westin SD, Hewett TE (2000) High tibial osteotomy and ligament reconstruction for varus angulated anterior cruciate ligament-deficient knees. Am J Sports Med 28(3): 282-296.
- Chang A, Hochberg M, Song J, Dunlop D, Chmiel JS, et al. (2010) Frequency of varus and valgus thrust and factors associated with thrust presence in persons with or at higher risk for knee osteoarthritis. Arthritis Rheum 62(5): 1403-1411.
- Boss A, Stutz G, Oursin C, Gächter A. et al. (1995): Anterior cruciate ligament reconstruction combined with valgus tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 3: 187-191.
- Markolf KL, Burchfield DM, Shapiro MM, Shepard MF, Finerman GA, et al. (1995): Combined knee loading states that generate anterior cruciate ligament forces. J Orthop Res 13(6): 930-935.
- Van de Pol GJ, Arnold MP, Verdonschot N, van Kampen A (2009): Varus alignment leads to increased forces in the anterior cruciate ligament. Am J Sports Med 37(3): 481-487.
- Kim SJ, Moon HK, Chun YM, Chang WH, Kim SG, et al. (2011) Is correctional osteotomy crucial in primary varus knees undergoing anterior cruciate ligament reconstruction? Clin Orthop Relat Res 469(5): 1421-1426.
- Jackson JP, Waugh W (1960) Tibial osteotomy for osteoarthritis of the knee. Proc R Soc Med 53(10): 888.
- Dejour H, Walch G, Deschamps G, P Chambat (1987) Arthrose du genou sur laxite chronique anterieure. Rev Chir Orthop Reparatrice Appar Mot 73: 157-170.
- Dejour H, Neyret P, Boileau P, Donell ST (1994): Anterior cruciate reconstruction combined with valgus tibial osteotomy. Clin Orthop Relat Res 299: 220-228.
- Webb JM, Salmon LJ, Leclerc E, Pinczewski LA, Roe JP (2013) Posterior tibial slope and further anterior cruciate ligament injuries in the anterior cruciate ligament-reconstructed patient. Am J Sports Med 41(12): 2800-2804.
- Giffin JR, Vogrin TM, Zantop T, Woo SL, Harner CD (2004) Effects of increasing tibial slope on the biomechanics of the knee. Am J Sports Med 32(2): 376-382.
- Luites JW, Brinkman JM, Wymenga AB, van Heerwaarden RJ et al. (2009) Fixation stability of opening versus closing wedge high tibial osteotomy: a randomized clinical trial using radiostereometry. J Bone Joint Surg Br 91(11): 1459-1465.






























