Increasing Indications of Treatment with Vitamin D, The Magic Hormone of Present Time
Picarelli G1,5*, Di Munno O2,5, Tarantino U3,5, Iolascon G4,5 and Migliore A1,5
1Fatebenefratelli Unit of Rheumatology, San Pietro Fatebenefratelli Hospital, Italy
2Rheumatology Unit, Department of Clinical and Experimental Medicine, University of Pisa, Italy
3Department of Orthopaedics, University of Rome Tor Vergata, Italy
4Department of Medical and Surgical Specialties and Dentistry, University of Campania “Luigi Vanvitelli”, Italy
5SI GUIDA member
Submission: July 03, 2019;Published: July 17, 2019
*Corresponding author: Giovanna Picarelli, Operative Unit of Rheumatology, San Pietro Fatebene fratelli Hospital, Italy
How to cite this article: Picarelli G, Di Munno O, Tarantino U, Iolascon G, Migliore A. Does the Post-Operative Infectious Risk increase in Patients Previously Treated with Intra-Articular Injections?. Ortho & Rheum Open Access J 2019; 14(3): 555889.. DOI: 10.19080/OROAJ.2019.14.555889
Abstract
Background: several systematic reviews have been conducted to study the relation between intra-articular injections and the associated risk of post-operative infection following arthroplasty. Despite the large use of intra-articular corticosteroids and hyaluronic acid injections in fact, there are no guidelines regarding the safety and timing of intra-articular drug administration related to the subsequent arthroplasty.
Questions/Purposes: the purpose of this study is to conduct a narrative review to report literature data about intra-articular corticosteroid or viscosupplementation and the risk for infection after arthroplasty.
Patients and Methods: full-length English articles up to August 2018 were included and identified through a literature research on PubMed using predefined text words related to the topic.
Results: 12 studies were analysed: patients had hip or knee steroid intra-articular injections before undergoing arthroplasty surgery. Eight of the studies were performed in patients with total hip arthroplasty and the other four were in patients with total knee arthroplasty. In each study we analysed the average time from injection to replacement and the types of steroids injected. Steroid injection had no significant effect on either deep or superficial infection rates of subsequent arthroplasty and only two of the analysed studies reported a significant increase in the incidence of deep infection in hip or knee replacement surgery following steroid injections.
Conclusion: This review reports that intra-articular steroid injections have no effect on deep infection rates of subsequent joint arthroplasty, suggesting that such practice is justifiable. Studies investigating the infectious risk of viscosupplementation prior to surgery are desirable.
Keywords: Intra-articular injections; Post-operative infection; Arthroplasty; Corticosteroids; Viscosupplementation
Introduction
Osteoarthritis (OA) is a leading cause of pain and disability worldwide. OA affects 240 million people globally and is becoming an increasing problem with the rates of total knee and hip arthroplasty rising globally. Intra-articular corticosteroid and viscosupplementation injections have become a widespread therapy in conservative management in the treatment of OA. Specifically, injections can be helpful in clinical practice for patients with initial or moderate OA and when end stage OA patients are not willing or able to undergo an arthroplasty in the short term. Regarding viscosupplementation, there is a lack of agreement between national and international guidelines on the use of intra-articular hyaluronic acid for medical management of symptomatic OA. However, results from randomized controlled trials and meta-analysis indicate that viscosupplementation offers the best benefit / risk ratio among various pharmacologic treatments to improve knee OA pain [1–5].
While different medical organizations, including the American Academy of Orthopaedic Surgeons [6], the American College of Rheumatology [7], the European League Against Rheumatism [8], and thle European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis [9], endorse corticosteroid injection for the handling of knee pain associated with OA, concerns exist about the timing of injections before undergoing a subsequent arthroplasty and a potential association with prosthetic joint infection in the peri-operative period [10–14]. Joint sepsis is considered the most serious complication of intra-articular corticosteroid injections. Research in literature has estimated that the risk of developing an infected joint following intra-articular corticosteroid injections is low, approximately 4.6 per 100,000 [15].
Periprosthetic joint infection is a devastating complication following knee or hip replacement leading to a significant increase in morbidity. A recent meta-analysis estimates the rate of surgical site infection to be 2.5% and the rate of deep periprosthetic joint infection to be 0.9% after arthroplasty [16].
Furthermore, it is important to identify the right sequence of conservative and surgical treatments for OA patients since it is also relevant from an economic point of view considering the high costs of the revisions.
Therefore, there is a debate about whether steroid injections increase the risk of post-operative infection following total knee arthroplasty [17–19]. Despite the widespread use of intra-articular corticosteroids and hyaluronic acid injections worldwide, there are currently no guidelines regarding safety and timing of intra-articular drug administration related to the subsequent arthroplasty. The purpose of this study is to conduct a narrative review to report literature data about intra-articular corticosteroid or viscosupplementation and the risk for infection after arthroplasty.
Discussion
Articles included in this narrative review were identified through a literature research on PubMed using predefined text words related to the operation (i.e. “total hip replacement” or “total knee replacement” or “hip arthroplasty” or “knee arthroplasty”), injection (e.g., “intra-articular” or “steroid” or “viscosupplementation”), infection (e.g., “infectious risk”) and a combination of these keywords. The search strategy was limited to studies conducted in humans, publications in English language and full-length articles published until August 2018.
Ten retrospective studies and 2 control cases were analysed (Table 1). The sample size ranged from 32 to 352 for patients and from 32 to 224 for control group, for a total number of 972 patients in the control group and 1213 in the experimental group. Patients had hip and knee steroid intra-articular injections before undergoing arthroplasty surgery. Eight of the studies were performed in patients with total hip arthroplasty and the other four were in patients with total knee arthroplasty. The average time from injection to replacement was between 0.5 and 50 months. We also extracted information, at least where available, about the types of steroid injected.
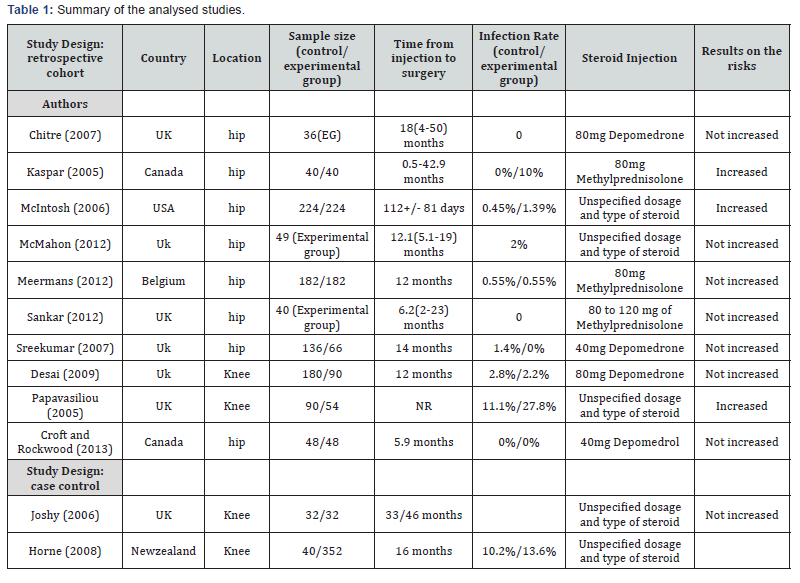
Joshy et al. [20] conducted a retrospective matched case control study. He compared a group of 32 patients who underwent knee arthroplasty complicated by infection with a control group of 32 patients with a past knee arthroplasty, selected from a database, who did not develop infection. An intra-articular steroid injection was performed in each group. The mean time between last steroid injection and arthroplasty was 46 months (range 12–121 months) in the infection group and 33 months (range 8–56 months) in the non-infected group. The results of the study showed no significant differences between the numbers of patients who received an intra-articular steroid injection in both groups. The authors concluded that steroid injection, performed before arthroplasty, was not a risk factor for post-operative infection. The small sample size of this study does not have much impact on the results.
Another retrospective case control study [21], with similar findings to those of Joshy et al. [20] compared 40 patients who developed post-operative infection within 6 months following total knee arthroplasty or who had revision surgery with 352 patients who underwent knee arthroplasty with no infection or wound healing problems. Patients completed a questionnaire asking if they had received knee infiltration before undergoing arthroplasty. The groups of non-responsive patients or deceased patients were removed and 28 infected cases and 219 patients who did not develop infection were selected. For all patients who received injections, the mean time of the last injection before arthroplasty was 16 months (range 1 month to 45 years). In the control group, it was determined that 32% of patients had received a steroid injection prior to surgery, compared with 39% in the infected group. The results demonstrated that prior steroid injection was not associated with a higher risk of postoperative infection.
To identify infected wounds, a follow-up of only 6 months was considered, thus excluding patients who developed infections later. Besides, risk factors such as smoking and diabetes mellitus, were self-reported by questionnaire. Even the execution of the steroid infiltration before knee arthroplasty was identified only through the questionnaire. Desai et al. [22] reported the outcome of 440 total knee arthroplasties with a 1 year follow-up. 90 knees in 80 patients were identified from hospital records as having had intra-articular steroid injections before undergoing total knee arthroplasty. A control group, where the patients were matched for age, sex and year of operation of 180 knees in 170 patients and did not undergo steroid injections, was used.
The results demonstrated that no cases of deep infection occurred in both groups. Two cases of superficial infection were found in the study group and five cases in the control group. For the two infected cases in the study group, steroid injections were given 18 months prior to surgery. Furthermore, 45 knees in the study group received an injection within the 12 months prior to surgery. It is difficult to identify significant differences between treatment and control groups due to the low infection rate reported in this study. However, it was observed that 60 out of 90 knees received steroid injections in the operating room under strict sterile conditions, which possibly contributed to the low infection rate in the study group. But this method of performing steroid injections is not common. Therefore, the findings of this study illustrated that giving a steroid injection before surgery is not a risk factor for infection and should not be extrapolated in the centres where aseptic techniques are less severe.
Chitre [23] analysed in retrospective all patients who had had steroid injection followed by hip arthroplasty over a 5-year period, with no case of deep joint sepsis reported. The average interval between injection and surgery was 18 months (range 4 to 50 months). Sankar et al. [24] also reviewed retrospectively 40 patients who had undergone hip arthroplasty after a steroid hip injection with an average interval from injection to joint replacement of 6.2 months. All patients during follow up did not develop deep infection. Meermans, et al. [25] evaluated 175 patients who underwent intra-articular steroid hip injections within one year before total hip arthroplasty to a control group. The authors reported no difference in superficial or deep infection between groups at average 71-month follow-ups. Sreekumar, et al. [26] compared 68 patients who had injections at an average of 14 months prior to total hip arthroplasty with a control group of 136 patients who underwent total hip arthroplasty and found no difference in post-operative infection.
Only a few studies showed that steroid injections prior to total knee arthroplasty may be associated with an increased incidence of post-operative infection. Papavasiliou et al. [13] showed a statistically higher deep infection rate in knee arthroplasty that had had a steroid injection prior to surgery as compared to those who were not given the injection. Three deep infections in the patients with previous steroid injection occurred whereas none developed in the control group. Deep infection, occurring within one year of surgery, was defined on the basis of certain characteristics (i.e. purulent drainage from the depths of the incision, microbiological culture from aseptically aspirated fluid, or pus cells present on microscopy, an abscess, local pain plus tenderness and patient temperature above 38 °C).
The time from the last injection to surgery for the three infected cases was eight, ten and eleven months respectively. The timing of injections for those patients who did not develop infection was not evaluated.
This study proved to be weak because no relationship between the number, dosage and timing of injections and risk of post-operative infection was established. Finally, these findings are not correlated to the general population because subjects with common risk factors such as diabetes mellitus, smoking and inflammatory arthritis were not included. It would have been more useful to include those risk factors to ensure that the control group was matched accordingly. Kaspar et al. [27] conducted a retrospective, matched, cohort study about infective complications after total hip arthroplasty, in 40 patients who had received an injection and 40 who had not. In the injection group there were five revisions, four of which were due to deep infection. There were no infections in the control group. Despite the moderate size of the study, complications in the injection group were very high with 30% having some form of sepsis of the hip, a rate which was four times higher than that of the control group.
Similarly to Kaspar, McIntosh [28] retrospectively compared 224 patients who underwent total hip arthroplasty implanted within 1 year of steroid injection with 224 patients in the control group. The authors reported hazard ratios of 3 for deep infection and 1.5 for superficial infection in patients who underwent total hip arthroplasty within one year of steroid injection. It should be kept in mind that certain sub-populations may be at risk of infection regardless of the injection, for example, very old patients and/or in multidrug therapy, diabetics, or patients in therapy with immunosuppressants. In these cases, routine preoperative precautions should take place including identification and optimization of recognized risk factors for post-operative infection, such as anemia, diabetes mellitus, smoking withdrawal, reduction or withdrawal of immunosuppressants. Besides, the different studies have used different types of steroids at different dosages with results that are not always comparable. The length of time that steroids remain active in the knee or in the hip is debatable. It has been hypothesised that steroid crystals do not fully dissolve into the joint but remain within the knee or the hip, and at the time of the surgery, the steroid crystals might be released. Furthermore, low-grade deep infection is often diagnosed after one year post surgery and therefore studies evaluating post-operative infection rates with a follow-up of only one year or less may underestimate the true infection rates.
The evaluation of the infectious risk of intra-articular steroid injections before arthroplasty was evaluated in several reviews while there is currently no data regarding the infectious risk of viscosupplementation, for hip and knee, on the subsequent surgery. Although numerous clinical trials have assessed the safety and efficacy of hyaluronic acid for the management of knee and hip OA, cumulative evidence leads to inconsistent interpretations. The most important finding of this review is that intra-articular steroid injection had no statistically significant effect on deep infection rates of subsequent joint arthroplasty, suggesting that such practice is justifiable. However, caution should be used before giving an intra-articular steroid injection. It is difficult to determine what is the best time from injection to subsequent surgery and there is no certain correlation with timing, dosage or frequency of injections. We may suggest, as a precautionary measure and while awaiting further study, avoiding the use of intra-articular steroids injected in the hip or in the knee for at least 3 months before surgery. Considering the lack of data, it is essential that good communication regarding the previous steroid treatment exists among general practitioners, rheumatologists and orthopedic surgeons when arthroplasty surgery is considered.
Conclusion
Several systematic reviews have been conducted to study the relationship between intra-articular corticosteroid and the increased risk for infection after arthroplasty. The pooled results of these reviews are still controversial and could not provide strong evidence; for this reason, we conducted a narrative review to report recent and updated literature data. Concerning the risk of infection, 12 studies looking at hip and knee arthroplasties were analyzed. These showed that steroid injection had no significant effect on either deep or superficial infection rates of subsequent arthroplasty. This narrative review suggests that intra-articular steroid injections prior to arthroplasty do not increase infection rates after surgery, however, further studies (i.e. high quality, prospective, multi centre RCTs) are still required to verify the safety of steroid injections given prior to the surgery. Furthermore, studies investigating the infectious risk of viscosupplementation prior to surgery are desirable.
Conflict of Interests
Each author certifies no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- Altman RD, Schemitsch E, Bedi A (2015) Assessment of Clinical Practice Guideline Methodology for the Treatment of Knee Osteoarthritis with Intra-Articular Hyaluronic Acid. Seminars in Arthritis and Rheumatism 45(2): 132–139.
- Bannuru RR, Schmid CH, Kent DM, Vaysbrot EE, Wong JB, et al. (2015) Comparative Effectiveness of Pharmacologic Interventions for Knee Osteoarthritis: A Systematic Review and Network Meta-Analysis. Annals of Internal Medicine 162(1): 46–54.
- Maheu E, Bannuru RR, Herrero-Beaumont G, Allali F, Bard H, et al. (2019) Why we Should Definitely Include Intra-Articular Hyaluronic Acid as a Therapeutic Option in the Management of Knee Osteoarthritis: Results of an Extensive Critical Literature Review. Semin Arthritis Rheum 48(4): 563-572.
- Maheu E, Rannou F, Reginster JY (2016) Efficacy and Safety of Hyaluronic Acid in the Management of Osteoarthritis: Evidence from Real-Life Setting Trials and Surveys. Semin Arthritis Rheum 45: S28-33.
- Trojian TH, Concoff AL, Joy SM, Hatzenbuehler JR, Saulsberry WJ, et al (2016) AMSSM Scientific Statement Concerning Viscosupplementation Injections for Knee Osteoarthritis: Importance for Individual Patient Outcomes. Clin J Sport Med 26(1): 1–11.
- Jevsevar DS, Brown GA, Jones DL, Matzkin EG, Manner PA, et al. (2013) The American Academy of Orthopaedic Surgeons Evidence-Based Guideline on: Treatment of Osteoarthritis of the Knee, 2nd The Journal of Bone and Joint Surgery. American Volume 95: 1885–1886.
- Hochberg MC, Altman RD, April KT, Benkhalti M, Guyatt G, et al. (2012) American College of Rheumatology 2012 Recommendations for the Use of Nonpharmacologic and Pharmacologic Therapies in Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care & Research 64(4): 465–474.
- Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, et al. (2003) EULAR Recommendations 2003: An Evidence Based Approach to the Management of Knee Osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis 62(12): 1145–1155.
- Bruyère O, Cooper C, Pelletier JP, Branco J, Luisa Brandi M, et al. (2014) An Algorithm Recommendation for the Management of Knee Osteoarthritis in Europe and Internationally: A Report from a Task Force of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Semin Arthritis Rheum 44(3): 253–263.
- Bedard NA, Pugely AJ, Elkins JM, Duchman KR, Westermann RW, et al. (2017) The John N. Insall Award: Do Intraarticular Injections Increase the Risk of Infection After TKA? Clinical Orthopaedics and Related Research 475(1): 45–52.
- Cancienne JM, Werner BC, Luetkemeyer LM, Browne JA (2015) Does Timing of Previous Intra-Articular Steroid Injection Affect the Post-Operative Rate of Infection in Total Knee Arthroplasty? J Arthroplasty 30(11): 1879–1882.
- Chambers AW, Lacy KW, Liow MHL, Manalo JPM, Freiberg AA, et al (2017) Multiple Hip Intra-Articular Steroid Injections Increase Risk of Periprosthetic Joint Infection Compared With Single Injections. J Arthroplasty 32(6): 1980–1983.
- Papavasiliou AV, Isaac DL, Marimuthu R, Skyrme A, Armitage A (2006) Infection in Knee Replacements after Previous Injection of Intra-Articular Steroid. J Bone Joint Surg Br 88(3): 321–323.
- Xing D, Yang Y, Ma X, Ma J, Ma B, et al. (2014) Dose Intraarticular Steroid Injection Increase the Rate of Infection in Subsequent Arthroplasty: Grading the Evidence through a Meta-Analysis. J Orthop Surg Res 9: 107.
- Pal B, Morris J (1999) Perceived Risks of Joint Infection Following Intra-Articular Corticosteroid Injections: A Survey of Rheumatologists. Clin Rheumatol 18(3): 264–265.
- Lindeque B, Hartman Z, Noshchenko A, Cruse M (2014) Infection after Primary Total Hip Arthroplasty. Orthopedics 37(4): 257–265.
- Dodd LE (2007) Infection in Knee Replacements after Previous Injection of Intra-Articular Steroid. J Bone Joint Surg Br 89(3): 422.
- Little NJ, Chipperfield A, Ricketts DM (2007) Infection in Knee Replacements after Previous Injection of Intra-Articular Steroid. J Bone Joint Surg Br 89(3): 423.
- Vashista GN (2007) Infection in Knee Replacements after Previous Injection of Intra-Articular Steroid. J Bone Joint Surg Br 89(3): 422–423.
- Joshy S, Thomas B, Gogi N, Modi A, Singh BK (2006) Effect of Intra-Articular Steroids on Deep Infections Following Total Knee Arthroplasty. Int Orthop 30(2): 91–93.
- Horne G, Devane P, Davidson A, Adams K, Purdie G (2008) The Influence of Steroid Injections on the Incidence of Infection Following Total Knee Arthroplasty. N Z Med J 121(1268): U2896.
- Desai A, Ramankutty S, Board T, Raut V (2009) Does Intraarticular Steroid Infiltration Increase the Rate of Infection in Subsequent Total Knee Replacements? The Knee 16(4): 262–264.
- Chitre AR, Fehily MJ, Bamford DJ (2007) Total Hip Replacement after Intra-Articular Injection of Local Anaesthetic and Steroid. J Bone Joint Surg Br 89(2): 166–168.
- Sankar B, Seneviratne S, Radha S, Rajeev A, Banaszkiewicz P (2012) Safety of Total Hip Replacement Following an Intra-Articular Steroid Hip Injection--an Audit. Acta Orthop Belg 78(2): 183–186.
- Meermans G, Corten K, Simon JP (2012) Is the Infection Rate in Primary THA Increased after Steroid Injection? Clin Orthop Relat Res 470(11): 3213–3219.
- Sreekumar R, Venkiteswaran R, Raut V (2007) Infection in Primary Hip Arthroplasty after Previous Steroid Infiltration. Int Orthop 31(1): 125–128.
- Kaspar S and de V de Beer J (2005) Infection in Hip Arthroplasty after Previous Injection of Steroid. J Bone Joint Surg Br 87(4): 454–457.
- McIntosh AL, Hanssen AD, Wenger DE, Osmon DR (2006) Recent Intraarticular Steroid Injection May Increase Infection Rates in Primary THA. Clin Orthop Relat Res 451: 50–54.






























