A Study of The Management of Distal Radius Fractures as Per AO Classification in A Tertiary Care Centre
Nandu R Baby1* and P Saravanan2
1Postgraduate, Department of Orthopedics, Sri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth, India
2Assosciate professor, Department of Orthopedics Sri Sathya Sai Medical College and Research Institute, Sri Balaji Vidyapeeth, India
Submission: March 14, 2019;Published: April 08, 2019
*Corresponding author: Nandu R Baby, Sri Sathya Sai Medical College and Research Institute, Sri balaji Vidyapeeth Ammapettai, Kancheepuram, Tamil Nadu, India
How to cite this article: Nandu R B, P Saravanan. A Study of The Management of Distal Radius Fractures as Per AO Classification in A Tertiary Care Centre. Ortho & Rheum Open Access J 2019; 14(1): 555876. DOI: 10.19080/OROAJ.2019.14.555876
Abstract
Introduction: One of most frequently used classification system for distal radius fractures is the AO (Arbeitsgemeinschaft für Osteosynthesefragen) Classification which has nine chief subgroups. The prognostic and outcome worth of the classification, to assess the consequence of a fracture of distal radius may not be precise, particularly concerning inter- and intra-observer level of agreement. This is a descriptive study dealing with the association of the functional outcomes in AO type of fractures at the distal end of radius which are managed by various treatment modalities and DASH score.
Methods: This is a descriptive study showing the association of AO type of distal end radius fractures treated with various modalities with DASH score, study subjects were 50 patients with fracture of distal radius of distal radius of age ranging between 18 - 80 years who visited our tertiary care centre in Ammapettai from May 2017 to September 2018.
Results: The study subject who scored between 0-16 were classified as Excellent, 17 to 35 were classified as good and above 35 were classified as fair According to this classification 74% had excellent outcomes followed by 16% of study subjects who had good outcome and only 16% had fair clinical outcome based on DASH scoring. Our study results point towards good outcome subsequent to a fracture of distal radius fractures.
Conclusion: The proportion of study subjects with an adverse consequence has not undergone any change. There could be several reasons to this lack of change over the decade. The tool may not be sensitive enough or catering to minimal changes. Sometimes the DASH-score for study subjects with bad outcome has already reached its limit, and hence these study subjects would have ended up with bad outcome irrespective of management due to coexisting illness or any other psychological reasons, or the reason which is most unacceptable, that is the modification in management merely has no outcome.
Keywords: Distal end radius fractures; AO classification of distal radius fractures; DASH Score
Introduction
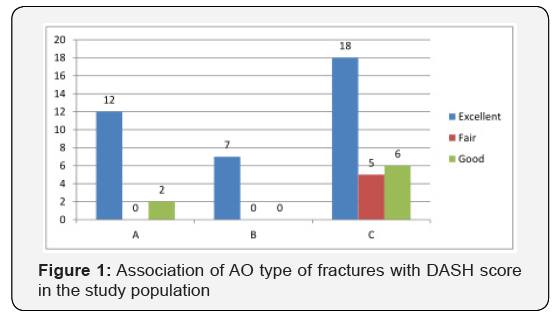
The distal radial fractures account for about 15 to 20% of total fractures managed by an Orthopaedic surgeon [1]. Many studies on this topic have been done earlier with reverence to the association between various management modalities of fractures of distal radius and functional outcomes [2]. The findings of these studies have most often presented no correlation between the two factors. Distal radial fracture is common in females above 50 years of age [3]. Two of the most frequently used were the AO (Arbeitsgemeinschaft für Osteosynthesefragen) Classification which had nine chief subgroups and the Frykman classification which had 8 subgroups [4]. The prognostic and outcome worth of these classifications, to assess the consequence of a fracture of distal radius may not be precise [5], particularly concerning inter- and intra-observer level of agreement [6]. This is a descriptive study dealing with the association of the functional outcomes in AO type of fractures at the distal end of radius which are managed by various treatment modalities and DASH score (Figures 1 & 2).

Materials and Methodology
This is a descriptive study showing the association of AO type of distal end radius fractures treated with various modalities with DASH score, study subjects were 50 patients with fracture of distal radius of distal radius of age ranging between 18 - 80 years who visited our tertiary care centre in Ammapettai from May 2017 to September 2018.
Inclusion Criteria
i. Study subjects in the age group of 18-45 years of either gender.
ii. Study subjects presenting with intra-articular unstable fracture of distal radius with acute injury.
iii. The existence of an unstable fracture of distal radius, with antero-posterior (AP) and lateral X-rays
Exclusion Criteria
a. Extra-articular and stable fractures of distal radius
b. The existence of medical disorders with an influence on bone physiology and another ipsilateral fracture
c. Severe medical co morbid conditions.
d. Polytrauma
Study Groups
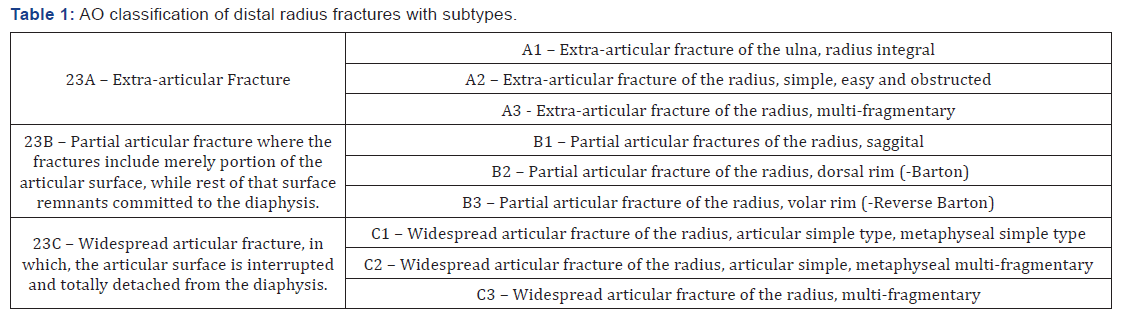
The Swiss Association for the Study of Internal Fixation (AO/ ASIF) assembly established the “Comprehensive Grouping of Fractures of Long Bone” to function as a basis for management and assessing consequences [7]. The distal radius and ulna were explained as “2 3” and is additionally categorized into 3 types. Each type is again categorized into three groups and further each group into three subgroups. The lone alteration matched to the AO system was the adding of the „die-punch“ fracture to the incomplete articular fractures assembly Radiographic imaging is essential for diagnosis, categorization, and management and follows up assessment of these type of fractures.
The considerations measured include angulation or inclination of the radius – is the comparative angle of the distal radial articular surface to a line perpendicular to the long alignment of the radial shaft. This averages 23 degrees (range, 13 to 30 degrees), length of the radius – relates the length of the radius to the ulna by space stuck between two perpendicular lines to the long axis of the radius, one connecting the tip of the radial styloid process and the further, the surface of ulnar head. This be an average of 11 mm (range, 8 to 18 mm),variance of ulna – is the vertical space between the distal ends of the medial angle of the radius and the ulnar head, width of the radius – the dislocation of distal fragment in relation to the radial shaft and is measured as the space between the longitudinal axis through the middle of radius and the most adjacent point of the radial styloid process.
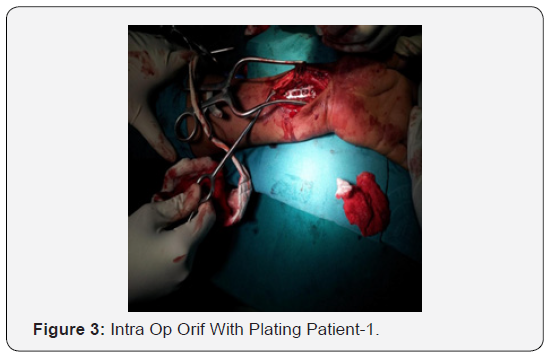
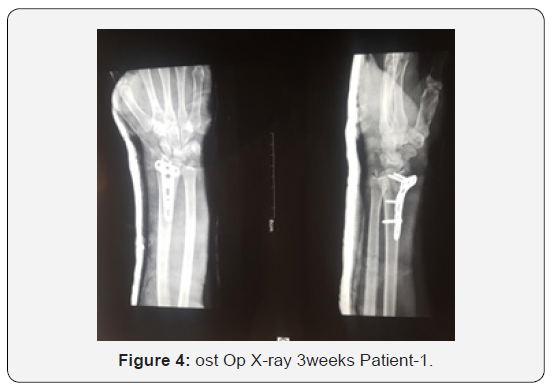
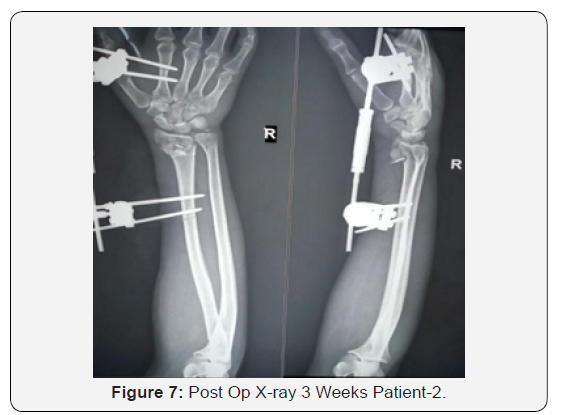
Guiding principle for satisfactory closed reduction as given by Nana A D et al. in the year 2005 comprise [8], radial leaning: ≥150 on the postero-anterior outlook. radial span: ≤5 mm shortening on postero-anterior outlook. radial Angle : <150 dorsal or 200 volar tilt on lateral outlook. Articular inconsistency: <2 mm of step off (Figures 3 & 4). radiographic signs that ready to act the surgeon, that the fracture is perhaps unbalanced and closed reduction alone will be inadequate, which further include as the following: dorsal comminution > 50% of the thickness sideways, palmar metaphyseal comminution, initial dorsal slope > 20 degrees, initial dislocation (fragment translation) > 1 cm, Initial radial shortening > 5 mm, intra-articular commotion, related ulna fracture, severe osteoporosis. The management options for fractures of distal radius has always been in changed and improvised from cast immobilization to open reduction & internal fixation using locking compression plates. Study subjects were included in groups according to AO types of fractures with the management of choice (Figure 5).

Methodology
Study subjects include 50 individuals who comes under the inclusion criteria, who undergoes various treatment modalities depending on the AO type of fracture at a tertiary care centre in Ammapettai with a follow-up of 2 weeks , 6 months and 1 year Initial Assessment: The initial characteristics of the injury were recorded, including the type of accident, the energy level, and the type of fracture according to the AO classifications [7], and the associated soft tissue injuries at the fracture site. AP and lateral X-rays were obtained of each study subject at the time of admission, immediately after the treatment provided and during the follow-up visits. The radiologic features were measured, and the fracture stability, according to the Altissimi [9] and Fernández [10] criteria and the treatment provided were recorded, the association of functional outcome in AO type of fractures managed with various managements and DASH score has been tabulated and projected in a bar diagram. Institutional ethical committee clearance was obtained (IEC No:2017/310)
Procedures
Closed Reduction
Closed reduction [11] and plaster cast application [12] is the main treatment for undisplaced fractures, minimally displaced fractures and bending fractures in good bone. Percutaneous pinning [13-15]: Closed reduction and percutaneous pinning is carried out when: Displaced extra articular fractures with or without Dorsal Communition, early loss of reduction after closed reduction, communited intra articular fractures when adequate closed reduction is able to obtain but likely not maintained without additional support.
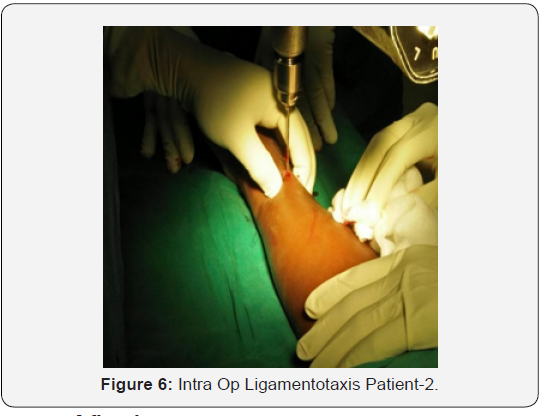
External fixation/Ligamentotaxis:
Bridging external fixation typically relies on the principle to obtain and maintain a reduction of fracture fragments. As longitutional Traction is applied to the carpus [16], the tension is transmitted mostly through radioscaphocapitate and long radiolunate ligaments to restore radial length mainly used for: extra articular fractures with an unstable metaphysis, intra articular radial styloid fractures, intra articular fractures with depression or communition.
Internal fixation
The ability to hold both large extra articular fragments as well as small Intra articular fragments is necessary in many complex fractures. Internal fixation with Ellis buttress plates or Volar locking plates is done [17]. Works by biomechanical principle of external fixator, does not require friction between plate and bone, locking plates are precontoured for anatomical fit, locking screws offer a fixed angle construct to support the articular surface and to obtain good fixation in osteoporotic bone.
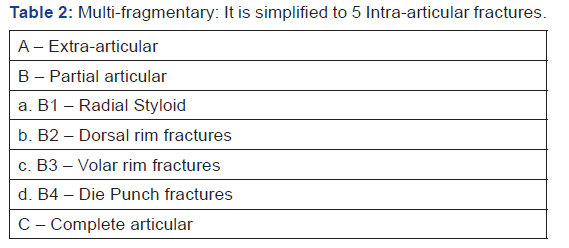
Follow-up Interview: The study protocol was patient oriented which implemented with the application of a questionnaire 2 weeks, 1month, 6months and up to one year after treatment was provided; the questionnaire is applied during the follow-up visit or by telephone. The functional result was calculated using the DASH questionnaire [18]. All adverse effects were documented throughout the duration of the study. The radial angle, the radial height, the ulnar variance was evaluated in the AP X-rays. The volar tilt angle, and the presence of a step off or articular gaps were evaluated in the lateral X-rays. These measurements were made according to the criteria by Kreder et al. [6]. The association of AO fracture types in distal radius fractures with DASH score have been tabulated and projected in a bar diagram (Tables 1 & 2).
Results
Results of this study are described under the following headings:
i. Descriptive statistics.
ii. Inferential statistics.
iii. Descriptive statistics:
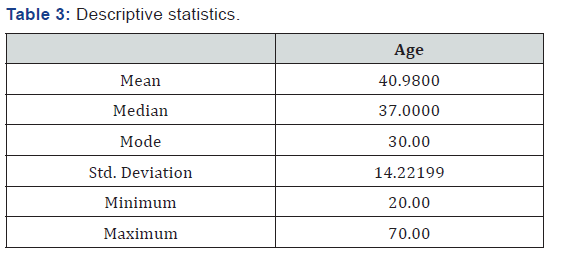
Age: The Mean age of the study population is 40.9800, with Median being 37.0, Mode being 30.00,
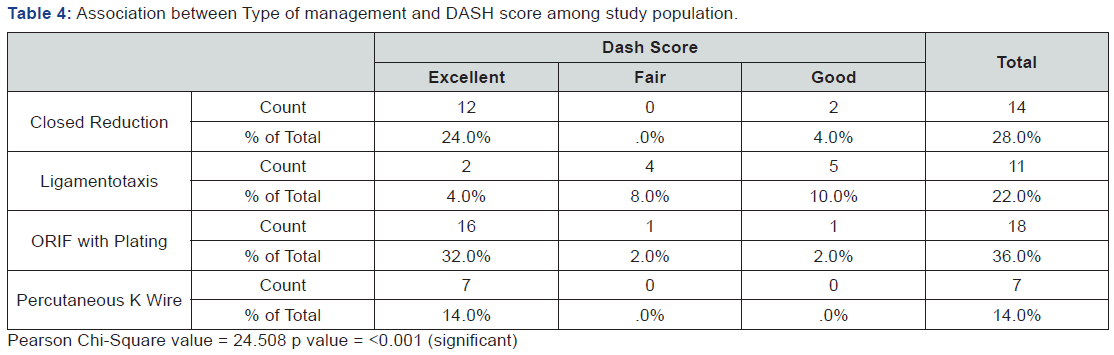
Pearson Chi-Square value = 24.508 p value = <0.001 (significant)
Std. Deviation is 14.22199, Minimum value being 20.00 and Maximum value being 70.00. This is represented in Table 3. Cross tabulation of DASH score and Type of Management is done in Table 4. The association between type of management and DASH score. There is a significant association between those who had ORIF with plating as type of management and excellent DASH score have been tabulated in Table 4. The association between AO type of fractures at the distal end of radius and DASH score is tabulated in Table 5. The bar diagram Figure 1 shows that majority 18(62.07%) of those who had C type of AO type fracture were having excellent DASH score .
Discussion
According to AO classification the injury profile in our study is classified into three types namely extra articular, partially articular and completely articular. In our study it was found that 29% of the subjects had completely articular fracture which is the major type in our study group followed by 14% of the study subjects with extra articular fractures and only 7% had completely articular fractures. In our study majority of the study subjects about 18% were managed with procedure of open reduction & internal fixation with volar plating, 14% of the study subjects were managed by closed reduction, 11 % were managed by closed reduction and internal fixation and finally about 7% were managed with open reduction & internal fixation with volar or dorsal plating. The outcome measure was analysed using DASH scoring. The study subject who scored between 0-16 were classified as Excellent, 17 to 35 were classified as good and above 35 were classified as fair According to this classification 74% had excellent outcomes followed by 16% of study subjects who had good outcome and only 16% had fair clinical outcome based on DASH scoring. Our study results point towards good outcome subsequent to a fracture of distal radius (DRF). Compared to other studies done which showed a median DASH score of 19 at 6 months [19], which estimates a moderate disability according to the DASH definition. Another study shows at 6 months, 68% of the study subjects have minimal pain [20]. After 12 months, the participants had minimal pain and better function with fewer limitations in their activities of daily living [20], and a DASH score of 8.5 at 12 months [19]. Approximately 16−20% participants complained about modest to most important disability even 12 months after the injury, which is not a very favourable outcome measure of a distal end radius fractures treatment. Further it appears that only a little proportion of the study subjects with major disability after one year will revert back to pre-fracture position in the long- standing.

The occurrence of DRF in European countries seems to have decreased after the turn of the 20th century because of unknown reasons. The life expectancy also tends to increase for both male and female and the whole quantity of fractures [21,22]. So it is a common expectation that fracture also increase and the societal burden should increase as well. In India the population is increasing, the number of vehicles is increasing and consequently the incidence of radial fractures is on the increasing trend. The management of a distal end radius fractures has been varied and in the last decade with recent procedures with a greater quantity of study subjects being managed through surgical treatment [3,23-25] it expected that the outcome should have advanced significantly, at least for the group treated with surgery. we have found some limitations of follow up of these patients and further analysis of the results with the details of complication and union with regard to various treatment modalities in distal radius fractures can yield a better result, the sample size is small, not a representative of the general population hence may limit the application to general population.
Conclusion
The proportion of study subjects with an adverse consequence has not undergone any change. There could be several reasons to this lack of change over the decade. The tool may not be sensitive enough or catering to minimal changes. Sometimes the DASHscore for study subjects with bad outcome has already reached its limit, and hence these study subjects would have ended up with bad outcome irrespective of management due to coexisting illness or any other psychological reasons, or the reason which is most unacceptable, that is the modification in management merely has no outcome.
References
- Rockwood, Charles A, David P Green, Robert W Bucholz (2010) Rockwood and Green's Fractures in Adults. (7th edn), Wolters Kluwer Health/Lippincott Williams & Wilkins, Philadelphia, PA, USA.
- Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am 89(9): 2051–2062.
- Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, et al. (2006) Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am 88(12): 2687-2694.
- Frykman G (1967) Fracture of the distal radius including sequelae--shoulder- hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function. A clinical and experimental study. Acta Orthop Scand Suppl 108: 3+.
- Flinkkilä T, Raatikainen T, Hämäläinen M (1998) AO and Frykman’s classifications of Colles’ fracture. No prognostic value in 652 patients evaluated after 5 years. Acta Orthop Scand 69(1): 77–81.
- Kreder HJ, Hanel DP, McKee M, Jupiter J, McGillivary G, et al. (1996) Consistency of AO fracture classification for the distal radius. J Bone Joint Surg Br 78(5): 726-731.
- Colles A (2006) On the fracture of the carpal extremity of the radius. Edinb Med Surg J 10:181. Clin Orthop 445: 5–7.
- Nana AD, Joshi A, Lichtman DM (2005) Plating of the distal radius. J Am Acad Orthop Surg 13(3): 159-171.
- Lindau TR, Aspenberg P, Arner M, Redlundh-Johnell I, Hagberg L (1999) Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand 70(2): 124–128.
- Mallmin H, Ljunghall S, Persson I, Naessén T, Krusemo UB, et al. (1993) Fracture of the distal forearm as a forecaster of subsequent hip fracture: a population-based cohort study with 24 years of follow-up. Calcif Tissue Int 52(4): 269-272.
- LaMartina J, Jawa A, Stucken C, Merlin G, Tornetta P (2015) Predicting alignment after closed reduction and casting of distal radius fractures. J Hand Surg 40(5): 934-939.
- Hove LM, Furnes O, Nilsen PT, Oulie HE, Solheim E, et al. (1997) Closed reduction and external fixation of unstable fractures of the distal radius. Scand J Plast Reconstr Surg Hand Surg. 31(2): 159–164.
- Atroshi I, Brogren E, Larsson GU, Kloow J, Hofer M, et al. (2006) Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: a randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop 77(3): 445–453.
- Krukhaug Y, Ugland S, Lie SA, Hove LM (2009) External fixation of fractures of the distal radius: a randomized comparison of the Hoffman compact II non-bridging fixator and the Dynawrist fixator in 75 patients followed for 1 year. Acta Orthop 80(1): 104–108.
- Rayhack JM, Langworthy JN, Belsole RJ (1989) Transulnar percutaneous pinning of displaced distal radial fractures: a preliminary report. J Orthop Trauma 3(2): 107–114.
- Cooney WP, Linscheid RL, Dobyns JH (1979) External pin fixation for unstable Colles’ fractures. J Bone Joint Surg Am 61(6A): 840–845.
- Orbay JL, Fernandez DL (2014) Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg 29(1): 96-102.
- Kennedy CA, Beaton DE, Solway S, McConnell S, Bombardier C (2011) Disabilities of the Arm, Shoulder and Hand (DASH). The DASH and QuickDASH Outcome Measure User’s Manual, (3rd Edn), Institute for Work & Health, Toronto, Ontario, Canada.
- Abramo A, Kopylov P, Geijer M, Tägil M (2009) Open reduction and internal fixation compared to closed reduction and external fixation in distal radial fractures: a randomized study of 50 patients. Acta Orthop 80(4): 478–485.
- MacDermid JC, Richards RS, Donner A, Bellamy N, Roth JH (2000) Responsiveness of the short form-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg 25(2): 330-340.
- Rosengren BE, Karlsson M, Petersson I, Englund M (2015) The 21st-century landscape of adult fractures: cohort study of a complete adult regional population. J Bone Miner Res Off J Am Soc Bone Miner Res 30(3): 535–542.
- Sigurdardottir K, Halldorsson S, Robertsson J (2011) Epidemiology and treatment of distal radius fractures in Reykjavik, Iceland, in 2004. Acta Orthop 82(4): 494–498.
- Adolphson P, Abbaszadegan H, Jonsson U (1993) Computer-assisted prediction of the instability of Colles’ fractures. Int Orthop 17(1): 13-15.
- Wilcke MKT, Abbaszadegan H, Adolphson PY (2007) Patient-perceived outcome after displaced distal radius fractures. A comparison between radiological parameters, objective physical variables, and the DASH score. J Hand Ther 20(4): 290-298; quiz 299.
- Mattila VM, Huttunen TT, Sillanpää P, Niemi S, Pihlajamäki H, et al. (2011) Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma 71(4): 939-942; discussion 942-943.






























