Restoration of Large and Massive Rotator Cuff Tears with Arthroscopic Technique
Andreas X Papadopoulos*, George E Chatzimarkakis and Athanassios Ch Karageorgos
Department of Orthopaedic Surgery, Olympion Medical Center, Patras, Greece
Submission: April 17, 2019;;Published: April 29, 2019;
*Corresponding author: Andreas X Papadopoulos, Department of Orthopaedic Surgery, Olympion Medical Center, Patras, Greece
How to cite this article: Andreas X P, George EC, Athanassios CK. Restoration of Large and Massive Rotator Cuff Tears with Arthroscopic Technique. Ortho & Rheum Open Access J 2019; 14(1): 555878. DOI:10.19080OROAJ.2019.14.555878
Abstract
Purpose: The evaluation of the clinical results and the integrity of the tendon reconstruction after arthroscopic treatment of patients with large or massive rotator cuff rupture.
Methods: This is a retrospective study, with a minimum postoperative follow-up of 24 months, of 134 patients (74 men and 60 women, mean age of 58 years), with large or massive rotator cuff tear. They were patients with a rupture of one or two tendons and a subsequent gap of more than 2 cm in the coronary MRI views (C3 and C4 according to Snyder classification), with incidence of a tendon stump at least at the level of the humeral head (stage 2 and 3 according to Patte), without severe osteoarthritis. The surgical technique involved preparation, mobilization, suturing and fixation, in a single row pattern, by means of bone anchors of the tendon abutments at the anatomical insertion site on humerus head neck.
Results: The suture integrity was checked either by ultrasound scanning or magnetic resonance imaging, and on evaluation, the rates of sound healing and partial or full re-rupture incidence were 75%, 12% and 3%, respectively. Clinical results were satisfactory, concerning final postoperative outcome over preoperative pain assessment (mean VAS pain scoring from 6.2 to 0.88), functionality (mean VAS scoring from 4.32 to 8.8) as well as the ASES questionnaires (from 42.3 to 86.2) and the Constant score (from 42.7 to 82.5).
Conclusion: The arthroscopic investigation and treatment of patients with large and massive rotator cuff tear, that meet the criteria for this type of intervention is a minimally invasive and very effective method that provides satisfactory results in terms of pain, functionality and anatomical restoration of the damage.
Level of evidence II
Keywords: Shoulder arthroscopy; Large – massive rotator cuff tear
Introduction
The way to deal with large or massive rupture of the rotator cuff has been proved in the recent years to be a field of reflection, research and development of particularly demanding surgical techniques. The development of arthroscopic surgery in conjunction with the continuous technological refinement of arthroscopic devices, tools and materials, as well as the better understanding of the biomechanical function and the role of the rotator cuff in centering the humerus head to the glenoid fossae, stimulated the concept of approaching these ruptures with more emphasis to the logic of the ‚anatomical restoration‘ of the tendon damage [1].
The term „non-repairable lesion“ that very often follows a magnetic resonance imaging report with the stump of the supraspinatus muscle tendon close to the anatomic level of the glenoid, can eventually correspond to a fully or partially repairable anatomic lesion that adequately responds to the functional demands of the rotator cuff tendons [2,3]. Thus, the use of advanced arthroscopic means and techniques for the relaxation, mobilization and fixation of the tendon stump can prevent the need of more demanding and expensive interventions such as reconstruction with upper capsular substitutes or a reverse total shoulder arthroplasty [4].
Materials and Methods
From 2008 to 2016, in our clinic 134 patients with a large or massive rupture of the rotator cuff were treated by the same operative team. They were patients with a rupture of one or two tendons with a subsequent gap of more than 2 cm in the coronary MRI views (C3 and C4 according to Snyder classification), with incidence of a tendon stump at least at the level of the humeral head (stage 2 and 3 according to Patte). In total 74 men and 60 women with a mean age of 58 years, were treated. In 88% of the cases the rupture was of a chronic pattern character with clinical evidence of pain and muscle weakness, while in 12% of the cases the rupture was due to acute trauma. In 18 patients there was a concomitant partial or total rupture of the subscapularis tendon. When selecting patients for this surgical technique, those suffering from advanced shoulder arthritis, chronic humerus head migration at the level of the acromion with severe decrease of the subacromial space (Rotator Cuff Arthropathy), and patients with chronic inability to anterior abduction of upper limb (pseudo-paralysis) were excluded. Scheduled hospitalization period was up to 24h. A 10-month rehabilitation regime was then followed.
Surgical Technique
Under general anesthesia, the patient is placed on the surgical table in a ‘beach chair’ position with the head resting on a special headrest, removing the bed section under the shoulder area. After prepping and draping accordingly the shoulder, and the whole upper limb areas with subsequent placement of a special sterile arthroscopic bed sheet, hand and distal arm half are kept under appropriate sterile stockinette and elastic bandage. Then, the connection to the arthroscopic tower (camera, cold light cable, shaver, arthroscopic diathermy device) takes place. Intra-articular pressure on the shoulder is ensured at a constant level (60 - 75 mmHg) via an arthroscopic water pump distention system. The patient‘s blood pressure is adjusted by the anesthesiologist and maintained at low levels (controlled hypotension) by means of intra-arterial recording to achieve intraoperative hemostasis and clarity of the arthroscopic field and image.
Initially, the primary posterior intra-articular portal is to be placed, though which the arthroscopic optic fiber (30 degrees - 4mm) is inserted and subsequently the glenohumeral joint is overviewed. Then, an anterior-superior portal is made in the rotator interval, under the long head of the biceps, under direct intra-articular vision. The long head of the biceps is given an overview securing that if eventually deteriorated, an arthroscopic tenotomy is to be made at its insertion at the level of the upper pole of the glenoid and its full removal from the articulation field is to be secured. Capsular release and its relaxation, labral debridement and chondroplasty are also performed accordingly.
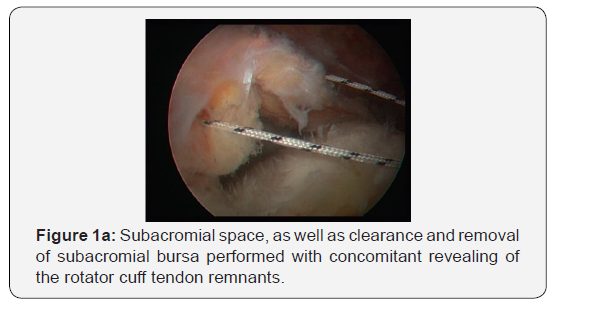
Next step is to check the anatomical integrity of subscapularis muscle tendon and its insertion upon the lesser tuberosity. In the unfortunate event of a rupture (partial or total), a reattachment to the original humeral insertion is to take place. Initially, an anterior-inferior arthroscopic portal placement is performed. We then insert an arthroscopic anchor armed with 2 suture filaments and, by means of a specifically designed passer, sutures are passed through the tendon. By arthroscopic knots, the tendon stump is then clamped to the region of the lesser brachial tuberosity, at the point of the bone anchor. Thereafter, the arthroscope is inserted into the sub-acromial space through a posterior-lateral portal. Overview of the subacromial space, as well as clearance and removal of subacromial bursa is then performed with concomitant revealing of the rotator cuff tendon remnants (Figure 1a). Acromioplasty then follows, as well as removal (if necessary) of the eventual osteophytic lateral edge of the clavicle. Preparation (debris clearance and mild reaming) is thereafter carried out at the area of the anatomical tendon insertion on humerus (footprint).
Subsequently, the mobility of the tendon struts is checked. With an arthroscopic tendon grasper, the tendon edge is pulled and the direction of elasticity and the possibility of reattachment without exercising excessive tension to the insertion site (anatomic footprint), is evaluated. In the case of massive chronic ruptures, the stump of the supraspinatus and/or part of the subscapularis muscles tendons are unfortunately close to the glenoid level, a fact that often renders impossible any attempt to re-approximate them to the point of fixation. In such situations, tissue mobilization is attempted by means of arthroscopic diathermy and specially designed rasps, under direct vision through the arthroscope, beneath the tendon stump and between the tendon and the upper glenoid pole, until the base of the coracoid apophysis (coraco-brachial ligament release). If the tendon stump is adequately mobilized, its mobility and the morphology of the tissue deficit are then re-evaluated.
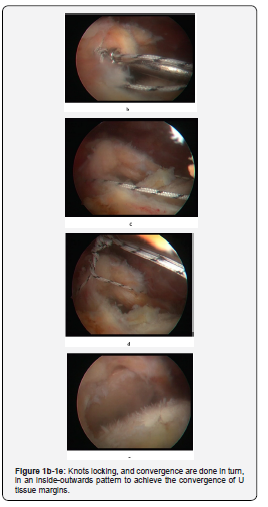
If again the tendons margin lips cannot be easily approached at the fixation point (large U-defects), side to side margins convergence is attempted. In this way, by using 2-4 simple sutures, we can reduce the tendon deficit by more than 50% (to reproduce a smaller U deficit). Entering the arthroscope through the lateral subacromial portal, polyclonal non-absorbable sutures through the posterior and the anterior tendon margins (U limbs) are passed by the tendon passer. Knots locking, and convergence are done in turn, in an inside-outwards pattern to achieve the convergence of U tissue margins (Figure 1b-1e).
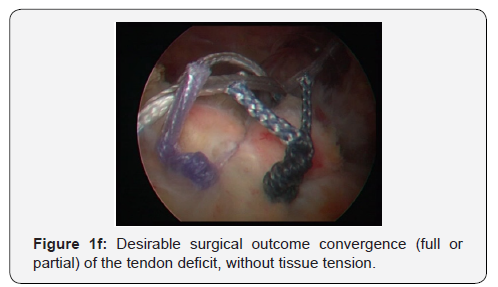
Finally, we place 1 to 3 non-metallic bone anchors loaded with 2 or 3 non-absorbable sutures in the anatomical tendon insertion on humeral head (or slightly inwards - medialization up to 10 mm). By using the special tendon passer, each suture passes through the free edge of the tendon stump. Beginning the suture passage medially (infraspinatus or teres minor muscles area) moving laterally, an attempt is made to alternately place single and double (mattress) sutures in a single row. The final knot locking is performed following the same manner. The desirable surgical outcome is the convergence (full or partial) of the tendon deficit, without tissue tension (Figure 1f). The shoulder position during the whole suturing phase is to be kept neutral (without abduction). The operation is completed by suturing arthroscopic cutaneous portals with single nylon 3-0 sutures and the upper limb is then placed in suspension while on light abduction.
Results
During arthroscopic examination, degeneration changes of biceps brachii long head tendon were detected in almost all cases and arthroscopic tenotomy at the glenoid level was carried out in all cases that automatic rupture had not preceded. Acromioplasty and clearance of the subacromial space was as well performed in all patients, while removal of the lateral clavicular head due to degenerative issues occurred in 38% of the cases. The mean length of the medio-lateral tissue deficit was 3.8 cm. Margin convergence by means of lateral suture placement was done in 48 patients (35.8%). Partial close of the deficit was achieved in 22 patients (16.4%).
Minimum follow-up regimen of patients was 24 months. In terms of suture integrity (by Ultrasound or MRI Scan), healing rates, as well as partial or full re-rupture rates were 75%, 12% and 3%, respectively. As for clinical outcomes, there was a great improvement over preoperative pain assessment (mean VAS pain score from 6.2 to 0.88), functionality (mean functionality VAS score from 4.32 to 8.8) as well as the ASES questionnaires (from 42.3 to 86.2) and the Constant Score (from 42.7 to 82.5). Active anterior elevation improved on average from 148.6 to 170.8 degrees, while the average enhancement of active external rotation was 15.3 degrees.
Discussion
The gradual disruption of the rotator cuff tendons integrity, because of a chronic impingement syndrome, can lead to anatomical destruction and functional deficiency of one or more of the rotator cuff tendons. This results in both muscle insufficiency and gradual fatty infiltration of the corresponding muscle, whose tendon is disturbed, but also results in the general disruption of the stability and concentricity of the shoulder joint at the glenoid level. An intact rotator cuff constitutes a powerful glenohumeral stabilizer concentrating the humeral head to the glenoid [5,6]. Progressive migration of the humeral head towards the acromion and subsequent occlusion of the subacromial space because of a large tissue deficit and functional deficiency of 2 or more rotator cuff tendons leads to mechanical disturbance of the range of motion, deltoid muscle disfunction, pseudo-paralysis and rotator cuff arthropathy [7,8]. Arthroscopic reconstruction of the large rotator cuff ruptures is becoming one of the most demanding surgical techniques that has been developing with continuous technical variations in the last few years trying to provide with functional solutions to a major anatomical and functional impairment of the shoulder joint [1].
The ideal goal of a surgical intervention in a middle aged or older but functional patient without evidence of severe osteoarthritis in the shoulder joint, who suffers from a large and possibly unrecoverable damage to the rotator cuff, is to achieve a painless and functional shoulder with a large and active range of motion. The development of knowledge, materials and arthroscopic technique renders this aim feasible in most cases by performing purely arthroscopic surgery and by applying surgical techniques greatly limiting the need for more open surgical procedures such as tendon transfers, use of tendon substitutes and eventual shoulder replacement surgery [9]. This often seems quite impossible and difficult to assess preoperatively with imaging methods. Thus, in many cases, reverse shoulder arthroplasty or tendon transfer is selected from the outset, with the well-known rates of early or delayed post-operative complications. However, the arthroscopic investigation of the remaining rotator cuff usually reveals possibilities for an anatomical restoration at a rate sufficient to achieve, first the maintenance of the external rotation and, secondarily, the focusing of the humeral head on the glenoid fossae, fact that ensures the ideal biomechanical conditions allowing the application of the deltoid forces and thus movement of the hand over the shoulder level [4].
In cases where, during the initial arthroscopic control, the tendon stump is quite inelastic and stiff and cannot be attracted gently to the area of the anatomic fixation, release around the tendon needs to be performed. This procedure becomes particularly effective when the release extends to the base of the coracoid process, between the supraspinatus tendon stump and glenoid, performing a cross-section of the coracobrachial ligament. This can also be combined with interval slides, which were quite popular since the 1990s [10-13], but subsequently appeared to lead (especially the posterior interval slide between supra- and infra-spinatus) to tendon perfusion disorder, ischemic necrosis and re-rupture in the first post-op semester [14,15]. Therefore, it is also considered by us to be effective and safe for the tendon viability to mobilize the tendon stump by sectioning and, thus, loosening of the coraco-brachial ligament at the base of coracoid process, without additional interval slides, technique that provides satisfactory mobility to the tendon without disturbing its perfusion.
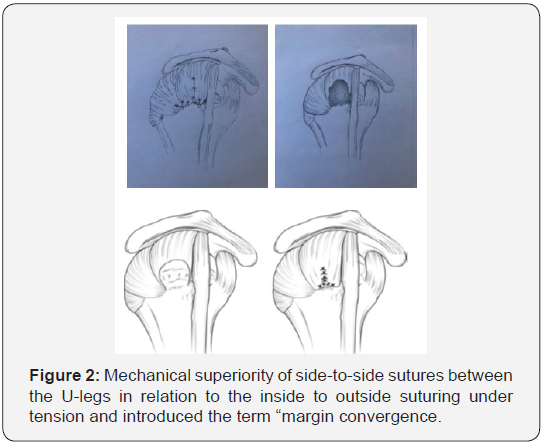
Assessing and evaluating the mobility of the tendon stump after its release, is crucial and vital for taking the most appropriate intraoperative decision on how to converge the margins of the tendon deficit. For the large U-type deficiencies, the difficulty or insufficiency of pulling without exercising excessive tension on the central U part attempting to move it towards the anatomical footprint point is clearly highlighted. Burkhart [5,16,17] depicted the mechanical superiority of sideto- side sutures between the U-legs in relation to the inside to outside suturing under tension and introduced the term „margin convergence“ (Figure 2). In this way the length of the rupture gradually decreases while increasing the cross-sectional area of the stump. This reduces the tension for the tendon stump to settle on the bone as the lateral sutures act protectively reinforcing the tendon stump strength [18,19]. In theory, this may also increase the likelihood of healing, as shown by post-operative ultrasound studies [20].
In cases where despite the tendon mobilization techniques its length does not meet the requirements for suturing without tension to the anatomical footprint, if the suturing is performed under tension re-rupture rate increases [4]. It is preferable and safer to perform fixation slightly inwards (medialization) by sutures in a single row without tension, rather than by sutures in a double row under tension. It appears that fixation of up to 10 millimeters medially than footprint does not disturb the biomechanics during the anterior arm elevation [21-23], while if it exceeds 17 millimeters, there is a negative effect due to a significant reduction of the lever arm [24]. Therefore, in cases where the convergence is rather technically demanding, the inward fixation of up to 10 millimeters is an acceptable bibliographic option in any reconstructive attempt to fix the tendon stump under no tension [25,26].
It is, thus, apparent from the literature, a fact we also realized in the treatment of our patients, that the decision which method to choose for dealing with large and possibly unrecoverable ruptures should ultimately be taken, in several cases, intraoperatively during the arthroscopic investigation. Only this way can the shoulder surgeon investigate exhaustively all possibilities of functional anatomical recovery, before deciding that this is impracticable and thus requires some other type of surgery. Evolution of arthroscopic technique, materials, and personal surgical training progress of each surgeon can give functional results to apparently non-repairable shoulder issues.
Conclusion
Arthroscopic treatment of patients with large and massive rotator cuff tears that meet the criteria for this type of intervention is a minimally invasive and at the same time very effective method that yields satisfactory results in terms of pain, functionality and anatomical repair of the lesion. The use and improvement of arthroscopic techniques of tendon mobilization and release, marginal convergence, and medialized fixation are useful and documented interventions that facilitate fixation without tendon tissue tension and lead to the conversion of difficult and unrecoverable damages to biomechanical and biologically correct fixations.
Compliance with Ethical Standards
Conflict of Interest: Author A, Author B, and Author C declare that they have no conflict of interest.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Ethical approval: The study was approved by the ethical committee of the institute.
Informed consent: The patients were informed, and they consented to conduct the study.
References
- Anley CM, Chan SK, Snow M (2014) Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthop 5(5): 557-565.
- Berth A, Neumann W, Awiszus F, Pap G (2010) Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 11(1): 13-20.
- Iagulli ND, Field LD, Hobgood ER, Ramsey JR, Savoie FH 3rd (2012) Comparison of partial versus complete arthroscopic repair of massive rotator cuff tears. Am J Sports Med 40(5): 1022-1026.
- Henry P, Wasserstein D, Park S, Dwyer T, Chahal J, et al. (2015) Arthroscopic repair for chronic massive rotator cuff tears: A systematic review. Arthroscopy 31(12): 2472-2480.
- Burkhart SS (2004) The principle of margin convergence in rotator cuff repair as a means of strain reduction at the tear margin. Ann Biomed Eng 32(1): 166-170.
- Parsons IM, Apreleva M, Fu FH, Woo SL (2002) The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res 20(3): 439-446.
- Su WR, Budoff JE, Luo ZP (2009) The effect of anterosuperior rotator cuff tears on glenohumeral translation. Arthroscopy 25(3): 282-289.
- Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL (2004) Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am 86(suppl 2): 35-40.
- Galasso O, Riccelli DA, De Gori M, De Benedetto M, Orlando N, et al. (2017) Quality of life and functional results of arthroscopic partial repair of irreparable rotator cuff tears. Arthroscopy 33(2): 261-268.
- Berdusco R, Trantalis JN, Nelson AA, Sohmer S, More KD, et al. (2015) Arthroscopic repair of massive, contracted, immobile tears using interval slides: clinical and MRI structural follow-up. Knee Surg Sports Traumatol Arthrosc 23(2): 502-507.
- Bigliani LU, Cordasco FA, McLlveen SJ, Musso ES (1992) Operative repair of massive rotator cuff tears: long-term results. J Shoulder Elbow Surg 1(3): 120-130.
- Lo IK, Burkhart SS (2004) Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy 20(1): 22-33.
- Tauro JC (1999) Arthroscopic "interval slide" in the repair of large rotator cuff tears. Arthroscopy 15(5): 527-530.
- Kim SJ, Kim SH, Lee SK, Seo JW, Chun YM (2013) Arthroscopic repair of massive contracted rotator cuff tears: aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Joint Surg Am 95(16): 1482-1488.
- Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM (2012) Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy 28(6): 761-768.
- Burkhart SS, Athanasiou KA, Wirth MA (1996) Margin convergence: a method of reducing strain in massive rotator cuff tears. Arthroscopy 12(3): 335-338.
- Burkhart SS, Nottage WM, Ogilvie-Harris DJ, Kohn HS, Pachelli A (1994) Partial repair of irreparable rotator cuff tears. Arthroscopy 10(4): 363-370.
- Mazzocca AD, Bollier M, Fehsenfeld D, Romeo A, Stephens K, et al. (2011) Biomechanical evaluation of margin convergence. Arthroscopy 27(3): 330-338.
- Oh JH, McGarry MH, Jun BJ, Gupta A, Chung KC, et al. (2012) Restoration of shoulder biomechanics according to degree of repair completion in a cadaveric model of massive rotator cuff tear: importance of margin convergence and posterior cuff fixation. Am J Sports Med 40(11): 2448-2453.
- Shindle MK, Nho SJ, Nam D, Macgillivray JD, Cordasco FA, et al. (2011) Technique for margin convergence in rotator cuff repair. HSS J 7(3): 208-212.
- Cole BJ, ElAttrache NS, Anbari A (2007) Arthroscopic rotator cuff repairs: An anatomic and biomechanical rationale for different suture-anchor repair configurations. Arthroscopy 23(6): 662-669.
- Domb BG, Glousman RE, Brooks A, Hansen M, Lee TQ, et al. (2008) High-tension double-row footprint repair compared with reduced-tension single-row repair for massive rotator cuff tears. J Bone Joint Surg Am 4: 35-39.
- Liu J, Hughes RE, O'Driscoll SW, An KN (1998) Biomechanical effect of medial advancement of the supraspinatus tendon: a study in cadavera. J Bone Joint Surg Am 80(6): 853-859.
- Kim YK, Jung KH, Won JS, Cho SH (2017) Medialized repair for retracted rotator cuff tears. J Shoulder Elbow Surg 26(8): 1432-1440.
- Yamamoto N, Itoi E, Tuoheti Y, Seki N, Abe H, et al. (2007) Glenohumeral joint motion after medial shift of the attachment site of the supraspinatus tendon: a cadaveric study. J Shoulder Elbow Surg 16(3): 373-378.
- Burkhart SS (1992) Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears: a suspension bridge model. Clin Orthop Relat Res 284: 144-152.






























