- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Complex Elbow Instability: What’s New in the Diagnosis, Classification and Principles of Surgical Treatment?
Giuseppe Giannicola1*, David Polimanti2, Marco Scacchi3, Gianlica Bullitta 4 and Stefano Gumina1
1Department of Anatomical, Histological, Forensic Medicine and Orthopedics Sciences, “Sapienza” University of Rome, Italy
2S Pertini Hospital Rome, Italy
3M G Vannini Figlie di S Camillo Hospital Rome, Italy
4Spaziani Hospital Frosinone, Italy
Submission: April 22, 2019;Published: May 03, 2019
*Corresponding author: Giuseppe Giannicola, Department of Anatomical, Histological, Forensic Medicine and Orthopedics Sciences, “Sapienza” University of Rome, Rome, Italy
How to cite this article: Giannicola G, Polimanti D, Scacchi M, Bullitta G, Gumina S. Complex Elbow Instability: What’s New in the Diagnosis, Classification and Principles of Surgical Treatment?. Ortho & Rheum Open Access J 2019; 14(1): 555879. DOI: 10.19080/OROAJ.2019.14.555879
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Abstract
Complex elbow instability represent a challenging injury even for expert elbow surgeons. Chronic instability, posttraumatic osteo-arthritis, stiffness and poor functional outcomes are frequent if these injuries are not adequately treated. A correct preoperative evaluation includes X-rays, CT scan with 2D and 3D reconstruction and stability tests under fluoroscopy in order to recognize all osseous and ligamentous lesions. The most common patterns of complex elbow instability includes: (1) radial head fractures associated with lateral and medial collateral ligaments lesions; (2) coronoid fractures and lateral collateral ligament lesion; (3) Terrible Triad; (4) fracture-dislocations of the proximal ulna and radius, also referred to as transolecranon fracture-dislocations and Monteggia-like lesions; and (5) humeral shear fractures associated with lateral and medial collateral ligament lesions.
The main goals of the treatment are (1) to perform a stable osteosynthesis of all fractures, (2) to obtain concentric and stable reduction of the elbow throught the repair of soft tissue constraint lesions and (3) to allow early motion. All the patterns of complex elbow instability share the same therapeutic algorithm based on seven main principles: 1) the proximal ulna must be anatomically reduced and fixed; 2) the radial head or humeral shear fracture must be repaired or replaced, 3) bone length, alignment and rotation of ulnar and radial shaft fractures must be recovered; 4) the lateral collateral ligament complex must be repaired to obtain elbow stability; 5) the medial collateral ligament must be repaired if persistent instability is observed after lateral collateral ligament repair; 6) an hinged external fixator must be considered if the elbow remains unstable or the protection of the joint reconstruction is required; 7) re-evaluation of the surgical steps if congruent ulno-humeral and radio-humeral joints have not been achieved. Following the surgical treatment an adequate rehabilitation programme should be started promptly and continued for at least 6 months since a significant improvement of the range of motion occurs prevalently in this period, which should be considered the critical time period to obtain a functional elbow.
Keywords: Instability; elbow; Complex elbow instability; Terrible triad; Monteggia fracture-dislocation; Transolecranon fractures; Coronoid fractures; Radial head fractures; Humeral shear fractures; Elbow ligaments
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Introduction
Complex elbow instability (CEI) is caused by osteo-articular fractures combined with capsule-ligament tears and muscle-tendinous lesions, which result in a loss of elbow stability. These injuries, which pose a challenge even to expert orthopaedic surgeons, still yield unsatisfactory results in 33-44% of patients, and require revision surgery in 26-55% of patients [1-8]. The stability of the elbow joint is achieved by means of the primary stabilizer structures, which include bony constraints (i.e. coronoid and olecranon processes and humeral trochlea) as well as soft tissue constraints (i.e. lat¬eral and medial collateral ligaments), whose contribution to elbow stability is comparable [9-16]. In general, elbow instability occurs when two, or more, of these anatomical structures are damaged. The degree of instability, as well as the complexity of the surgical treatment, may be even greater when associated injuries of the secondary elbow stabilizers (e.g. radiocapitellar joint, anterior and posterior joint capsule, muscle-tendinous units) occur [13,15,17-20].
Acute instability of the elbow may be either simple or complex: simple instability comprises a purely soft tissue constraint lesion that results in dislocation; complex instability is associated with a combination of bone and soft tissue constraint injuries, and may consequently also be defined as a fracture-dislocation of the elbow. The aim of this review is to describe what is new in the diagnosis and treatment of complex elbow instability.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Diagnosis
CEI is normally associated with low-energy trauma. The most common mechanism causing an elbow fracture-dislocation is a fall on an outstretched hand or direct trauma at the elbow. Severe elbow pain, ecchymosis, swelling and deformity are usually present. The clinical examination should include the ipsilateral wrist and shoulder joints since concomitant injuries occur in nearly 20% of patients [21]. A thorough neurovascular examination is warranted before and after closed reduction, even though neurovascular injuries are unlikely to occur in low-energy traumas. Two-dimensional X-ray images (anteroposterior and lateral view) should be taken both before and after repositioning maneuvers. Complex elbow instability may be evident radiographically when complete elbow dislocation occurs. However, since instability often also occurs without dislocation or with slight joint malalignment on the coronal or sagittal planes, the complexity of the injury may easily be underestimated. The injury in such cases is likely to be treated inappropriately, and ultimately yield poor results [5,7,8,22,23].
A computed tomography scan with 2- or 3-D reconstructions is thus mandatory in all cases to evaluate the extension and severity of bone injuries; a fluoroscopy examination is instead essential for the assessment of soft tissue constraints. The severity of ligament lesions and residual elbow stability are usually evaluated shortly before surgery. With the patient’s arm positioned under the radiograph intensifier, the ability to maintain concentric reduction during flexion-extension in varying degrees of forearm rotation should be assessed; elbow joints also need to be examined during valgus and varus stress tests at flexion angles of 0°-30° to assess medial collateral ligament (MCL) and lateral collateral ligament (LCL) function, respectively; the pivot-shift test may also shed relevant information on LCL function. Moreover, fluoroscopy also allows the evaluation of the distal radio-ulnar joint and interosseous membrane. MRI is rarely indicated in CEI. A number of CEI patterns have been identified in recent decades. CEI currently includes the following fracture-dislocations: (1) radial head fractures associated with LCL and MCL lesions; (2) coronoid fractures with a LCL lesion; (3) terrible triad; (4) fracturedislocations of the proximal ulna and radius, also referred to as transolecranon fracture-dislocations and Monteggia-like lesions; (5) humeral shear fractures associated with LCL and MCL lesions.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
General Principles of Treatment
CEI presents with a range of clinical and radiographic patterns. However, since the principles and the surgical steps involved in the treatment of these injuries are shared, a single therapeutic algorithm can be defined. We have identified a “rule of seven principles”, which has the following aims:
I. To restore the main joint of the elbow, i.e. the ulnohumeral joint. This is achieved by performing an anatomical reduction and stable osteosynthesis of the coronoid and olecranon fractures.
II. The radio-humeral joint must be preserved given its role as a secondary stabilizer of the elbow; radial head or humeral shear fractures should be fixed or replaced, particularly if the ulno-humeral joint and medial collateral ligament have been damaged; resection of the radial head is rarely recommended in CEI.
III. Attention should be paid to the recovery of bone length, alignment and rotation in cases of ulnar and radial shaft fractures so as to fully restore the forearm functions, particularly rotations.
IV. The LCL complex must be repaired in all cases following osteosynthesis of fractures to ensure recovery of elbow stability. Intraoperative testing under fluoroscopy should reveal a stable and congruent elbow.
V. The MCL must be repaired if persistent instability is observed after LCL repair, as well as in cases in which the medial compartment has been exposed for other reasons (e.g. coronoid osteosynthesis).
VI. A hinged external fixator (HEF) should be applied if elbow instability persists after MCL repair or when osteosynthesis is unstable or ligament reconstruction is tenuous. This device allows the elbow to be mobilized early, ensures ligament healing in physiological tension and protects the osteosynthesis [24,25].
VII. Every surgical step should be re-evaluated if congruent ulno-humeral and radio-humeral joints have not been achieved by the end of the surgical procedures.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Complex elbow Instability Patterns
Radial Head Fractures with Associated Lateral and Medial Collateral Ligament Lesions
Radial head fractures (RHF), which are the most frequent bone elbow injury in adults, account for approximately 33% of all elbow fractures [26]; it is important to bear in mind that isolated displaced fractures occur in fewer than 5% of patients, while concomitant injuries, including other fractures, elbow dislocation or collateral ligament tears, occur in the remaining 95% of cases [27,28]. RHF associated with ligament lesions are common and usually result from a combination of valgus and axial loads being placed on an elbow joint that is supinated and extended (i.e. posterolateral rotatory instability). The surgeon should suspect associated ligament lesions, above all in displaced and comminuted fractures (Mason II-III type).
The Mason-Hotchkiss classification [29] is useful when planning surgery of RHF, even in CEI. Type I fractures are defined as non-displaced fractures or as minimally displaced marginal lip fractures (<2 mm displacement) that do not prevent motion and can be treated nonoperatively. Type II fractures (partial head) are displaced fractures (usually >2 mm) that may be associated with a mechanical block that prevents motion or are incongruent but not severely comminuted. Type II fractures can often be treated by means of open reduction and internal fixation (ORIF). Lastly, type III fractures (whole head) are comminuted fractures that cannot be repaired and thus need to be treated by means of radial head arthroplasty (RHA). Osteosynthesis in this type of fracture tends to be complicated and may require mini-plates.
In spite of the numerous clinical studies and advances in technology, controversy surrounds the indications for ORIF as opposed to conservative treatment in some fractures in which displacement is slight. A recent biomechanical study showed that RHF that are depressed 2 mm or angulated 30° may result in an 80% loss of the concavity-compression stability of the radiocapitellar joint; the anatomical repair of such fractures may therefore be considered to prevent elbow instability [30]. Disagreement also exists regarding the indications for ORIF versus RHA for comminuted fractures. The current indications for RHA are: 1) comminuted fractures that involve the whole head in which reduction and stable fixation cannot be satisfactorily achieved, 2) partial head fractures that involve over 30% of the articular rim of the radial head that cannot be reconstructed, and 3) fractures consisting of more than 3 fragments [31].
While Al Burdeni et al. [32] stated that there is no significant difference between RHA and ORIF to treat pluri-fragmentary and comminuted fractures, other authors believe that RHA is a more reliable surgical solution in such fractures, especially in patients over 65 years of age [33-35]. Osteosynthesis of partial head fractures can be performed through a lateral approach using mini-fragment screws or headless screws, while precontoured mini-plates can be used when the fracture involves the whole radial neck and greater stability is required; in such cases, the positioning of the plate in the non-articular portion of the radial head (the so-called ‘‘safe-zone”) is mandatory to avoid hardware impingement during forearm rotation. When radial neck bone deficiency is present, bone may be augmented by using autologous chips taken from the lateral column of the distal humerus or the iliac crest.
Radial head excision is seldom indicated in CEI because it aggravates elbow instability. The radial head is known to provide roughly 30% of the resistance to valgus stress when the MCL is intact, though this percentage grows markedly if the ligament is injured [10,36]. The radial head also acts as an anterior buttress to posterior elbow dislocation [10,30] when the elbow is flexed and is a primary stabilizer in forearm longitudinal stability [2]. Previous studies have highlighted the association between radial head excision and a number of complications, such as chronic valgus or longitudinal instability, ulno-humeral osteoarthritis, increased carrying angle and ulnar neuropathy [26,37-40].
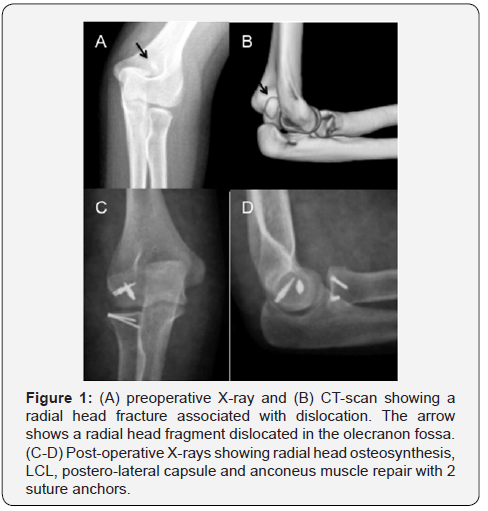
Soft tissue constraint lesions of the lateral compartment must be repaired in all patients after radial head osteosynthesis or replacement (Figure 1), whereas the LCM should be repaired in selected cases. Following surgery, elbow stability should be tested under fluoroscopy. Scanty information is available on the clinical outcome of treatment of acute postero-lateral instability of the elbow associated with radial head fractures alone; indeed, most of the existing reports retrospectively analysed heterogeneous case-series of CEI that contained few patients with this pattern [41,42]. The results of studies that focused on radial head fractures alone were instead unclear because Mason type IV fractures were not distinguished from other types of fractures. In addition, this CEI pattern is frequently underdiagnosed and confused with simple radial head fractures. In one recent study, Giannicola et al. observed this CEI pattern in 5 out of 78 patients with CEI, and reported satisfactory functional results in all cases following surgical treatment [41].
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
The coronoid process is one of the main elbow constraints that provide ulno-humeral joint stability. Coronoid fractures are rare, being reported to occur in 2-15% of patients with elbow dislocations. They are rarely found in isolation, most often being associated with other bony and soft tissue injuries surrounding the elbow [43-46]. Some authors have suggested that certain types of coronoid fractures are closely associated with specific CEI patterns [47,48]. These observations are in keeping with a recent computed tomography study [49] that lent further support to the strong association of small anterior transverse fractures with postero-lateral rotatory instability, as occurs in terrible triad injuries, whereas large basilar coronoid fractures are associated with anterior/posterior transolecranon fracturedislocations; finally, antero-medial facet (AMF) fractures are correlated with varus postero-medial rotational instability injuries.
Two main mechanisms of injury thus underlie isolated coronoid fractures associated with elbow instability: 1) posterolateral rotatory instability and 2) varus postero-medial rotatory instability. The first mechanism results in small anterior coronoid fractures and is the same as that involved in TT injuries; the second, which was defined more recently, is caused by a combination of varus and axial load on an elbow joint in the pronated position [50]. The coronoid AMF protrudes medially from the ulna metaphysis and is susceptible to varus stress trauma because approximately 60% of the facet lacks support by the ulnar metaphysis [51]. If the varus injury force continues and the lateral collateral ligament fails, an elbow subluxation or dislocation may ensue [52,53].
Since posterolateral instability alone was believed to occur and was thus described in earlier studies on the elbow, the classification proposed by Morrey focused on fractures affecting the anterior section of the process; indeed, Morrey’s classification [2] is based on the radiographic examination of such fractures on the sagittal plane. In 2003, O’Driscoll et al. [12] introduced a new classification system that is based on the anatomical location and size of the fractured fragment assessed by CT, and highlights the important contribution made by AMF fractures in reducing elbow stability. Briefly, the coronoid fracture may involve the tip (type I), the anteromedial facet (type II) or the base (type III). These three main types are further divided into subtypes depending on the severity of coronoid involvement [48].
The Type II fracture subtype needs to be identified in cases of postero-medial instability: subtype 1 fractures involve the anteromedial rim, while subtype 2 fractures extend as far as the tip; subtype 3 fractures involve the anteromedial rim and the entire sublime tubercle, either with or without the involvement of the coronoid tip. As regards type II fractures, it is worth bearing in mind that an untreated AMF fracture, however small, may lead to varus postero-medial instability on account of a concomitant LCL injury. The disrupted AMF allows the lateral ulno-humeral joint gap to open; this in turn causes increased loading on the incongruent medial ulno-humeral joint under gravitational varus stress, which may ultimately result in earlyonset medial ulno-humeral arthritis [43,44,48].
A number of techniques for coronoid fixation have been described, including transosseous sutures, K-wires, finethreaded K-wires, screws and mini-plates. However, the optimal treatment protocol and technique have yet to be established. The technique preferred by the authors of this chapter consists in using fine-threaded K-wires (FFS-Orthofix) [54]. They are inserted through the posterior aspect of the ulna, which is directed toward the coronoid using a one-step fixation technique. A varying number of fine-threaded K-wires of different diameters (1.2, 1.6, or 2.2 mm) can be positioned to increase primary and rotational stability depending on the num¬ber and size of the fragments. We have found that this technique provides easy, stable, mini¬mally-invasive and successful osteosyn¬thesis (Figure 2). When wide medial exposure is required or in comminuted fractures, osteosynthesis with precontoured miniplates is a valid alternative that increases the stability of the reconstruction and neutralizes biomechanical stress during early joint mobilization.

In their biomechanical study on postero-medial instability, Pollock et al. [55] recommended that small fragments (type IIsubtype 1) be treated by means of LCL repair alone, whereas larger fragments (type II-subtype 2 and type II-subtype 3) require fixation of the fracture fragment besides LCL repair. Park et al. [56] came to the same conclusion in their clinical study, adding that if the elbow remains unstable following coronoid fixation and LCL repair, the surgeon should investigate a hidden MCL injury, especially in subtype 2 fractures.
Hence, restoration of the LCL is of greater importance than bone fixation in type II-subtype 1 fractures because this injury may be associated with posterior dislocation. In type II-subtypes 2-3, anatomical reduction and fixation of the AMF and LCL repair are warranted because they act as a bone buttress that not only resists the varus force but also provides joint congruency [55,56]. When significant instability and/or unstable ORIF of the coronoid process persist, a HEF should be considered [23].
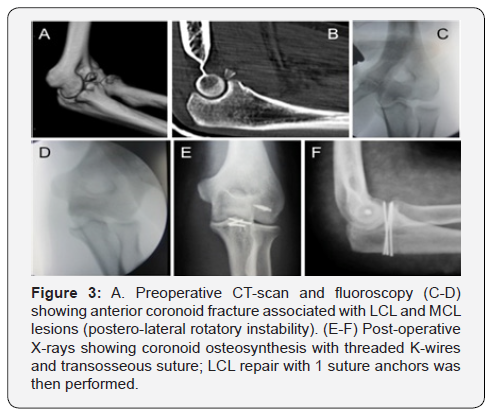
Following surgery, the elbow should be protected from varus and gravitational stresses, and shoulder elevation in internal rotation should be avoided by applying a hinged brace for 6-8 weeks if necessary. Moreover, limited extension (30°- 40°) is advisable in the first 4 weeks to avoid placing mechanical loads on the anterior part of the coronoid. The diagnostic and therapeutic principles regarding anterior coronoid fractures associated with posterolateral rotational instability (Figure 3) are similar to those of the TT, and are thus included in the following paragraph.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Terrible Triad
In 1996, Hotchkiss first described in detail a complex pattern of elbow fracture-dislocation characterized by a posterior dislocation associated with radial head and coronoid fractures, which he named the “terrible triad of the elbow” (TT) [57]. The mechanism underlying this injury is a valgus posterolateral rotatory load, caused by an axial load combined with both valgus and supinating forces on the elbow. The compression and valgus forces fracture the anterior coronoid and radial head, while the pathological supination avulses the LCL; an MCL tear is associated with other lesions in approximately 60% of cases [58,59]. The TT is a serious injury that poses a challenge to even an expert elbow surgeon and that may result in chronic instability, elbow stiffness, post-traumatic arthritis along with loss of function and chronic pain [60-76]. An increased knowledge of primary and secondary elbow stabilizers and the adoption of more standardized treatments have yielded more favorable and reproducible clinical outcomes in recent studies [64,66,69,72,74-81], though a high rate of complications and reinterventions persists [8].
The aim of TT treatment, which is the same as that of all CEI patterns, is to restore the primary and secondary stabilizers of the elbow to achieve a stable joint and allow early rehabilitation. A posterior skin incision is usually made to provide good exposure of the medial and lateral compartments, especially in cases with MCL disruption. The RHF is exposed through the Kocher interval, which widens the LCL lesion. Before radial head reconstruction or arthroplasty, coronoid osteosynthesis can be performed through a lateral approach after any radial fragments have been removed. The coronoid fracture is often a small type I Regan-Morrey fracture that can be treated by means of a simple transosseous suture also allowing the tensioning of the anterior capsule. If there is an isolated fragment that is large enough to be fixed, threaded K wires or screws may prove useful. Otherwise, a coronoid ORIF may be performed by using the medial approaches in cases of small radial head fractures in which the coronoid fragments cannot easily be visualized.
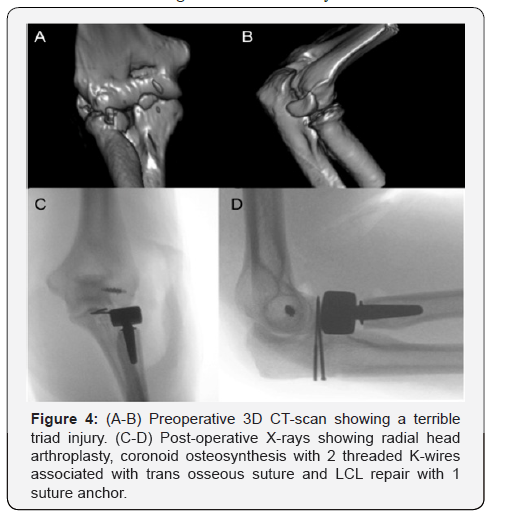
Although it has been suggested that small coronoid fractures do not require osteosynthesis [80,82,83], the need to synthesize such fragments is likely to depend on the humeral coverage angle of the greater sigmoid notch (GSN-ca). Indeed, the considerable variability of the GSN-ca on the sagittal plane that emerged from a recent MRI-anatomical study suggests that coronoid treatment should ideally be personalized. In this regard, the ORIF of small coronoid fractures may be more suited to GSNs with a low GSN-ca than to those with a higher GSN-ca [84,85]. The authors believe that a coronoid ORIF should be adopted whenever osteosynthesis is possible. After the coronoid ORIF has been performed, the radial head and ligaments should be treated (Figure 4).
In their meta-analysis of 312 cases, Chen et al. [8] reported that functional outcomes after surgery for the TT are generally satisfactory, though complications are common. The mean Mayo elbow performance scores ranged from 78 to 95, the mean Broberg-Morrey scores ranged from 76 to 90 and the mean DASH scores ranged from 9 to 31. The proportion of patients who underwent a reoperation following complications, most of which were related to hardware fixation problems, joint stiffness, joint instability and ulnar neuropathy, ranged from 0 to 54.5% (mean 22.4%). The complications least likely to require a reoperation were heterotopic ossification (12.5%) and arthrosis (11.2%). These results confirm that the TT remains a challenging lesion to treat and the complication rate is significant. Furthermore, unavoidable factors, such as obesity, low compliance, delayed treatment and extensive soft elbow tissue damage, are additional negative prognostic factors that may affect the surgical outcomes [76].
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
Fracture-dislocations of the proximal ulna and radius (FDUR) account for between 2% and 5% of all elbow injuries [86,87]. The term “fracture-dislocations of the proximal ulna and radius” includes any ulnar fracture associated with an isolated elbow joint dislocation or multiple elbow joint dislocations (radiohumeral, ulno-humeral and proximal radio-ulnar joints); the whole ulna has to be damaged to be included in this definition so as to distinguish this from other CEI patterns, such as TT injuries or postero-medial instability, in which only an apophysis of the proximal ulna (i.e. the coronoid process or supinator crest) has been fractured [88].
In 1814, Monteggia described, for the first time, the fracture of the proximal ulna associated with an anterior dislocation of the radial head [89]. However, until a few decades ago, the eponym ‘Monteggia fracture’ was also used to refer to other complex FDURs that were not originally included by Monteggia himself. These types of lesions usually comprised various coronoid, olecranon, ulnar shaft and radial head injuries, i.e. the majority of the bone structures involved in elbow stability. Several FDUR classifications have been proposed over the years, though none has proved to be exhaustive and few are of any therapeutic or prognostic value [90-93]. Moreover, as most of these classifications were designed a number of years ago, they do not take into consideration more recently acquired knowledge on the functional anatomy of the elbow, which includes the complex interaction between bone and soft-tissue constraints of the joint [1,10,94-96].
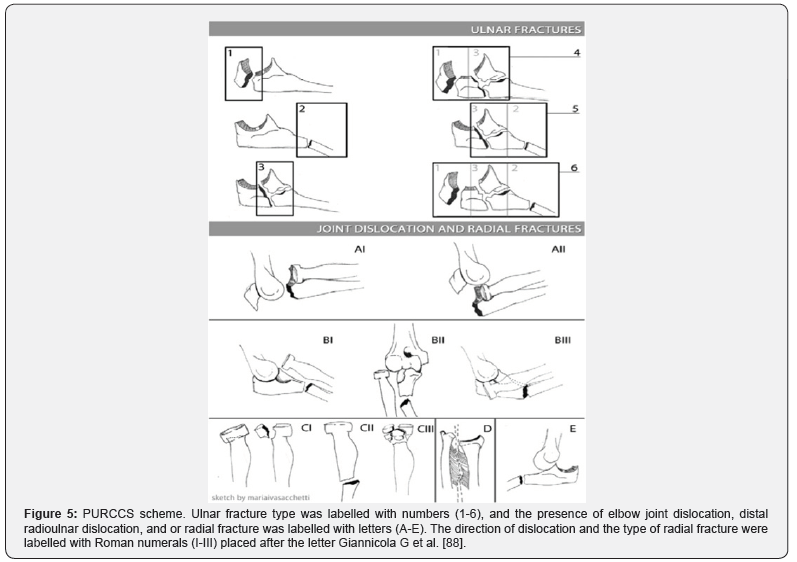
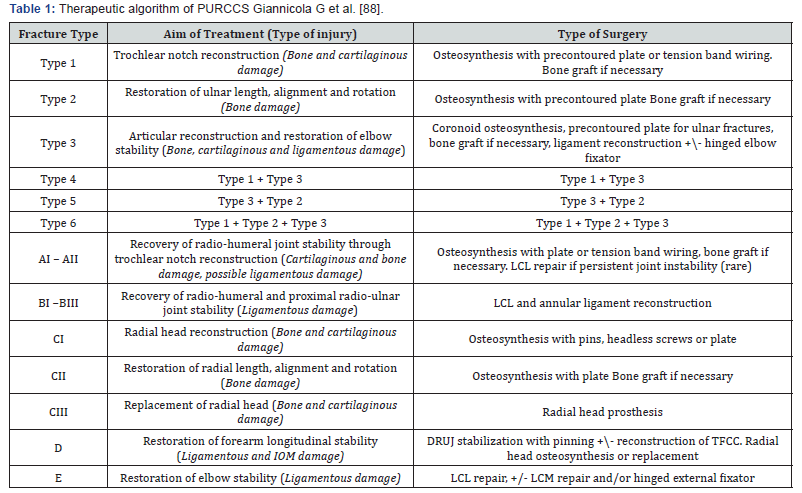
A new comprehensive classification of fracture-dislocations of the proximal ulna and radius (PURCCS) has recently been proposed by the authors [88]. The aim of this new classification is to identify definite anatomical lesions, referred to as ‘‘main lesions,’’ whose presence may affect the prognosis and that require a specific type of treatment. The main lesions that make up the FDUR patterns and are labelled using an alphanumeric system include: 1) the type of ulnar fracture, including its location in relation to the insertion of the collateral ligaments and coronoid process (type 1-6); 2) the presence of an isolated radio-humeral dislocation (A lesion); 3) the presence of a radiohumeral dislocation with a proximal radio-ulnar dislocation (B lesion); 4) the presence of radial fractures (C lesion); 5) the presence of the distal radio-ulnar joint and interosseous membrane lesions (D lesion); finally, 6) the presence of an ulnohumeral dislocation (E lesion). According to this classification, any given FDUR pattern arises from the association of at least two main lesions, which must include an ulnar fracture combined with an isolated dislocation or multiple dislocations of the elbow joints, radial fractures and forearm lesions (Figure 5).
As a missed diagnosis of soft-tissue constraint injuries associated with elbow and wrist joint dislocations was one of the most frequent causes of a poor outcome in FDUR [93,97- 100], the PURCSS classification was designed in such a way as to take into account any damage to the collateral ligaments in patients with these injuries; all the FDURs were therefore classified in A and B lesions. The A lesion indicates the presence of a radio-humeral dislocation with no injury to the proximal radio-ulnar joint; it is usually associated with a type 1 ulnar fracture (olecranon fracture) and both bones in the forearm dislocated as a single unit. We make a distinction between 2 possible directions of a radio-humeral joint dislocation: anterior (AI) and posterior (AII). The AI lesion corresponds to the anterior transolecranon fracture-dislocation described by Biga and Thomine [101], and the AII lesion corresponds to the rarely seen posterior transolecranon fracture-dislocation described by Marotte et al. [102]. While the LCL and MCL may on occasion be injured, the annular and quadrate ligaments tend to remain intact; the A lesion is largely a bone injury.
The B lesion is a radio-humeral dislocation associated with a proximal radio-ulnar joint dislocation. The radio-humeral dislocation may be anterior (BI), lateral (BII) or posterior (BIII). A lesion of the LCL complex always occurs and the quadrate ligament is often injured as well. MCL lesions are present in about one third of cases [58]. The B lesions include the typical joint damage that is observed in the Monteggia fracture-dislocation described by Monteggia & Bado [89,103]. The dislocations in such cases are often combined with a type 2 and type 3 ulnar fracture, and may even be associated with a proximal radial fracture.
Therefore, according to the PURCCS, isolated dislocations of the radio-humeral joint (A lesion) are thus distinguished from those associated with a proximal radio-ulnar joint dislocation (B lesion) in that the former do not require any soft-tissue reconstruction, whereas the latter are often associated with persistent instability, even following ulnar osteosynthesis, because of damage to the LCL complex. We believe that greater accuracy when diagnosing a transolecranon fracture-dislocation (A lesion) or a Monteggia-like lesion (B lesion) is more likely to result in the most appropriate treatment for these injuries.
Injuries to the interosseous membrane and distal radioulnar joint (DRUJ) (D lesion) are included among the main lesions because they may be associated with FDUR and require additional treatment [87,104]. Ulno-humeral joint dislocation (E lesion), which is typically associated with complex shaft ulnar fractures, was included as another main lesion. This infrequent injury is caused by high-energy trauma and is characterized by the combination of complex soft-tissue constraint damage and an ulnar fracture, which is often comminuted; the prognosis in such injuries tends to be poor [105-107]. The presence of a radial fracture (C lesion) plays an important additional role in the prognosis of elbow fracture-dislocations [1,86,93,108,109]. We described 3 types of radial fractures that require specific treatment, according to the Hotchkiss classification and by taking into account the possible association with proximal radial shaft fractures [29].

The PURCCS classification helps to identify the main lesions within each injury FDUR pattern that require a specific type of treatment (Figure 6). In fact, the accompanying, highly detailed, therapeutic algorithm (Table 1) helps to select the most suitable surgical strategies. In particular, the following questions should be addressed before surgery is planned: (1) To what extent has the ulna been injured (from type 1 to type 6)? (2) Is the radiohumeral joint alone involved (A lesion), or is it associated with a proximal radio-ulnar joint dislocation (B lesion)? (3) Is the radius fractured (C lesion) and, if so, what type of fracture is it? (4) Are the elbow joints alone involved, or are the interosseous membrane and the DRUJ (D lesion) also involved? (5) Lastly, is an ulno-humeral dislocation (E lesion) present? When answering these questions, the surgeon should consider all the main lesions that may require treatment to achieve good results. In a case series of 39 FDUR cases that were classified and treated according to the PURCCS, we achieved satisfactory clinical results in the majority of patients, reporting few major complications or re-interventions. The MEPS, Dash score and m-ASES score in our series were respectively 91.2, 14.9 and 83.9 [110].
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
Humeral shear fractures are rare injuries that involve the capitellum and trochlea and account for 1 % of all elbow fractures and 6 % of distal humeral fractures; the incidence of such fractures is higher in women than in men because the former suffer from osteoporosis to a greater extent than the latter [111]. The mechanism of injury usually consists of a fall on an outstretched arm, which results in direct axial and valgus compression transmitted to the capitellum by the radial head [112]. Several classifications have been proposed for this kind of fracture, the most widely used being that by Bryan- Morrey. In 2006, Dubberley et al. [113] classified humeral shear fractures according to 3 different types: type 1, which involves the capitellum with or without the lateral trochlear ridge; type 2, a fracture of the capitellum and trochlea as one piece; type 3, fractures of both the capitellum and the trochlea as separate pieces. These fractures are further divided depending on the absence (A) or presence (B) of posterior condylar comminution given that osteosynthesis may be more challenging in the latter case.
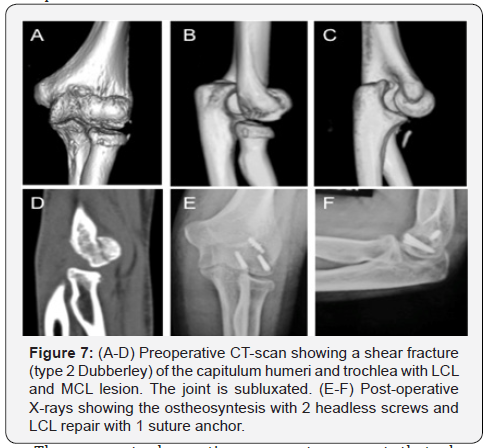
Coronal shear fractures usually occur in isolation with a stable elbow, but may be involved in a more complex elbow injury with other osseous and soft-tissue constraint lesions. Indeed, an associated radial head fracture has been observed in as many as 30% of cases [111,113-116] while an association with an olecranon or coronoid fracture is rarer [117-119]. Ruchelsmann reported that 4 out of 5 associated radial head fractures in his series occurred in type IV fractures, according to the Bryan-Morrey classification [119]. Some studies have observed LCL lesions in up to 40% of cases [113-116]. In their series of 18 patients, Mighel et al. [116] found that a LCL injury was more often associated with injuries involving the capitellum and trochlea as one piece than with isolated fractures of the capitellum. In another series of 15 patients who sustained humeral shear fractures and were treated with ORIF and hinged external fixation, Giannicola et al. [120] reported 4 cases who had an elbow dislocation associated with both collateral ligament disruption, while another 4 cases had a MCL tear.
These recent observations seem to suggest that shear fractures associated with elbow dislocation or lateral and medial collateral ligament tears may represent a pattern of CEI according to which bone failure occurs on the humeral rather than on the ulnar or radial side. This is the reason why we decided to include this type of lesion in CEI even though no consensus has yet been reached on this issue. A distinction should be made between this type of injury and monocondylar fractures of the distal humerus, which are unstable owing to the fragment displacement which includes the collateral ligament that remains intact. In the latter case, condylar ORIF directly restores the stability of the elbow, whereas ligament reconstruction is required after ORIF when shear fractures are associated with ligament lesions; in such cases, the pathoanatomical finding of a soft tissue constraint lesion is, in our experience, comparable to that observed in other CEI patterns [120].
In view of these considerations, the same therapeutic algorithm of CEI should be applied to this type of injury. In brief, correct surgical treatment consists in performing ORIF with headless screws and ligament repair (Figure 7), as has also been advocated by other authors [121]. There is as yet no consensus on the optimal method of fixation for these challenging fractures, though headless compression screws are widely adopted. Indeed, one biomechanical study has shown that the placement of headless compression screws in an anterior-posterior fashion is superior to placing cancellous screws in a posterior-to-anterior fashion [122]. Furthermore, placing screws in an anterior-toposterior fashion does not entail disrupting the posterior soft tissues, and thus helps to preserve the distal humeral blood supply.
When posterior comminution is present, supplemental fixation with a plate and bone graft may be required. Capitellar excision is another option, which may however lead to complications, such as elbow instability. ORIF is thus recommended whenever possible, with capitellar excision being reserved for small, unfixable fractures. Indeed, a recent biomechanical study showed that even small impaction fractures of the posterior part of the capitellum reduce radiocapitellar stability, particularly in elbow fracture dislocations [20]. A capitellar prosthesis, humeral hemiarthroplasty or total elbow arthroplasty should therefore be considered in patients with fractures that cannot be repaired, especially in Dubberley type 3 fractures. Following fracture treatment, the LCL always needs to be repaired and the stability checked. The remaining steps in the surgical procedure are the same as those described above for the other CEI patterns.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Soft Tissue Constraint Injuries in Complex Elbow Instability: Prevalence, Pathoanatomy
Classification and Treatment
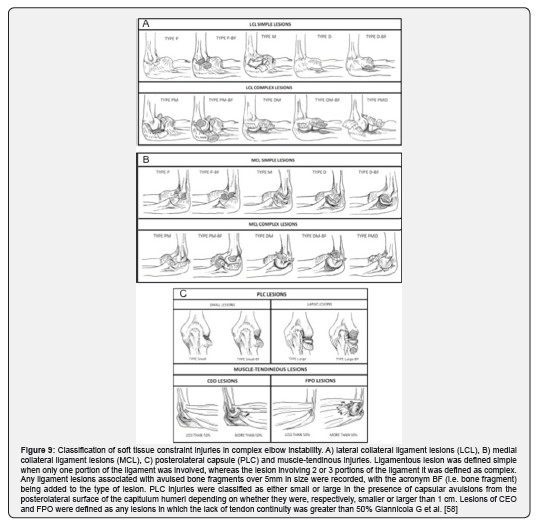
Soft tissue constraint injuries are consistently found in all CEI patterns [2,5,7,58,59]; unless these lesions are recognized and treated adequately, postoperative elbow instability is likely to occur and disappointing long-term clinical results are to be expected [2,5,22,23]. To date, few studies have analyzed the prevalence and pathoanatomy of soft tissue constraint lesions [58,59]. In a study by Giannicola et al. the LCL was found to be the most frequently injured soft tissue constraint (96%); MCL and posterolateral capsule (PLC) tears were observed, respectively, in about 45% and 66% of cases. PLC lesions were always associated with proximal LCL avulsion, which was combined with anconeus humeral detachment in large tears in all cases. Common extensor tendon origin (CEO) and flexor-pronator tendon origin (FPO) injuries were detected in approximately one third of the cases [59].
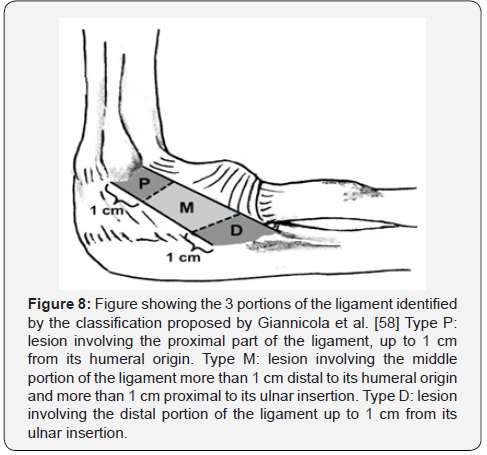
On the basis of pathoanatomical findings, the authors proposed a comprehensive classification of soft tissue constraint injuries; in particular, ligament injuries were distinguished as simple or complex lesions, depending on whether the liga¬ment was damaged in only 1 portion or in 2-3 portions (Figure 8, Figure 9A-B). PLC, CEO and FPO injuries were classified as well (Figure 9C) [59].
The identification of the type and severity of soft tissue constraint lesions involved in complex elbow instability might help to select the most ap¬propriate treatment, thereby restoring the original function of the primary and second¬ary soft tissue stabilizers of the elbow joint. This surgical strategy may reduce the rate of postoperative instabilities and improve the surgical out¬comes in this patient population. Giannicola et al. described a detailed surgical technique to repair each type of lesion pattern (Figure 10) and reported the clinical outcomes in 45 patients [123]. The MEPS, DASH and m-ASES scores after a mean follow-up of 25 months were 94, 5.6, and 89, respectively; 93% of the patients recovered elbow stability. To our knowledge, no other studies have yet focused on this topic in the literature; indeed, most of the papers that have been published only mention the use of suture anchors or transosseous sutures, but do not describe the technique used for each pattern of soft tissue constraint lesion. A comprehensive and reproducible classification of these injuries may be useful to guide surgeons in the re¬constitution of soft tissue constraints of the elbow joint and to compare the results of different surgical techniques.
- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
Postoperative Treatment
Two drainages (one endoarticular, the other subcutaneous) are applied at the end of the operation and the elbow is immobilized in a plaster splint for the first 48 hours. The elbow position is normally chosen upon completion of the surgical procedure and after joint stability has been assessed by means of fluoroscopy; the elbow should be positioned in maximum extension to avoid anterior bleeding as well as flexion contracture. The upper limb needs to be placed in the elevated position and cryotherapy and analgesic therapy are administered. To prevent heterotopic ossifications, pharmacological prophylaxis with indomethacin (100 mg daily) is usually administered to all patients day for 5 weeks starting from the second postoperative. Once the drainages are removed (after 48 hours), a hinged elbow brace is applied for between 45 and 60 days to protect the joint reconstruction in the early rehabilitation phases. The use of a compression arm sleeve for 3-4 weeks after surgery is likely to help minimize swelling and improve blood circulation. If a HEF needs to be implanted during surgery, it is kept locked in extension for 48 hours and then unlocked. The device is usually removed between 6 and 8 weeks following surgery to allow soft tissue and bone tissue lesion/reconstruction to heal fully.
The elbow rehabilitation programme should be started immediately and continued for at least 6 months because the most significant improvement in elbow range of motion (ROM) occurs in this period, which should thus be considered the critical time period to achieve a good functional outcome [42]. In the early phases, rehabilitation should be performed in the so-called “over the head” position, in which gravity helps to keep congruent the ulno-humeral and radiocapitellar joints throughout the arc of movement. In a recently published study, a case series of 76 cases affected by CEI was analyzed in the postoperative period; 70% of the patients recovered functional ROM between the third and sixth month, though the recovery of flexion proved to be slower than that of the other elbow movements. Thereafter, improvement continued, though at a lower rate, until the end of the first year, when approximately 80% of the patients had recovered the functional ROM [42].

- Review Article
- Abstract
- Introduction
- Diagnosis
- General Principles of Treatment
- Complex elbow Instability Patterns
- Coronoid Fractures with Associated Lateral Collateral Ligament Lesions
- Terrible Triad
- Fracture-Dislocations of the Proximal Ulna and Radius: Monteggia-Like Lesions and Transolecranon Fracture-Dislocation
- Humeral Shear Fractures with Associated Lateral and Medial Collateral Ligament Lesions
- Instability: Prevalence, Pathoanatomy
- Postoperative Treatment
- References
References
- Jupiter JB, Leibovic SJ, Ribbans W, Wilk RM (1991) The posterior Monteggia lesion. J Orthop Trauma 5(4): 395-402.
- Morrey BF (1998) Complex instability of the elbow. Instr Course Lect 47: 157-164.
- Ring D, Jupiter JB, Simpson NS (1998) Monteggia fractures in adults. J Bone Joint Surg Am 80(12): 1733-1744.
- Biyani A, Olscamp AJ, Ebraheim NA (2000) Complications in the management of complex monteggia-equivalent fractures in adults. Am J Orthop 29(2):115–118.
- Ring D, Jupiter JB (2002) Fracture–dislocation of the elbow. Hand Clin 18(1): 55-63.
- Konrad GG, Kundel K, Kreuz PC, Oberst M, Sudkamp NP (2007) Monteggia fractures in adults. Long term results and prognostic factors. J Bone Joint Surg Br 89(3): 354-360.
- Morrey BF (2009) Current concepts in the manage¬ment of complex elbow trauma. Surgeon 7(3): 151-61.
- Chen HW, Liu GD, Wu LJ (2014) Complications of treating terrible triad injury of the elbow: a systematic review. PLoS One 9: e974-76.
- Morrey BF, An KN (1983) Articular and ligamen¬tous contributions to the stability of the elbow joint. Am J Sports Med 11: 315-319.
- Morrey BF, Tanaka S, An KN (1991) Valgus stabil¬ity of the elbow. A definition of the primary and secondary constraints. Clin Orthop Relat Res 265: 187-195.
- Closkey RF, Goode JR, Kirschenbaum D, Cody RP (2000) The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. Bone Joint Surg Am 82-A: 1749-1753.
- O’Driscoll SW, Jupiter JB, King GJ (2001) The unstable el¬bow. Instr Course Lect 50: 89-102.
- Deutch SR, Jensen SL, Tyrdal S, Olsen BS, Sneppen O (2003) Elbow joint stability following experimental osteoligamentous injury and re¬construction. J Shoulder Elbow Surg 12(5): 466-471.
- Hull JR, Owen JR, Fern SE, Wayne JS, Boardman ND 3rd (2005) Role of the coronoid process in varus osteoarticular stability of the elbow. J Shoulder Elbow Surg 14(4): 441-446.
- Morrey BF, An KN (2005) Stability of the elbow: osseous constraints. J Shoulder Elbow Surg 14: S174-178S.
- Beingessner DM, Dunning CE, Stacpoole RA, Johnson JA, King GJ (2007) The effect of coronoid fractures on elbow kinematics and stability. Clin Biomech (Bristol, Avon) 22(2): 183-190.
- Park MC, Ahmad CS (2004) Dynamic contribu¬tions of the flexor–pronator mass to elbow valgus stability. J Bone Joint Surg Am 86: 2268-2274.
- Seiber K, Gupta R, McGarry MH, Safran MR, Lee TQ (2009) The role of the elbow mus¬culature, forearm rotation, and elbow flex¬ion in elbow stability: an in vitro study. J Shoulder Elbow Surg 18(2): 260- 268.
- Sabo MT, Fay K, McDonald CP, Ferreira LM, Johnson JA, et al. (2010) Effect of coronal shear fractures of the distal humerus on elbow kinematics and stability. J Shoulder Elbow Surg 19(5): 670-680.
- Shukla DR, Thoreson AR, Fitzsimmons JS, An KN, O'Driscoll SW (2015) The effect of capitellar impaction fractures on radiocapitellar stability. J Hand Surg Am 40(3): 520-525.
- Sotereanos DG, Darlis NA, Wright TW, Goitz RJ, King GJ (2007) Unstable fracture-dislocations of the elbow. Instr Course Lect 56: 369–376.
- Giannicola G, Sacchetti FM, Greco A, Cinotti G, Postacchini F (2010) Management of complex elbow instability. Musculoskelet Surg 94: S25-S36.
- Wyrick JD, Dailey SK, Gunzenhaeuser JM, Casstevens EC (2015) Management of Complex Elbow Dislocations: A Mechanistic Approach. J Am Acad Orthop Surg 23(5): 297-306.
- Nielsen D, Nowinski RJ, Bamberger HB (2002) Indications, alternatives, and complications of external fixation about the elbow. Hand Clin 18(1): 87-97.
- Tan V, Daluiski A, Capo J (2005) Hinged elbow external fixators: indications and uses. J Am Acad Orthop Surg 13(8): 503–514.
- Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Nyqvist F, et al. (2004) Fractures of the radial head and neck treated with radial head excision. J Bone Joint Surg Am 86-A(9): 1925–1930.
- Morrey BF (1993) Radial head fracture. In: Morrey BF (ed) The elbow and its disorders. (2nd edn), WB Saunders, Philadelphia, USA, pp. 383-404.
- van Riet RP, Morrey BF, O'Driscoll SW, Van Glabbeek F (2005) Associated injuries complicating radial head fractures: a demographic study. Clin Orthop Relat Res 441: 351–355.
- Hotchkiss RN (1997) Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg 5(1): 1–10.
- Shukla DR, Fitzsimmons JS, An KN (2012) Effect of radial head malunion on radiocapitellar stability. J Shoulder Elbow Surg 21(6): 789-794.
- Fowler JR, Goitz RJ (2013) Radial head fractures: indications and outcomes for radial head arthroplasty. Orthop Clin North Am 44(3): 425-431.
- Al-Burdeni S, Abuodeh Y, Ibrahim T, Ahmed G (2015) Open reduction and internal fixation versus radial head arthroplasty in the treatment of adult closed comminuted radial head fractures (modified Mason type III and IV). Int Orthop 39(8): 1659-1664.
- Ruan HJ, Fan CY, Liu JJ, Zeng BF (2009) A comparative study of internal fixation and prosthesis replacement for radial head fractures of Mason type III. Int Orthop 33(1): 249-253.
- Li N, Chen S (2014) Open reduction and internal-fixation versus radial head replacement in treatment of Mason type IIIradial head fractures. Eur J Orthop Surg Traumatol 24(6): 851-855.
- Liu R, Liu P, Shu H, Gong J, Sun Q, et al. (2015) Comparison of primary radial head replacement and ORIF (open reduction and internal fixation) in Mason type III fractures: a retrospective evaluation in 72 elderly patients. Med Sci Monit 21: 90-93.
- Søjbjerg JO, Ovesen J, Nielsen S (1987) Experimental elbow instability after transection of the medial collateral ligament. Clin Orthop Relat Res 218: 186-190.
- Morrey BF, Chao EY, Hui FC (1979) Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am 61(1): 63-68.
- Ikeda M, Sugiyama K, Kang C (2005) Comminuted fractures of the radial head. Comparison of resection and internal fixation. J Bone Joint Surg Am 87(1): 76-84.
- Pilato G, De Pietri M, Vernieri W, Bini A (2004) The surgical treatment of fractures of the radial head: a comparison between osteosynthesis and capitellectomy. Chir Organi Mov 89(3): 213–222.
- Lindenhovius AL, Felsch Q, Doornberg JN, Ring D, Kloen P (2007) Open reduction and internal fixation compared with excision for unstable displaced fractures of the radial head. J Hand Surg Am 32(5): 630-636.
- Giannicola G, Polimanti D, Bullitta G, Sacchetti FM, Cinotti G (2014) Critical time period for recovery of functional range of motion after surgical treatment of complex elbow instability: prospective study on 76 patients. Injury 45: 540-545.
- Wang ML, Beredjiklian PK (2015) Management of radial head fracture with elbow dislocation. J Hand Surg Am 40: 813-816.
- Budoff JE (2012) Coronoid fractures. J Hand Surg Am 37: 2418-2423.
- Manidakis N, Sperelakis I, Hackney R, Kontakis G (2012) Fractures of the ulnar coronoid process. Injury 43(7): 989-998.
- Steinmann SP (2008) Coronoid process fracture. J Am Acad Orthop Surg 16(9): 519-529.
- Wells J, Ablove RH (2008) Coronoid fractures of the elbow. Clin Med Res 6: 40-44.
- Doornberg J, Ring D, Jupiter JB (2004) Effective treatment of fracture dislocation of the olecranon requires a stable trochlear notch. Clin Orthop Relat Res 429: 292-300.
- O'Driscoll SW, Jupiter JB, Cohen MS, Ring D, Mckee MD (2003) Difficult elbow fractures: pearls and pitfalls. Instr Course Lect 52: 113-134.
- Mellema JJ, Janssen SJ, Guitton TG (2015) Quantitative 3-dimensional computed tomography measurements of coronoid fractures. J Hand Surg Am 40(3): 526-533.
- Sanchez-Sotelo J, O’Driscoll SW, Morrey BF (2005) Anteromedial fracture of the coronoid process of the ulna. J Shoulder Elbow Surg 15: e5–e8.
- Doornberg JN, Ring D (2006) Coronoid fracture patterns. J Hand Surg Am 31(1): 45-52.
- Regan W, Morrey B (1989) Fractures of the coronoid process of the ulna. J Bone Joint Surg Am 71: 1348–1354.
- Ring D (2006) Fractures of the coronoid process of the ulna. J Hand Surg Am 31(10): 1679-1689.
- Giannicola G, Polimanti D, Gumina S, Cinotti G (2013) Use of fine-threaded K-wires in the treatment of coronoid fractures in complex elbow instability. Orthopedics 36(10): e1233-1238.
- Pollock JW, Brownhill J, Ferreira L, McDonald CP, Johnson J, et al. (2009) The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am 91(6):1448-1458.
- Park SM, Lee JS, Jung JY, Kim, JY, Song KS (2015) How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J Shoulder Elbow Surg 24(1): 74-82.
- Hotchkiss RN (1996) Fractures and dislocations of the elbow. In: Rockwood CA, Green DP, Bucholz RW, Heckman JD (ed), Rockwood and Green’s fractures in adults, vol. 1, (4th edn), Lippincott-Raven, Philadelphia, USA, pp. 929–1024.
- Giannicola G, Polimanti D, Sacchetti FM, Scacchi M, Gumina S, et al. (2012) Soft tissue constraint injuries in complex elbow instability: prevalence, pathoanatomy, and classification. Orthopedics 35: e1738-1745.
- McKee MD, Schemitsch EH, Sala MJ, O'driscoll SW (2003) The pathoanatomy of later¬al ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg 12(4): 391-396.
- Josefsson PO, Gentz CF, Johnell O, Wendeberg B (1989) Dislocations of the elbow and intraarticular fractures. Clin Orthop Relat Res 246: 126-130.
- Ring D, Jupiter JB, Zilberfarb J (2002) Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am 84: 547-551.
- Van Riet RP, Morrey BF, O'Driscoll SW (2005) Use of osteochondral bone graft in coronoid fractures. J Shoulder Elbow Surg 14(5): 519-523.
- Egol KA, Immerman I, Paksima N, Tejwani N, Koval KJ (2007) Fracture-dislocation of the elbow functional outcome following treatment with a standardized protocol. Bull NYU Hosp Jt Dis 65(4): 263-270.
- Forthman C, Henket M, Ring DC (2007) Elbow dislocation with intra-articular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am 32(8): 1200-1209.
- Kälicke T, Muhr G, Frangen TM (2007) Dislocation of the elbow with fractures of the coronoid process and radial head. Arch Orthop Trauma Surg 127(10): 925-931.
- Lindenhovius AL, Jupiter JB, Ring D (2008) Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am 33(6): 920-926.
- Seijas R, Ares-Rodriguez O, Orellana A, Albareda D, Collado D, et al. (2009) Terrible triad of the elbow. J Orthop Surg 17(3): 335-339.
- Winter M, Chuinard C, Cikes A, Pelegri C, Bronsard N, et al. (2009) Surgical management of elbow dislocation associated with non-reparable fractures of the radial head. Chir Main 28: 158-167.
- Chemama B, Bonnevialle N, Peter O, Mansat P, Bonnevialle P (2010) Terrible triad injury of the elbow: how to improve outcomes? Orthop Traumatol Surg Res 96(2): 147-154.
- Wang YX, Huang LX, Ma SH (2010) Surgical treatment of "terrible triad of the elbow": technique and outcome. Orthop Surg 2(2): 141-148.
- Garrigues GE, Wray WH 3rd, Lindenhovius AL, Ring DC, Ruch DS. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg Am 19: 1873-1881.
- Leigh WB, Ball CM (2012) Radial head reconstruction versus replacement in the treatment of terrible triad injuries of the elbow. J Shoulder Elbow Surg 21: 1336-1341.
- Tarassoli P, McCann P, Amirfeyz R (2017) Complex instability of the elbow. Injury 48(3): 568-577.
- Fitzgibbons PG, Louie D, Dyer GS, Blazar P, Earp B (2014) Functional outcomes after fixation of "terrible triad" elbow fracture dislocations. Orthopedics 37: e373-376.
- Watters TS, Garrigues GE, Ring D, Ruch DS (2014) Fixation versus replacement of radial head in terrible triad: is there a difference in elbow stability and prognosis? Clin Orthop Relat Res 472: 2128-2135.
- Giannicola G, Calella P, Piccioli A, Scacchi M, Gumina S (2015) Terrible triad of the elbow: is it still a troublesome injury? Injury 46: S68-S76.
- Zeiders GJ, Patel MK (2008) Management of unstable elbows following complex fracture-dislocations--the "terrible triad" injury. J Bone Joint Surg Am 90: 75-84.
- Jeong WK, Oh JK, Hwang JH, Hwang SM, Lee WS (2010) Results of terrible triads in the elbow: the advantage of primary restoration of medial structure. J Orthop Sci 15: 612-619.
- Rodriguez-Martin J, Pretell-Mazzini J, Andres-Esteban EM, Larrainzar-Garijo R (2011) Outcomes after terrible triads of the elbow treated with the current surgical protocols A review. Int Orthop 35: 851-860.
- Papatheodorou LK, Rubright JH, Heim KA, Weiser RW, Sotereanos DG (2014) Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res 472(7): 2084-2091.
- Zhang C, Zhong B, Luo CF (2014) Treatment strategy of terrible triad of the elbow: experience in Shanghai 6th People's Hospital. Injury 45(6): 942-948.
- Chan K, MacDermid JC, Faber KJ, King GJ, Athwal GS (2014) Can we treat select terrible triad injuries nonoperatively? Clin Orthop Relat Res 472(7): 2092-2099.
- Mathew PK, Athwal GS, King GJ (2009) Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg 17(3): 137-151.
- Giannicola G, Sedati P, Cinotti G, Bullitta G, Polimanti D (2015) The ulnar greater sigmoid notch "coverage angle": bone and cartilage contribution. Magnetic resonance imaging anatomic study on 78 elbows. J Shoulder Elbow Surg 24(12): 1934-1938.
- Wadström J, Kinast C, Pfeiffer K (1986) Anatomical variations of the semilunar notch in elbow dislocations. Arch Orthop Trauma Surg 105(5): 313-315.
- Eathiraju S, Mudgal C, Jupiter JB (2007) Monteggia fracture-dislocations. Hand Clin 23(2): 165-177.
- Josten C, Freitag S (2009) Monteggia and Monteggia-like-lesion: classification, indication and techniques in operative treatment. Eur J Trauma Emerg Surg 35(3): 296-304.
- Giannicola G, Greco A, Sacchetti FM, Cinotti G, Nofroni I, et al. (2011) Complex fracture-dislocations of the proximal ulna and radius in adults: a comprehensive classification. J Shoulder Elbow Surg 20: 1289-1299.
- Monteggia GB (1814) Istruzioni chirurgiche. Vol 5. Pirotta & Maspero, Milano, Italy, p. 52-138.
- Boyd HB, Boals JC (1969) The Monteggia lesion: a review of 159 cases. Clin Orthop Relat Res 66: 94-100.
- Bruce HE, Harvey JP, Wilson JC (1974) Monteggia fractures. J Bone Joint Surg Am 56: 1563-1576.
- Egol KA, Tejwani N, Bazzi J, Susarla A, Koval KJ (2005) Does a Monteggia variant lesion result in a poor functional outcome? A retrospective study. Clin Orthop Relat Res 438: 233-238.
- Givon U, Pritsch M, Levy O (1997) Monteggia and equivalent lesions: a study of 41 cases. Clin Orthop Relat Res 337: 208-215.
- Hotchkiss RN, An KN, Sowa DT, Basta S, Weiland AJ (1989) An anatomic and mechanical study of the interosseous membrane of the forearm: pathomechanics of proximal migration of the radius. J Hand Surg Am 14: 256-261.
- Pomianowski S, O’Driscoll SW, Neale PG, Park MJ, Morrey BF, et al. (2001) The effect of forearm rotation on laxity and stability of the elbow. Clin Biomech (Bristol, Avon) 16(5): 401-407.
- Wadia F, Kamineni S, Dhotare S, Amis A (2007) Radiographic measurements of normal elbows: clinical relevance to olecranon fractures. Clin Anat 20(4): 407-410.
- Reckling FW (1982) Unstable fracture-dislocations of the forearm (Monteggia and Galeazzi lesions). J Bone Joint Surg Am 64: 857-863.
- Ring D, Jupiter JB, Simpson S (1998) Monteggia fractures in adults. J Bone Joint Surg Am 80: 1733-1744.
- Ahmad MA, White A, Reza SA, Rai A, Patel AD (2005) When is a Monteggia fracture not a Monteggia fracture? Inj Extra 38: 51-53.
- Doornberg JN, de Jong IM, Lindenhovius AL, Ring D (2007) The anteromedial facet of the coronoid process of the ulna. J Shoulder Elbow Surg 16(5): 667–670.
- Biga N, Thomine JM (1974) Trans-olecranal dislocations of the elbow. Rev Chir Orthop Reparatrice Appar Mot 60(7): 557–567.
- Marotte JH, Samuel P, Lord G (1982) La fracture-luxation conjointe de l’extremite superieure des deux os de l’avant-bras. Rev Chir Orthop 68: 104-114.
- Bado JL (1967) The Monteggia lesion. Clin Orthop Relat Res 50: 71-86.
- Gul A, Sambandam S, Rangaswamy S (2007) Ipsilateral Monteggia fracture dislocation with volar lunate dislocation of wrist: a case report. Eur J Orthop Surg Traumatol 17(3): 331-333.
- Karlstad R, Morrey BF, Cooney WP (2005) Failure of fresh-frozen radial head allografts in the treatment of Essex-Lopresti injury: a report of four cases. J Bone Joint Surg Am 87(8): 1828-1833.
- Strauss EJ, Tejwani NC, Preston CF, Egol KA (2006) The posterior Monteggia lesion with associated ulnohumeral instability. J Bone Joint Surg Br 88(1): 84-89.
- Mouhsine E, Akiki A, Castagna A, Cikes A, Wettstein M, et al. (2007) Transolecranon anterior fracture dislocation. J Shoulder Elbow Surg 16(3): 352-357.
- Penrose JH (1951) The Monteggia fracture with posterior dislocation of the radial head. J Bone Joint Surg Br 33-B(1): 65-73.
- Llusa Perez M, Lamas C, Martinez I (2002) Monteggia fractures in adults: review of 54 cases. Chir Main 21(5): 293-297.
- Giannicola G, Scacchi M, Sacchetti FM, Cinotti G (2013) Clinical usefulness of proximal ulnar and radial fracture-dislocation comprehensive classification system (PURCCS): prospective study of 39 cases. J Shoulder Elbow Surg 22(12): 1729-1736.
- Yari SS, Bowers NL, Craig MA, Reichel LM (2015) Management of distal humeral coronal shear fractures. World J Clin Cases 3(5): 405-417.
- McKee MD, Jupiter JB, Bamberger HB (1996) Coronal shear fractures of the distal end of the humerus. J Bone Joint Surg Am 78(1): 49-54.
- Dubberley JH, Faber KJ, Macdermid JC, Patterson SD, King GJ (2006) Outcome after open reduction and internal fixation of capitellar and trochlear fractures. J Bone Joint Surg Am 88(1): 46-54.
- Ashwood N, Verma M, Hamlet M (2010) Transarticular shear fractures of the distal humerus. J Shoulder Elbow Surg 19(1): 46-52.
- Lee JJ, Lawton JN (2012) Coronal shear fractures of the distal humerus. J Hand Surg Am 37: 2412-2417.
- Mighell M, Virani NA, Shannon R, Echols EL Jr, Badman BL, Keating CJ. Large coronal shear fractures of the capitellum and trochlea treated with headless compression screws. J Shoulder Elbow Surg 19(1): 38-45.
- Goodman HJ, Choueka J (2005) Complex coronal shear fractures of the distal humerus. Bull Hosp Jt Dis 62(3-4): 85-89.
- Watts AC, Morris A, Robinson CM (2007) Fractures of the distal humeral articular surface. J Bone Joint Surg Br 89(4): 510-515.
- Ruchelsman DE, Tejwani NC, Kwon YW, Egol KA (2008) Coronal plane partial articular fractures of the distal humerus: current concepts in management. J Am Acad Orthop Surg 16(12): 716-728.
- Giannicola G, Sacchetti FM, Greco A, Gregori G, Postacchini F (2010) Open reduction and internal fixation combined with hinged elbow fixator in capitellum and trochlea fractures. Acta Orthop 81(2): 228-233.
- Singh AP, Singh AP, Vaishya R, Jain A, Gulati D (2010) Fractures of capitellum: a review of 14 cases treated by open reduction and internal fixation with Herbert screws. Int Orthop 34(6): 897-890.
- Elkowitz SJ1, Polatsch DB, Egol KA, Kummer FJ, Koval KJ (2002) Capitellum fractures: a biomechanical evaluation of three fixation methods. J Orthop Trauma 16: 503-506.
- Giannicola G, Polimanti D, Sacchetti FM, Scacchi M, Bullitta G, et al. (2012) Soft tissue constraint injuries in complex elbow instability: surgical techniques and clinical outcomes. Orthopedics 35: e1746-1753.






























