Sternum Tuberculosis Osteomyelitis in an Adolescent Patient: A Case Report and Review of Children’s Literature
Pinheiro Pedro Carlos1*, Correa Marilia Grizende1, Rosaman Fernando Colonna2, Fazecas Tatiana3, Fazecas Tatiana4 and Aymore Ierecê Lins5
1Orthopedic Department, Jesus Children’s Hospital, Brazil
2Oncological and Pathological Department, Jesus Children’s Hospital, Rio de Janeiro, Brazil
3Radiological Department, Jesus Children’s Hospital, Brazil
4Department of Radiology, National Institute of Orthopedic and Traumatology, Brazil
5Oncological and Pathological Department of National Institute of Orthopedic and Traumatology, Brazil
Submission: October 21, 2019;Published: November 01, 2019
*Corresponding author: Pinheiro Pedro Carlos, Orthopedic Department, Jesus Children’s Hospital, Brazil
How to cite this article: Pinheiro Pedro Carlos, Correa Marilia Grizende, Rosaman Fernando Colonna, Fazecas Tatiana, Fazecas Tatiana, Aymore Ierecê Lins. Sternum Tuberculosis Osteomyelitis in an Adolescent Patient: A Case Report and Review of Children’s Literature. Ortho & Rheum Open Access J. 2019; 15(2): 555906. DOI: 10.19080/OROAJ.2019.15.555906
Abstract
Sternum tuberculosis osteomyelitis in pediatric patients is an unusually exceptional disease. The few cases in the literature a great majority of these are from underdeveloped countries where tuberculosis is endemic. The disease, from other sites, occurs by hilar lymph nodes, hematogenous route or lymphatic dissemination may result. A rare case of secondary tuberculosis osteomyelitis of the sternum body is described. Diagnosis in our case thorough clinical history, radiography, ultrasonography, tomography or further alternative diagnostic techniques and histopathological studies was confirmed. The patient, with anti-tubercular treatment regimen (non-operative), had a successfully decisive response and has not suffered any recurrence during the years of follow-up. The purpose of this paper was to demonstrate the rare case of sternum tuberculosis osteomyelitis disease to pediatricians, pediatric orthopedic surgeons, radiologists, and infectious disease specialists. Previous diagnosis and immediate antibiotic regimens can significantly intensify patients’ outcomes.
History
Hindu writings mentioned the disease, signifying “consumption” (or destruction by virtue of body deterioration, by progression of body condition). Hippocrates (460-337 BC) popularized the word for tuberculosis phthisis in ancient Greek, which has numerous connotations including: “to consume”, “to spit”, and “to waste away” [1]. John Schoenlein (1793-1864) reported, in 1839, the term tuberculosis derived from the Latin word tubercula (the diminutive of tuber), which indicates a small lump [1]. Robert Koch (1882) a German physician, bacteriologist and researcher (1843-1910) had Mycobacterium tuberculosis isolated [1].
Vaughan (1918) an Austrian Pole male patient aged 26, bearing clinical aspects the of the appearance of a firm woody swelling in the middle of the sternum (flat bone); a distinctly cloudy, purulent fluid serum was noted. A “woody presternal phlegmon” due to an organism of low virulence was observed. The swelling was very hard, red and tender. The woody phlegmon was sent for microscopic examination. This was the first report of sternum tuberculosis in the literature credited [2].
Kremer and Wiese (1936) showed a picture of a young patient, with an anterior and superior swollen mass on the upper part of the sternum bone, with a fistulous lesion, diagnosed as sternum tuberculosis3. Olmos (1948) described two young patients with involvement of tuberculosis of the sternum. In the two cases, pulmonary lesions occurring before the age of 8 were presented [3,4].
Introduction
Tuberculosis (TB) continues as a multi-systemic worldwide infection unchanged in countries where it is endemic. Sternum TB in children is one of the incredibly uncommon sites for flat bone to be infected. Sternum incidence involvement constitutes approximately less than 1% of all cases of Mycobacterium tuberculosis osteomyelitis [5-9]. Only a limited number of articles of sternum TB in children’s literature have been reported [3,4,7-23]. In view of this, a representative case of sternum tuberculosis osteomyelitis in an immunocompetent adolescent male patient is described. A patient aged 15-year-10-month-old, with a cutaneous sinus formation over the anterior chest wall was ascertained on. The aim of this manuscript was to present an unusual case of tuberculous osteomyelitis of the sternum body area in a young patient with a secondary type (form) and multifocal sternum TB infection categorized23. The compelling diagnosis by image examinations and histopathology lesions of infected tissues was confirmed. An anti-tuberculous chemotherapy treatment consisting of rifampicin (RIF), isoniazid (INH), pyrazinamide (PZA) and ethambutol (EMB) was prescribed.
Case Presentation
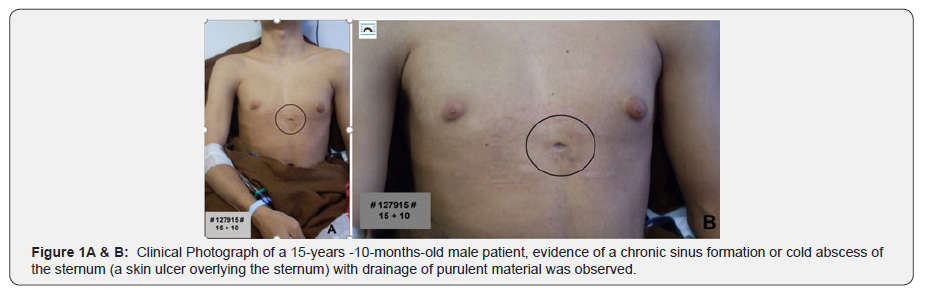
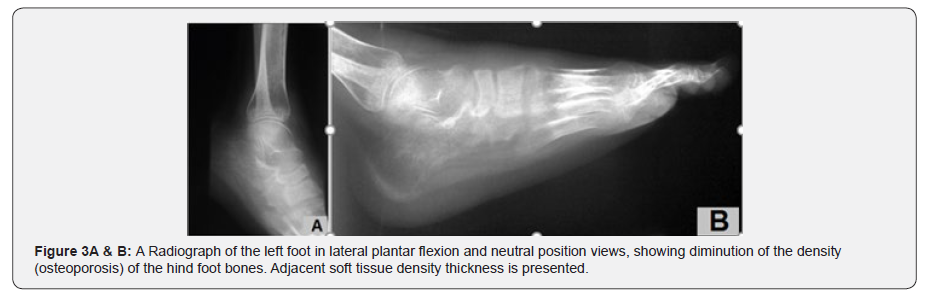
A 15-year -10-month-old male adolescent patient (PHFS) from a low socioeconomic level family, with foot symptoms, was admitted from another hospital. Careful clinical history revealed initial symptoms 4 months ago after trauma to his left ankle with cast immobilization plus treatment with antibiotics (oxacillin) for 32 days, without any benefit. Past medical history was collaborative, comprising a positive history of Bacillus-Calmette- Guérin (BCG) vaccination. At admission as an inpatient at our hospital, physical examination revealed tenderness on the left foot over the medial malleolus and a purulent secretion (abscess) fistulous lesion were detected. His gait needed auxiliary crutches in conformity with his difficulty of performing flexion-extension of the ankle joint, which was limited. In the thorax over the sternum flat bone an ulcer on the middle portion was evidenced. An open chronic sinus formation or cold abscess (a skin fistula overlying the bone) with drainage of purulent material was noted.
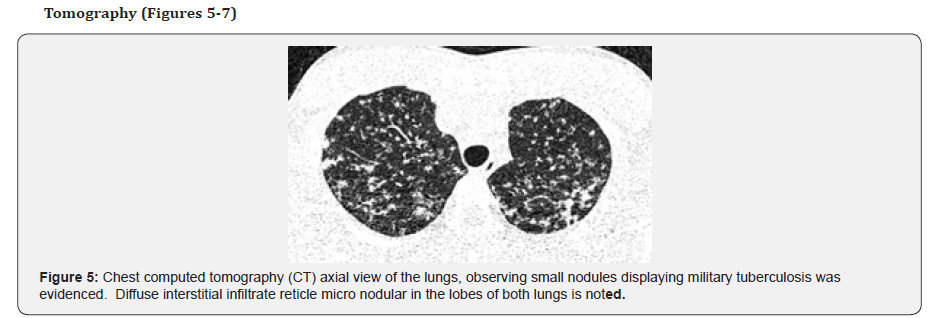
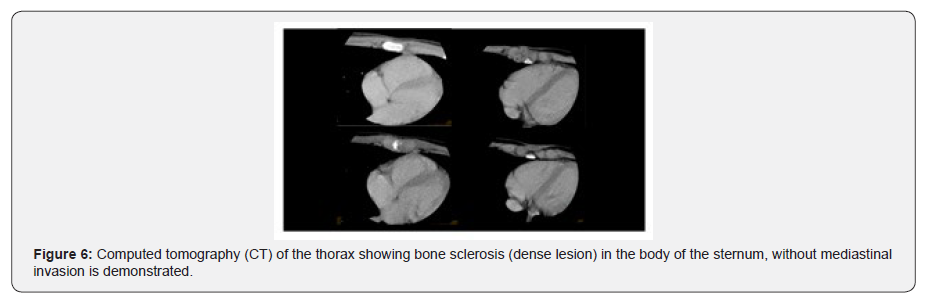
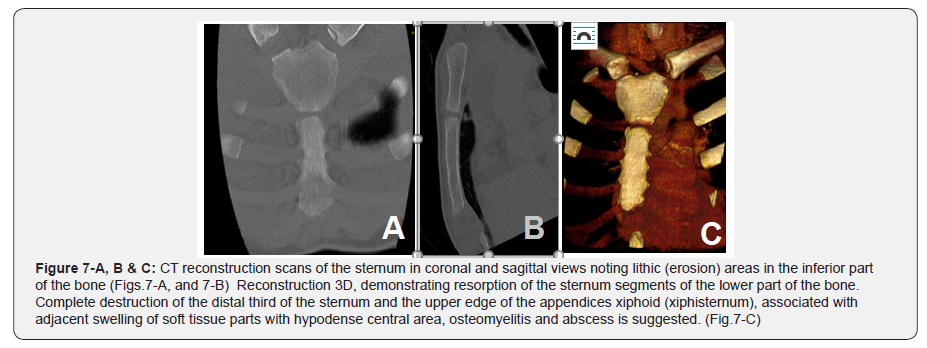
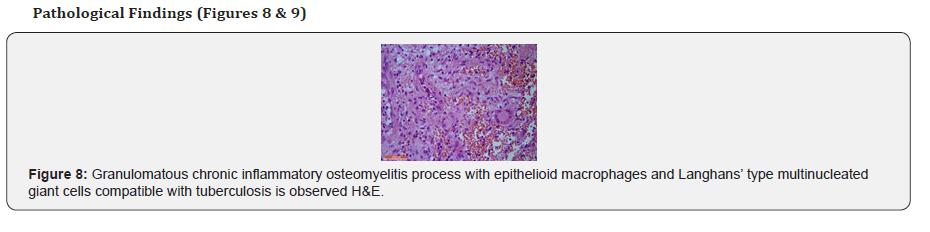
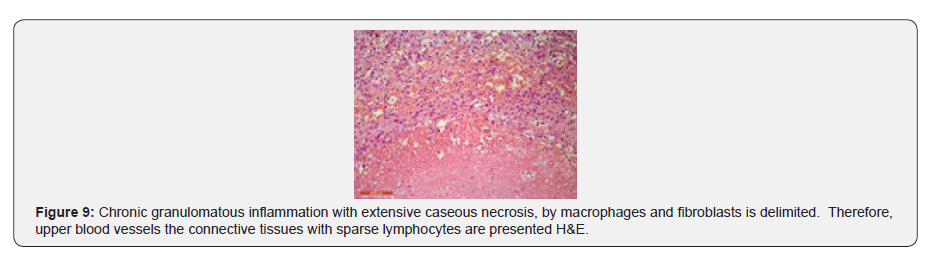
Following informed approval by the mother, a battery of investigations to confirm the diagnosis of tuberculosis was performed. Following informed consent, HIV testing method was requested. The laboratory complementary exams asked for blood count with erythrocyte sedimentation rate (ESR), anteroposterior and lateral chest radiographs as well as routine views for left ankle X-rays, ultrasonography and tomography of the chest were requested. Bone biopsies for microscopic examination of the ankle as well as of the sternum bone were required. On histopathological examination, granulomatous inflammation composing of epithelioid histiocytes, Langhans’ type giant cells and typical caseous necrosis were observed. Diagnosis of TB was corroborating upon the other histopathological macroscopic findings.
A standard four-drug regimen at our center, an antituberculous chemotherapy combination consisting of rifampicin (10mg/kg per day), isoniazid (10mg/kg per day), pyrazinamide (35mg/kg per day) and ethambutol (30mg/kg per day) for two months as an intensive phase patient was received. Subsequently for order seven months rifampicin (10mg/kg per day) and isoniazid (10mg/kg per day) following the national government’s (World Health Organization-WHO) guidelines were used. The patient was regularly followed by visiting the outpatient department at two-month intervals until the disease healed. The tuberculous lesions of the ankle and the sternum were completely relieved after four months of medications employed. The patient satisfactory response to treatment was demonstrated. During the follow-up period there have been no recurrences of the symptoms. Full treatment duration in our patient took nine months.
The authors present after six years clinical evaluations (photograph) of the patient (PHFS), aged 21-years-10-monthold, demonstrating, that a sinus over the sternum had healed.
Image Findings (Figure 1)s
Results
Laboratory Findings
Complete blood count has showed the following: red cells 5,560,000 per cubic millimeter (c.mm.), hemoglobin 12.8 gram%; hematocrit 40%; leukocytes count 7,100/mm3; basophils 0%; eosinophils 1%; mielocytes 0%; metamielocytes 0%; band cells 2%; segmentated 73%; lymphocytes 20%; monocytes 4%; plaquets were 375.000/mm3. Erythrocyte sedimentation (ERS) rate (Westergren method) was 44 mm of mercury after one hour, which was elevated; C-reactive protein (CRP) was positive (over 20,0 mg/dl); human immunodeficiency virus (HIV) testing was negative (nonreactive). Abnormalities in urinary findings were not evident. Purified protein derivative (PPD) was observed 11 mm (positive) 48 hours after administration.
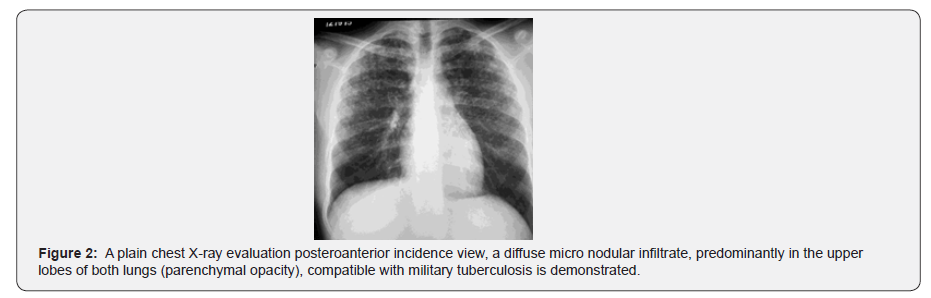
Roentgenographic Findings (Figures 2 & 3)


Discussion
In Brazil, bone tuberculosis is more common in children and corresponds to 10% to 20% of the extrapulmonary lesions in childhood [24]. Sternum tuberculosis osteomyelitis is a rare form of flat bone afflictions among pediatric populations such as in this case [20]. Sternum TB commonly occurs by reactivation of latent focuses formed throughout the course of hematogenous or lymphatic dissemination primary tuberculosis. Classically the disease is seen in young adults, although cases in children have been reported [11,16]. A few cases in countries where TB is endemic are described 16. Sternum TB in pediatric patients is uncommon in the literature; a small number of articles is reported [3,4,7,9-23]. Patients with pain and swelling in the sternum bone, tuberculosis should be considered [24,25].
Pinheiro reported a study of the records of a series of 94 child patients diagnosed with osteoarticular TB, with only one case of sternum TB observed [22]. McLellan reviewed 20 cases of sternum TB and only two cases to be from the pediatric age group found [25]. Khan et al. in his work about sternum TB, three cases in children were found [9]. Sternum TB osteomyelitis in children, comprises less than 1% of all skeletal TB cases [5- 9]. Shi-Min, predominantly in adult cases, from a total of 152 patients, 76 articles on the topic TB sternum infection have been reported. According to the pathogenesis sternum M. tuberculosis infections can be categorized into three types: primary, secondary and postoperative. He also ascribes into peristernal and multifocal in conformity with the extent of the lesions classified [23]. Our patient can be included into secondary and multifocal classification.
As stated, gender variable Shi-Min 64.9% males and 35.1% females were found [23]. Relating to young adults, males are more common than females affected [7]. According to our study in pediatric population sternum TB literature [3,4,7,9- 23], gender preferences were 72% males and 28% females. A significant gender difference between male and female pediatric sternum TB patients, among 18 articles [3,4,7,9-23,] at 68 patient’s studies was noted. Three patients’ genders were not determined 18. The gender percentage difference among the pediatric population, according sternum TB, is like that of adults. In conformity with variable age cases regarding sternum TB children, Kato et al. [11] and Aribas et al. [13] both authors in an infant 9 months of age at presentation was reported. An average age of pediatric with sternum TB, the literature [3,4,7,9- 23] an 8-year-4-month-old was described. In our patient, aged 15-years-10- months-old, above the average, was ascertained.
Esalatmanesh et al. [26] foot involvement accounts for less than 10% of cases of osteoarticular TB was described [26]. In our patient with sternum TB osteomyelitis the symptoms of an open draining on his left foot ankle was also observed. Alternative diagnostic techniques, Mantoux tuberculin skin test (purified protein derivative), radiographs, ultrasound and CT scans should be always included [23]. In our work, all variables mentioned above were followed. It is hard to understand making a final diagnosis without a histological examination of the sternum tissue [20,26]. It is mandatory, for diagnosis, to secure important histological samples to certify diagnosis and provide drug sensitivity data [18]. The gold standard for diagnosis of osseous tuberculosis comprises of histological examination verification.
A needle aspiration or excisional biopsy for histopathological diagnosis of sternum TB is obligatory [27]. Histopathology is the key suitable differential diagnosis to be confirmed18. In our case biopsy by an open excisional from the foot and the sternum bone has been done to ratify the diagnosis.
Treatment response depends on the stage when the disease was ascertained [28,29]. There is no consensus (empiric) on the optimal treatment of tuberculosis [21,30,31]. In our service, we follow World Health Organization (WHO) management for treating patients with active TB. Conservative treatment with competent antituberculous drugs in conformity with the research literature is the treatment of choice [3, 4,7,9- 23]. We have the opinion that standard anti-tuberculous chemotherapy (conservative management) is an enough procedure for obtaining good results. Adequate combinations with anti-tubercular drugs provide satisfactory results [17]. Treatment duration in our patient was 9 months based on RIF + INH + PZA + EMB for two months plus seven months according to RIF + INH was prescribed. Complications of sternum TB include ulcer overlying the sternum (fistula formation) [9], spontaneous fractures of sternum bone 9, tuberculous soft tissue mass (abscess) into the mediastinum16, secondary infection [29]. In our patient, a chronic sinus formation, with drainage of purulent material was noted.
Differential Diagnosis
Differential diagnosis of sternum bone lesions in children`s literature comprise: parasite infections7, actinomycosis [7,20,32] fungal diseases [7,20,32], sternum masses mimicking benign and malignant lesions [9] ,chest wall tumors in children [11], sarcoidosis [15,20] and acute osteomyelitis of the sternum bone [33].
Conclusion
In conclusion, in the case of any child patient with a nonhealing ulcer or abscess in the sternum bone, reliance on physicians involved with the musculoskeletal system (infection) tuberculosis disease should be kept in mind (Figure 11).

Acknowledgement
The authors wish to tank Paulo Vinicius Valladão Pinheiro, Angela Marta Marquini and Carlos Brown Scavarda for their review, advice, encouragement, and help in preparing the manuscript.
Ethical Approval
The procedures in this study involving human participants was in accordance with the ethical standards of the Institutional Jesus Children Hospital Rio de Janeiro, Brazil, and with the 1964 declaration of Helsinki (DoH) and its later amendments/ clarifications have been performed. This study with under protocol nº 172/11, CAAE (Presentation Certificate for Ethical Appreciation) number 0070.0.314.000-11, approved the Research about “Skeletal tuberculosis in children”.
Consent
Written informed consent from parents/guardians for publication of this report and accompanying images was obtained. Written consent on the patient´s chart registration number 73777 and 127915, Departments of orthopedic, and Radiologic Services of Jesus Children’s Hospital, Rio de Janeiro, Brazil is available.
Disclosure
None of the authors received payments or services, either directly or indirectly, i.e., via his or her institution of any aspect of this work. None of the authors, or their intuition(s), have had any financial relationship, prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this article. Also, no author has had any other relationships, or has engaged in any other activities, that could perceive to influence or have the potential to influence what is written in this work.
References
- Rubin SA (1995) Tuberculosis: captain of these men of death. Radiol Clin North Am 33(4): 619-639.
- Vaughn RT (1918) Acute osteomyelitis of the sternum: Woody Presternal Phlegmon: osteotomy and drainage. Surg Clin of Chicago 2(2): 253-262.
- Kremer W, Wiese O (1936) Tuberculosis de los huesos y articulaciones, Editorial Labor, S.A. Editorial Labor, S.A, Barcelona, Spain.
- V.S (1948) Skeletal Tuberculosis, The Williams & Wilkins Company. The Williams & Wilkins Company, Baltimore, United States.
- Boorugu HK, Chrispal A, Thomas EM (2009) Sternal tuberculous osteomyelitis presenting as a pulsatile swelling. Indian J Tuberc 56(3): 154-156.
- Saifudheen K, Anoop TM, Mini PN, Ramachandran M, Jabbar PK, et al. (2010) Primary tubercular osteomyelitis of the sternum. Int J Infect Dis;14(2): 164-166.
- Haynes W, Govender S (2000) Tuberculosis of the sternum in patients with infective spondylitis. SA Orthopaed J: 26-30.
- Singh S, Nagaraj C, Khare GN, Kumaraswamy V (2011) Multicentric tuberculosis at two rare sites in an immunocompetent adult. J Orthop Traumatol 12(4): 223-225.
- Khan SA, Varshney MK, Hasan AS, Kumar A, Trikha V (2007) Tuberculosis of the sternum: A clinical study. J Bone Joint Surg Br 89(6): 817-820.
- Ali WM, Beg MH, Rashid M, Zafar U, Abbas SN (2008) An experience with a rare diagnosis of isolated tuberculosis of sternum at JNMC Hospital, Aligarh, India. Saidi Med J 29(4): 580-593.
- Kato Y, Horikawa Y, Nishimura Y, Shimoda H, Shigeto E, et al. (2000) Sternal tuberculosis in a 9-month-old infant after BCG vaccination. Acta Paediatr 89(12): 1495-1497.
- Shah J, Patkar D, Parikh B, Parmar H, Varma R, et al. (2000) Tuberculosis of the sternum and clavicle: Imaging findings in 15 patients. Skeletal Radiol 29(8): 447-453.
- Aribas OK, Kanat F, Gomus N, Turk E (2002) Cold abscess of the chest wall as an unusual complication of BCG vaccination. Eur J Cardiothorac Surg 21(2): 352-354.
- Kuty S, Bennett D, Devitt A, Dowling FE (2002) Tuberculous osteomyelitis of the sternum in an infant: A case report and review of the literature. Pediatr Int 44:186-188.
- Tristano AG, Wilson M, López A, De Abreau F (2004) Sternal osteomyelitis caused by mycobacterium tuberculosis: Case report and review of the literature. Infect Dis Clin Pract 12: 174-177.
- Sharma S, Juneja M, Garg A (2005) Primary tubercular osteomyelitis of the sternum. Indian J Pediatr 72(8): 709-710.
- Thakker T, Prabhakar MM, Patel DA (2005) Tubercular osteomyelitis of sternum. Indian J Orthop 39(3): 179-181.
- Sandler DS, Al-Jibury M, Paton RW, Ormerod LP (2007) J Bone Joint Surg Br 89-B: 1379-81.
- Khaira A, Khaira DD, Gupta A, Bhowmik D, Kalra OP, et al. (2009) Tuberculosis of sternum: Three cases with different presentations. J Assoc Physicians India 57: 595-596.
- Mustafa G, Rubina, Sattar A, Ahmad UF, Asim M (2009) Sternal tuberculosis discharging through the skin: A rare presentation of disseminated tuberculosis. J Coll Physicians Surg Pak 19(5): 313-315.
- Narang M. Dwivedi A, Narang S, Mehrotra G (2011) Sternal tuberculosis: An uncommon presentation. J Case Rep 1: 9-11.
- Pinheiro PC (2014) Spectrum of skeletal tuberculosis in children. J Exerc Sports Orthop 1(2): 1-10.
- Shi-Min Y (2016) Sternal mycobacterial infections. Ann Thorac Med 11(2): 103-111.
- Guidelines for tuberculosis control in Brazil. Comitê Técnico Assessor do Programa Nacional de Controle da Tuberculose. Editora MS – OS 2011/0109 – Brasília – DF – Editora MS, 2011.
- McLellan DG, Philips KB, Corbett CE, Bronze MS (2000) Sternal osteomyelitis caused by Mycobacterium tuberculosis: case report and review of literature. Am J Med Sci 319(4): 250-254.
- Esalatmanesh K, Soleimani Z, Soleimani M (2008) Mycobacterium tuberculosis infection presenting with cutaneous abscess and osteomyelitis. Iran J Clin Infect Dis 3: 227-30.
- Vasa M, Ohikhuare C, Brickner L (2009) Primary sternal tuberculosis osteomyelitis: A case report and discussion. Can J Infect Dis Med Microbiol 20(4): 181-184.
- Gopal K, Raj A, Rajesh MR, Prabhu SK, Geothe J (2007) Seternal tuberculois after sternotomy for coronary artery bypass surgery: A case report and review of the literature. J Thorac Cardiovasc Surg 133(5): 1365-1366.
- Barbetakis N, Asteriou C, KleontasA, Karvelas C (2011) Primary sternal tuberculosis mimicking anterior chest wall tumor: Case report. Tuberk Toraks 59(2): 164-167.
- Singal R, Singh P, Mittal A, Gupta S, Singla S, et al. (2011) Primary sternal tuberculous ulcer with dissemination to the bone marrow: A clinical rarity. Ann Saudi Med 31(5): 542-545.
- Bajracharya S, Singh G, Singh M (2006) Primary tubercular osteomyelitis of the sternum: Report of two cases. Internet J Orthoped Surg 4.
- De Carli DM, Severo MD, Haygert CJP, Guollo M, Omairi A, et al. (2009) Sternal osteomyelitis caused by infection with Mycobacterim tuberculosis. J Bras Pneumol 35(7): 709-712.
- Drews H (1910) Die acute osteomyelitis des brustbeins (acute osteomyelitis of the sternum). Inaugural Dissertation.






























