Percutaneous Medial Collateral Ligament R elease in Arthroscopic Medial Menisectomy in Knees with Tight Medial Compartment
Mohammed Alnahas*
Orthopedic Department, Faculty of Medicine, AL-Azhar University, Egypt
Submission: July 01, 2019;Published: July 24, 2019
*Corresponding author: Mohammed Alnahas, Orthopedic Department, Faculty of Medicine, AL-Azhar University, Nasr City, postal code: 11884 - Cairo - Egypt
How to cite this article: Mohammed Alnahas. Percutaneous Medial Collateral Ligament Release in Arthroscopic Medial Menisectomy in Knees with Tight Medial Compartment. Ortho & Rheum Open Access J. 2019; 14(4): 555891. DOI: 10.19080/OROAJ.2019.14.555891
Abstract
In tight knee joints with a narrow medial joint space, there is a risk of iatrogenic articular cartilage injury, even by an arthroscopy specialist which may predispose to osteoarthritis of the knee. The aim of the study was to detect if there is any residual knee laxity after the Pie- crusting technique or any other complications. Between February 2018 and April 2019, 30 patients with torn posterior horn of the medial meniscus were found to have tight knees with difficulty in visualization of the tear. The pie-crusting technique was done in those patients, which made the performance of partial menisectomy easy and safe. All the patients complained post-operative from pain over the site of the release (grade I MCL sprain) that has resolved within 1-2 weeks.
Keywords: Medial collateral ligament; Arthroscopic medial menisectomy; knee; Arthroscopy
Abbrevations: MCL: Medial Collateral Ligament; PHMM: Posterior Horn of Medial Meniscus
Introduction
The posterior horn of the medial meniscus is a common site of meniscal tears. Unrestricted arthroscopic visualization of the posterior horn of the medial meniscus is crucial to perform adequate menisectomy. In patients with tight knees, the medial femoral condyle makes the visualization of the posterior horn of the medial meniscus and the usage of instruments is very difficult. So, in tight knees, this area is reported to be one of the greatest sources of diagnostic errors in knee arthroscopy [1,2]. Vigorous manipulations with the instruments in cases with tight knees may cause iatrogenic chondral damage which may contribute to degeneration of the articular cartilage and osteoarthritis [3,4]. Also, this inadequate visualization may lead to insufficient menisectomy, with the left meniscal fragment might result in continued symptoms and reoperation [5,6]. Meniscal pathologies may be missed as a result of this inadequate visualization. Moreover, this vigorous manipulation to open the medial compartment, may result in rupture of the MCL or even fracture of the femur [7,8].
Agneskirchner & Lobenhoffer [3,9], Bosch [10], Park et al. [11] and later Fakioglu et al. [12] described a minimally invasive technique to open the medial compartment by puncturing the postero-medial capsulo-ligamentous structures percutaneously with the use of a needle. Although they reported that the injured structures healed uneventfully, there were no data on the injury localization, healing patterns or complications. In this study, we used the same technique as described by Fakioglu et al. [12] to enlarge the medial joint space in tight knees, which is, percutaneous puncturing of the postero-medial capsulo-ligamentous structures with the use of needles. Also, we were concerned about studying the possible complications especially residual medial laxity.
Materials and Methods
From February 2018 and April 2019, a prospective randomized analytical clinical study was done to evaluate the effect of percutaneous release of the superficial medial collateral ligament (pie-crusting technique) in patients with tight medial compartment of the knee undergoing partial menisectomy for torn posterior horn of the medial meniscus. The material of this study includes 30 patients with torn posterior horn of the medial meniscus with tight medial compartment of the knee. All patients were selected according the following criteria: Age: skeletally mature patients, patients with Torn PHMM with tight medial compartment without mal-alignment, no other ligamentous injuries, and no osteoarthritis or any other articular lesions. Twenty-six male patients and 4 female patients were included. Of the thirty patients, 20 patients had torn PHMM of the right knee
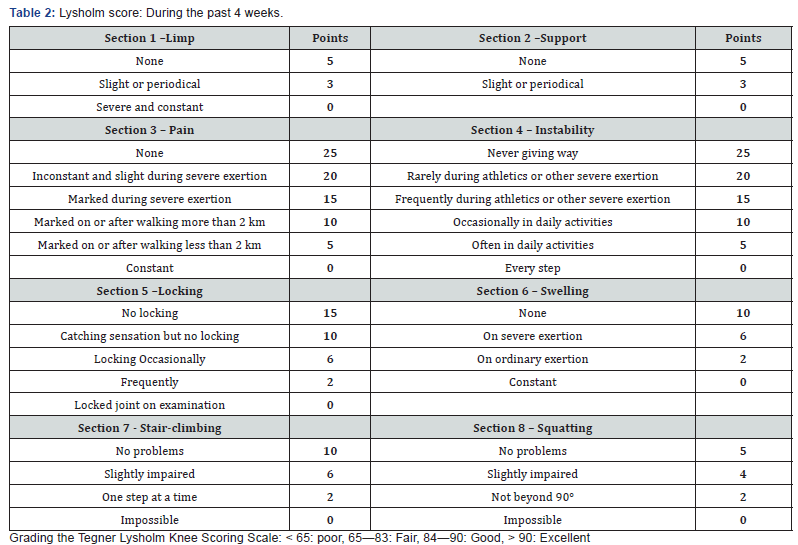
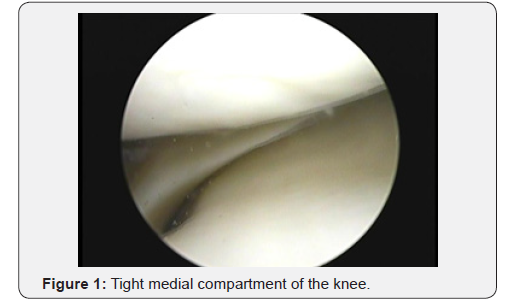
and 10 patients had torn PHMM of the left knee. In 16 patients the cause of the injury was sports practice, while in the other 14 patients the cause was non-sports injury. Table 1 Full clinical examination of the affected knee and the contra-lateral knee was done, and the patients scored according to Lysholm score (Table 2). All patients had poor results preoperative. Standard standing X- rays of both knee (AP, lateral views): To exclude osteoarthritis or mal-alignment. MRI of the affected knee was done to detect the site & type of the meniscal tear and to detect any other ligamentous injuries or patellar instability.
Surgical Technique
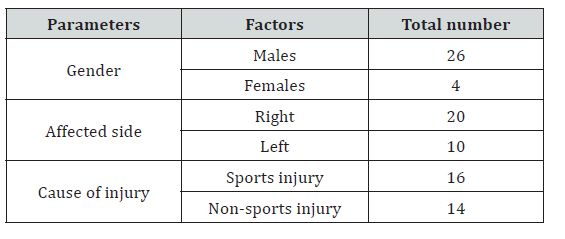
In this study, timing of surgery from the onset of symptoms was ranging from 1 month to 4 years. The patient was laid supine. A tourniquet over soft cotton is applied and elevated to 300 mmHg after administration of the anaesthesia. A flat or round, well padded, lateral post is positioned lateral to the tourniquet halfway up the thigh. Twenty-two patients received spinal anaesthesia, while the other 8 patients received general anaesthesia. Standard anterior-lateral and low anterior-medial portals were used with a 30° viewing scope. A fluid pump was used for inflow through arthroscopic sheath. Next a quick diagnostic knee examination was done starting with suprapatellar pouch, lateral gutter, and patello-femoral joint and medial gutter. Next, a probe was inserted through the anteriormedial working portal into the medial compartment. With the knee in extension to 30o flexion, valgus and external rotation was applied by the assistant to help better visualization of the PHMM. When complete visualization was difficult or instrumentation was difficult, the pie-crusting technique was done (Figure 1). When visualization or instrumentation of the posterior-medial meniscus under valgus stress was inadequate, controlled release of the posterior-medial capsulo-ligamentous structures with the metal inner shaft of the 16-gauge (G) syringe needle was performed. The targeted point for release was the posterior third of the superficial MCL proximal to the medial meniscus (Figure 2).
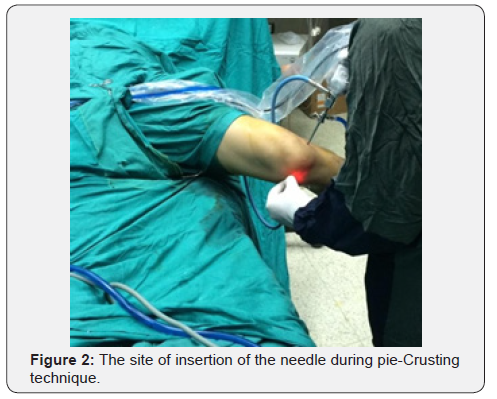
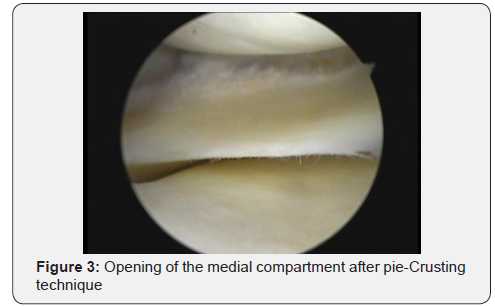
Puncture at this site produces a cracking sensation with a resultant opening in the medial compartment of the knee seen on the arthroscopy screen. If the opening in the medial compartment was enough on the monitor, then the release was stopped. Otherwise, without removing the needle from the skin, the posterior-medial capsulo-ligamentous structures were punctured again. In a more horizontal plane, while endeavoring to limit the punctures to the posterior part of the MCL, and the process was continued until the desired amount of opening of the medial compartment of the knee was reached (Figure 3). Better visualization of the footprint was obtained and subsequent partial medial menisectomy was done. Postoperative the patient was advised to use ice. No brace was used. Analgesics: ethidine 50-100 mg ampoule intramuscular was given when required for 2-3 days, Diclofenac sodium 50 mg. tablets twice daily for one week starting from the second day. Prophylactic antibiotics: Ceftriaxone IV. Weight bearing was encouraged from the second day post- operative whether with or without crutches as tolerated by the patient. Discharging the patient was after 24 hours post-operative.
Rehabilitation Protocol
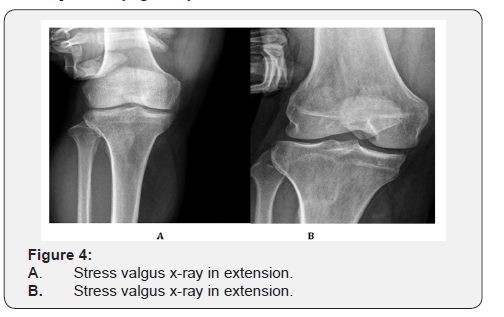
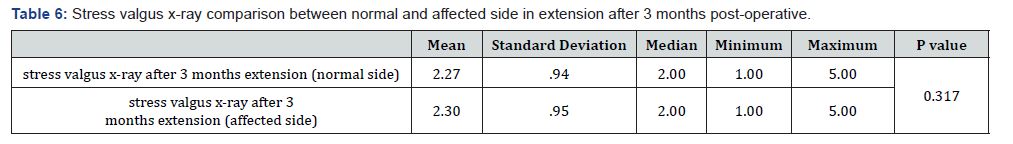
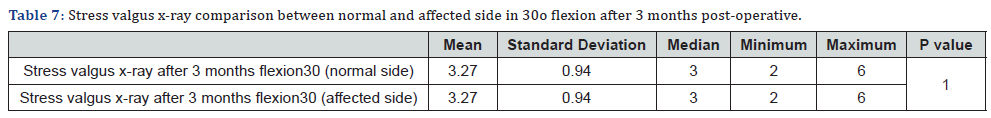
Active range of motion as tolerated. Weight bearing was allowed as tolerated. Isometric quadriceps contraction exercises. No squatting. No pivoting. Squatting is allowed gradually. Pivoting is allowed gradually. All patients were evaluated after surgery every two weeks up to the second postoperative month, then after one month. In this study the follow up period was 3 months. After assessment of the patients clinically and radiographically, the postoperative rating scales were recorded, and all data were documented 3 months post-operatively. Postoperative clinical evaluation was like the preoperative evaluation. In addition, the site of pie-crusting was examined for tenderness, swelling or ecchymosis. Stress valgus x-rays were done in full extension and 30° flexion after 3 months and the difference with the contralateral normal limb were documented. Medial joint space opening: The joint space width was measured as follows: A horizontal line (distal femoral line) was drawn tangent to the most distal portions of the femoral condyles. From this line, a perpendicular line was drawn to the most medial point of the medial plateau (Figure 4).
Results
Between February 2018 and April 2019, 30 patients were admitted to the department of Orthopedics and Traumatology in Al-Azhar University Hospital with torn posterior horn of the medial meniscus and intra-operatively they were found to have tight medial compartment. Considerable intra-operative chondral damage was expected on attempting to reach the posterior horn of the medial meniscus to perform partial menisectomy. In all the patients a partial menisectomy was performed with adequate visualization of the posterior horn of the medial meniscus and avoiding iatrogenic chondral injury. The duration of follow-up was 3 months. The results of the study at the end of the follow-up period were assessed both clinically and radiologically. Patients were evaluated using Lysholm score. In our study the median Lysholm score preoperatively was 49 (35-65). The median Lysholm score had increased at the end of the follow up period to 93 (86-98) with P value < 0.05 which was statistically significant (Tables 3-7).

Discussion
The posterior horn of the medial meniscus is still the single greatest source of errors in knee arthroscopy, despite the great advancement in arthroscopic techniques and instruments. Most errors occur in tight knees that have hidden lesions at the periphery of the posterior horn of the medial meniscus [1,2,13]. The posterior root attachment of the medial meniscus is critical for preserving important functions of the meniscus. Tears of the posterior root of the meniscus are clearly associated with major extrusion (>3 mm) of the medial meniscus, and meniscal extrusion appears to be associated with progression of osteoarthritis [11]. Resection of irreparable tears or repair of meniscal tears is associated with high success rate and minimal complications. In knee joints with a narrow medial joint space, there is a risk that cartilage may be damaged by the resection instruments, even by an arthroscopy specialist. Even superficial cartilaginous lesions due to hits or scratches caused by instruments and affecting the cartilage of the posterior femoral condyle and the tibial plateau do not heal with normal hyaline cartilage. They may predispose to osteoarthritis of the knee joint, especially if extensive partial menisectomy is performed simultaneously [10]. The superficial MCL is the primary stabilizer of the medial side of the knee. Biomechanical studies have shown that the highest strains in the MCL have been recorded in the posterior region of the ligament proximal to the joint line with the knee in extension during valgus loading [14,15]. Therefore, this area is thought to be the primary restraint to medial knee opening during valgus force in arthroscopy. In our study the targeted point for release was the posterior third of the superficial MCL proximal to the medial meniscus. This was done using a 16-gauge needle which was moved out-in.
Conclusion
Adequate visualization of the posterior horn of the medial meniscus is crucial for the performance of proper menisectomy. In cases with tight knees, the Pie-crusting technique is safe and efficient for visualization of the posterior horn of the medial meniscus. It allows the avoidance of causing iatrogenic chondral damage or fracture of the medial femoral condyle. The medial collateral ligament heals eventually in all patients after the Piecrusting technique without causing any subjective instability.
References
- Spahn G (2003) Arthroscopic revisions in failed meniscal surgery. Int Orthop 27(6): 378–381.
- Tolin BS, Sapega AA (1993): Arthroscopic visual field mapping at the periphery of the medial meniscus: a comparison of different portal approaches. Arthroscopy 9(3): 265–271.
- Agneskirchner JD, Lobenhoffer P (2004): Arthroscopic meniscus surgery: technical operative methods. Unfallchirurg, 107(9): 795–801.
- Buckwalter JA (2002) Articular cartilage injuries. Clin Orthop 402: 21–37.
- Ciliz D, Ciliz A, Elverici E, Sakman B, Yüksel E, (2008) Evaluation of postoperative menisci with MR arthrography and routine conventional MRI. Clin Imaging 32(3): 212–219.
- Nielsen DM, Twyman R (2005) Arthroscopic visualization of the posterior horn of the medial meniscus. Arthroscopy 21(10): 1272.
- Allum R (2002) Complications of arthroscopy of the knee. J Bone Joint Surg Br 84(7): 937–945.
- DeLee JC (1985) Complications of arthroscopy and arthroscopic surgery: results of national survey. Committee on Complications of AANA. Arthroscopy 1(4): 214–220.
- Agneskirchner JD, Bernard M, Lobenhoffer P (2005) Verbesserte Ubersicht bei arthroskopischen eingriffen am innenmeniskushinterhorn durch perkutanes needling des innenbandes. Artroskopie 20(7): 75–7.
- Bosch U (2002) Percutaneous perforation of the posteromedial capsuloligamentous structures to avoid cartilaginous damage due to arthroscopic intervention at the medial meniscal posterior horn in narrow joints. Oper Orthop Traumatol 18(5-6): 481–484.
- Park YS, Moon HK, Koh YG, Kim YC, Sim DS, et al. (2011) Arthroscopic pullout repair of posterior root tear of the medial meniscus: the anterior approach using medial collateral ligament pie-crusting release. Knee Surg Sports Traumatol Arthrosc 19(8): 1334-1336.
- Fakioglu O, Ozsoy MH, Ozdemir HM, Yigit H, Cavusoglu AT, et al. (2012): Percutaneous medial collateral ligament release in arthroscopic medial meniscectomy in tight knees. Knee Surg Sports Traumatol Arthrosc 20: 1417-1420.
- Boytim MJ, Smith JP, Fischer DA, Quick DC (1995): Arthroscopic posteromedial visualization of the knee. Clin Orthop 310: 82-86.
- Gardiner JC, Weiss JA, Rosenberg TD (2001): Strain in the human medial collateral ligament during valgus loading of the knee 391: 266-274.
- Gardiner JC, Weiss JA (2003) Subject-specific finite element analysis of the human medial collateral ligament during valgus knee loading. J Ortho Res 21(6): 1098-1106.






























