Surgical Stabilization of the Extensor Tendon Dislocation in Non-Rheumatic Hand
Ricardo Monreal¹* and Giovanni Osinaga²
1Medica Vial Orthopedic Clinic, Alvaro Obregon No.151, Mexico City, Mexico
2Hospital Obrero No. 3, Caja Nacional de Salud, Department of Orthopaedics, Santa Cruz, Bolivia
Submission: August 05, 2019;Published: September 13, 2019
*Corresponding author: Ricardo Monreal, Medica Vial Orthopedic Clinic, Alvaro Obregon No.151, Mexico City, Mexico
How to cite this article: Ricardo Monreal, Giovanni Osinaga. Surgical Stabilization of the Extensor Tendon Dislocation in Non-Rheumatic Hand. Ortho & Rheum Open Access J 2019; 14(5): 555899. DOI: 10.19080/OROAJ.2019.14.555899
Abstract
Purpose: Treatment of traumatic sagittal band injury and subluxation of the extensor tendon at the metacarpophalangeal joint is often conservative but can also require surgical intervention if conservative treatment fails. A technique is presented using an extensor digitorum communis (EDC) tendon slip to stabilize the dislocated extensor tendon.
Methods: Nine patients (7 males and 2 females) with persistent pain and traumatic or spontaneous extensor tendon subluxations (> 6 weeks) in non-rheumatic hand underwent surgery.
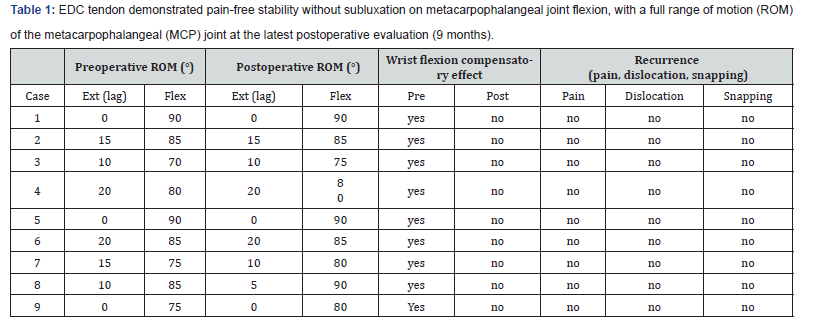
Results: In all patients the EDC tendon demonstrated pain-free stability without subluxation on metacarpophalangeal joint flexion, with a full range of motion (ROM) of the metacarpophalangeal (MCP) joint.
Conclusion: Restoration of sagittal band stability and extensor tendon centralization at the metacarpophalangeal joint by the extensor slip loop technique recreate the physiologic biomechanical forces.
Keywords: Sagittal band Extensor tendon subluxation, Reconstruction
Introduction
Different etiologies of extensor tendons dislocation of the hand (degenerative, traumatic, spontaneous and congenital) are mentioned although this condition is a is relatively uncommon in non-rheumatic hand [1,2].
Ulnar dislocation of the extensor tendon is the result of failure of the sagittal band to centralize the tendon, usually occurs in the middle finger because the radial component of the sagittal band is more prone to injury because they are thinner and longer than the ulnar fibers [3,4]. When dislocation of the extensor tendon is not treated in acute phase by closed methods, extensor tendon instability persists, and surgical treatment is indicated. A simple surgical technique is presented using an extensor digitorum communis (EDC) tendon slip to stabilize the dislocated extensor tendon.
Material and Methods
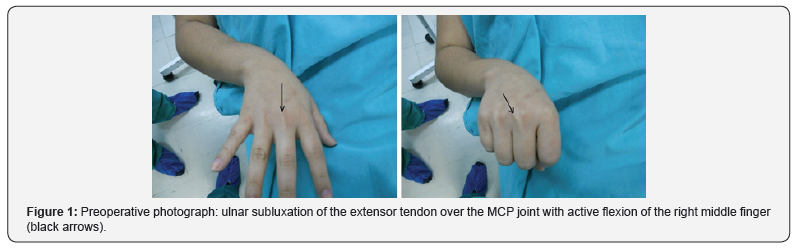
Nine patients (7 males and 2 females) with persistent pain and traumatic or spontaneous extensor tendon subluxations (> 6 weeks) in non-rheumatic hand (Figure 1) underwent surgery. Joint contracture and arthritic deformity were considered contraindications. The mean age was 28.6 years (range, 16-47 years). The middle finger was involved in all patients. The causesincluded traumatic subluxation (7 cases) and spontaneous subluxation (2 cases). The period from acute rupture of the sagittal bands and extensor tendon dislocation to surgery was a mean of 10.8 months (range, 3-18 months). Informed consent from the patients were obtained for this study. This study conforms to the Declaration of Helsinki.
Assessment of the Pre- and Postoperative findings
The involved finger was pre- and postoperatively evaluated on the basis of the symptoms including pain on metacarpophalangeal joint flexion associated with dislocation of the extensor tendon (Figure 1), and the range of motion (ROM) of the metacarpophalangeal (MCP) joint. The necessary range of motion (ROM) of the metacarpophalangeal (MCP) joints to maintain hand function are flexion ROM >70° with an extension ROM <30°of extension lag [5].
Surgical Technique [6]
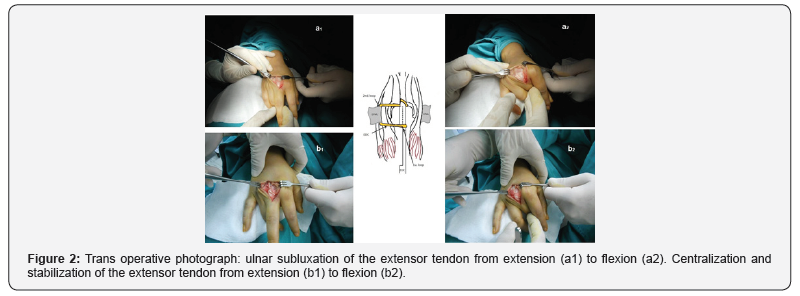
The ulnar dislocated extensor tendon is exposed using a dorsal 3-cm curved incision over the metacarpophalangeal joint. A distally based extensor digitorum communis (EDC) tendon strip 1/3 width on same side of tear is looped around the EDC to prevent migration of slip (1st. loop), passed under the deep transverse intermetacarpal ligament (DTML) on the radial side(2nd. loop) and woven back to into extensor hood /remaining EDC tendon and sutured after adjusting the tension. In the cases involving the index finger the tendon slip was passed under the radial lateral band instead of the deep transverse intermetacarpal ligament (Figure 2).
Postoperative Rehabilitation
After surgery, the arm is maintained with a short orthosis for 6 weeks with the metacarpophalangeal and proximal interphalangeal joints extended allowing active range of motion of the distal interphalangeal joint is allowed. When the shortarm orthosis is removed, the patient begins active motion of the metacarpophalangeal and proximal interphalangeal joints.
Results
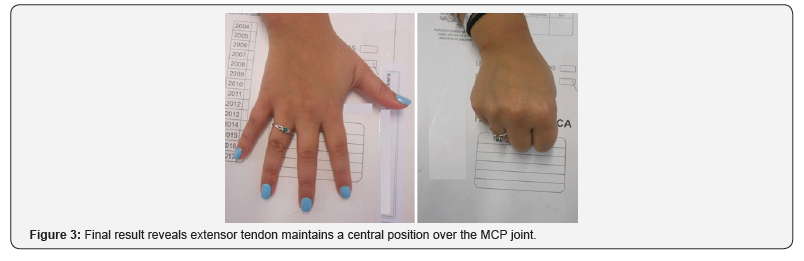
In all patients the EDC tendon demonstrated pain-free stability without subluxation on metacarpophalangeal joint flexion, with a full range of motion (ROM) of the metacarpophalangeal (MCP) joint at the latest postoperative evaluation (9 months) (Figure 3) (Table 1).
Discussion
ACL deficiency in the presence of varus alignment of the knee is not an uncommon finding. There is an ongoing debate on whether ACL reconstruction should be associated with correction of the varus deformity and if correction of the deformity is to be performed, should this be performed as sequential or a combined procedure? [6]. There is a direct relationship between varus malalignment and ACL tension 6. In one cadaveric study, it was noted that when knees were loaded in increasing degrees of varus, tensile forces increased in the ACL, and when the ACL was resected, the same knees demonstrated increasing lateral opening with increased stresses [7]. Therefore, it may be better for the success of ACL reconstruction and knee overall function to simultaneously correct the varus deformity. In this series, the combined procedure of anatomic ACL reconstruction and open wedge HTO were performed on patients who had both instability and symptomatic varus deformity with a satisfactory outcome for both instability and medial joint line pain. The success achieved in this series would help in establishing some criteria for patient selection. It is therefore essential to place the emphasis on the presence of symptomatic varus along with the instability symptoms and signs. Hence, individuals with asymptomatic primary varus deformities without widening of the lateral joint space may not be ideal candidates of this combined procedure [8- 10]. Previous reports suggested performing the combined ACL reconstruction along with correction of varus malalignment only in the presence of lateral thrust as it puts the reconstructed ACL under a high risk of failure [11]. It was also mentioned that varus malalignment in an ACL-deficient knee does not necessarily lead to a varus thrust, and therefore varus malalignment does not always require operative correction [8]. It could be argued that combining HTO with ACL reconstruction increases the surgical risk and may delay the rehabilitation process [9]. However, this was not observed in this series.
Acute sagittal band and/or ruptures can be successfully treated using closed methods but if extensor tendon instability persists surgical treatment is necessary. Although several surgical techniques have been described to achieve stability of the EDC tendon in chronic injury direct repair of the sagittal band may not be possible due to contracted remnant of the band within the scar tissue. Restoration of sagittal band stability and extensor tendon centralization at the metacarpophalangeal joint by the extensor slip loop technique recreate the physiologic biomechanical forces. This surgical technique presented is relatively simple, reduces the surgical time and only a single skin incision is necessary.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- McCoy FJ, Winsky AJ (1969) Lumbrical Loop Operation for Luxation of the Extensor Tendons of the Hand. Plast Reconst Surg 44(2): 142-146.
- Ovesen OC, Jensen EK, Bertheussen KJ (1987) Dislocation to Extensor Tendons of the Hand Caused by Focal Myoclonic Epilepsy. J Hand Surg 12(1): 131-132.
- Rayan GM, Murray D, Chung KW, Rohrer M (1997) The extensor retinacular system at the metacarpophalangeal joint. Anatomical and histological study. J Hand Surg 22(5): 585–590.
- Kettelkamp DB, Flatt AE, Moulds R (1971) Traumatic dislocation of the long-finger extensor tendon. A clinical, anatomical, and biomechanical study. J Bone Joint Surg Am 53(2): 229-240.
- Hiroyuki Hayashi, Hideki Shimizu, Shoji Okumura, Kazuhiro Miwa, et al. (2014) Necessary MCP ROM to maintain hand function. Hong Kong Journal of Occupational Therapy 24(2): 51-55.
- Watson HK, Weinzweig J, Guidera PM (1997) Sagittal band reconstruction. J Hand Surg 22(3): 452–456.
- Tubiana R, Valentin P (1964) The anatomy of the extensor apparatus of the fingers. Surg Clin North Am Aug 44: 897-906.
- Rayan GM, Murray D (1994) Classification and treatment of closed sagittal band injuries. J Hand Surg Am 19(4): 590-594.
- Kichouh M, Vanhoenacker F, Jager T, Van Roy P, Pouders C, et al. (2009) Functional anatomy of the dorsal hood or the hand: correlation of ultrasound and MR findings with cadaveric dissection. Eur Radiol 19(8): 1849-1856.
- Hakstian RW, Tubiana R (1967). Ulnar deviation of the fingers. The role of joint structure and function. J Bone Joint Surg Am 49(2): 299-316.
- Ishizuki M (1990) Traumatic and spontaneous dislocation of extensor tendon of the long finger. J Hand Surg Am 15(6): 967–972.






























