Mid-Term Results of Unicompartmental Knee Arthroplasty in Medial Compartment Osteoarthritis
Yusuf erdem1*, Cagri neyisci1, Bulent karslioglu2, Zafer atbasi3, Cemil yildiz1 and Mustafa basbozkurt1
1Orthopedics and Traumatology Department, Gulhane Training and Research Hospital, Turkey
2Orthopedics and Traumatology Department, Okmeydani Training and Research Hospital, Turkey
3Orthopedics and Traumatology Department, Guven Hospital, Turkey
Submission: January 30, 2019;Published: February 21, 2019
*Corresponding author: Yusuf Erdem, Orthopedics and Traumatology Department, Gulhane Training and Research Hospital, Turkey
How to cite this article: Yusuf erdem, Cagri neyisci, Bulent karslioglu, Zafer atbasi, et al. Mid-Term Results of Unicompartmental Knee Arthroplasty in Medial Compartment Osteoarthritis. Ortho & Rheum Open Access J 2019; 13(4): 555869. DOI: 10.19080/OROAJ.2019.13.555869.
Abstract
Background: The popularity of unicompartmental knee arthroplasty (UKA) for the treatment of isolated compartment osteoarthritis of the knee has risen over the past two decades. Currently, UKA covers a considerable amount of all knee arthroplasties worldwide. The aim of this study was to present the clinical and radiological outcomes of unicondylar knee arthroplasty in patients with medial compartment osteoarthritis.
Material and Methods: Between January 2010 and January 2014, unicondylar knee prosthesis was applied to 46 (3 men, 43 women) patients’ 56 knees with isolated knee medial gonarthrosis. The mean age of the patients was 54 (range 42 to 73), the body mass index was 26.3 (range 24 to 29) and the follow-up period was 48 months (range 20-84), respectively. patients were evaluated with Oxford Knee Score (OKS), Knee Society Score (KSS) and pain score (VAS) before and after surgery and evaluated radiologically by Oxford Radiological Evaluation Criteria.
Results: Compared to the preoperative values, the knee flexion increased from 116° to 123° (p<0.001). Statistically significant increase in OKS and KSS, and decrease in VAS was obtained postoperatively (p<0.001). All of the components were aligned within the acceptable ranges radiologically. In one patient, there have been an insert dislocation at 6th weeks postoperatively which was initially managed with closed reduction and then revised due tto redislocation. No major complications occurred including infection, deep vein thrombosis, pulmonary emboli, and neurovascular injury.
Conclusion: The mid-term clinical and radiological outcomes of UKA were excellent in this study, and our results demonstrate that UKA in proper indication is effective with considerable success in the treatment of medial compartmental knee osteoarthritis.
Keywords: Knee osteoarthritis; Unicompartmental knee arthroplasty; Medial compartment
Abbreviations: OA: knee Osteoarthritis; TKA: Total Knee Arthroplasties; HTO: High Tibial Osteotomy; TKA: Total knee arthroplasties; UKA: Unicompartmental knee Arthroplasties; OKS: Oxford Knee Score, KSS: Knee Society Score
Introduction
There is still controversy about the best treatment options for patients with medial compartment-involved knee osteoarthritis (OA). In cases of symptomatic medial compartment knee OA when conservative treatment is insufficient, correcting osteotomies such as high tibial osteotomy (HTO) and distal femoral osteotomy, total knee arthroplasties (TKA) or unicompartmental knee arthroplasties (UKA) are both utilized for surgical treatment [1-3]. Though TKA has been considered the gold standart of operative intervention for degenerative knee joint, many authors have shown better long term results for the latter choice, UKA, as well as good knee kinematics and function with lower complication rates. Beside this, preserving the healthy joint structures of the knee and replacing the degenerative compartment alone are the main reason for its rising popularity and led the technique to further increase of the applied frequency [3-5].
Since the first design was introduced by McKeever in 1957 [6], UKA technique had been developed with more anatomical implants and minimal invasive approach over the years. Marmor reported %10 revision rates in two-years follow-up and %65 survivorship with first design implants in UKA at a mean follow-up of ten years [7,8], while Goodfellow’s early results with Oxford phase II was reported by Murray as more than 90 % survivorship at ten years [9]. Increased success had been achieved by understanding the isolated anteromedial arthritis which is identified as bone cartilage loss in the anterior and mid portion of the medial compartment in association with intact ligamentous structures and normal lateral compartment cartilage [4,10] 17. In the late 1990s, more anatomical implants were manufactured and superior outcomes were yielded with these anatomical designs and mini-invasive surgical techniques. In a review, Khanna reported that 10-year survivorships have been increased ranging from %91 to %100 in most series with %93 survival rate in fifteen years [11]. In some similar studies, UKA survivorship, with the use of most recent implants, has demonstrated greater than %90 (ranging from %83 to %95) for more than 15-year follow-up [12,13]. These scientific publications, even with good long-term survival rates by the designer surgeons, induced the resurgence in UKA’s popularity over osteotomies and total knee artroplasties (TKA).
The purpose of this study was to assess the clinical and radiologic results, survival rates and complications of 56 knees with medial compartment OA treated consecutively with UKA implants.
Material and Methods
A written informed consent was obtained from each patient. The study protocol was approved by the Institutional Review Board. The study was conducted in accordance with the principles of the Declaration of Helsinki. 56 consecutive knees of 46 patients who underwent UKA due to isolated medial compartment osteoarthritis between January 2010 and January 2014 in our clinic were included with no loss to follow up. 43 patients (%93) were female and 3 (%7) were male. The mean age was 54 years (range, 42 to 73 years), mean follow-up was 48 months (range, 20 to 84 months) and mean BMI was 26.3 (range, 24 to 29). Patients demographic data are summarized in Table 1. All surgeries were performed and the data was collected by the senior surgeon. Patients were assessed clinically and functionally by using Oxford Knee Score (OKS) [14], Knee Society Score (KSS) [15] preoperatively and at further follow-ups postoperatively. Also patient satisfaction regarding pain and perception of knee normality were assessed by subjective evaluation which is categorized as very satisfied, satisfied, uncertain and dissatisfied. Range of motion of the operated knee is recorded pre and postoperatively. Prosthesis were assessed using the Oxford radiological evaluation criterias.
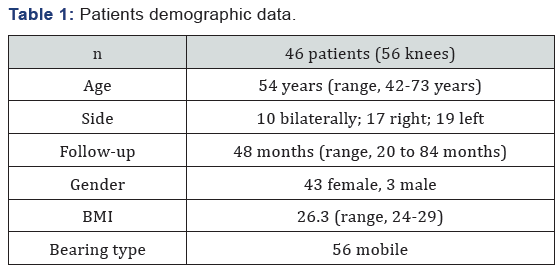
BMI: Body Mass Index.
Patient Selection
After medical history and physical examination, serial radiographs including anteroposterior (AP) standing up-right and lateral (L) knee graphies at 30° flexion and Rosenberg views (PA 10° caudal knee graphy in knee slightly flexion) are routinely taken. The inclusion criterias for this study were:
i. Anteromedial knee pain on one finger test with medial compartment osteoarthritis
ii. Intact lateral compartment (no loss of cartilage on lateral condyles weight-bearing surfaces and no meniscal tear) and intact anterior cruciat ligament some of which were revealed by magnetic resonance imaging (MRI) scans
iii. Varus deformity lower than 15° or correctable varus deformity at 20° flexion
iv. Flexion contracture lower than 15°
Furthermore patellofemoral arthritis classified as lower than outerbridge grade 4, the patients’s age, weight and activity level were not contraindications to the operation. However patients with a history of surgery for osteoarthritis and previous fractures around the affected knee were excluded from the study.
Preoperative Assessment
We used the templates of implants on anteroposterior and lateral x-rays to predict the implant size preoperatively. Also the weight, height, and BMI of each patient had been recorded preoperatively. Preoperative patient information booklet was given to each patient including informations about the operation and medical care they will require during perioperative period.
Surgical Procedure
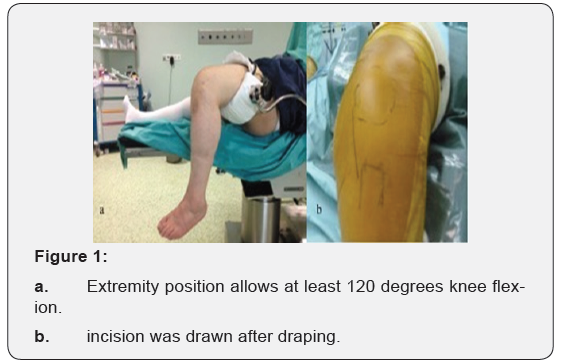
Patients were placed in the supine position after combined (spinal+epidural) anesthesia in the operating room. The thigh was held in special leg holder to allow minimum 120 degrees knee flexion during the procedure (Figure 1). After the medial parapatellar incision, arthrotomy was performed. Appropriate bone cuts were done and implants were placed (Figure 2). UKA was performed both knees in 10 patiens simultaneously, while implanted unilaterally in 36 patients. Mobile-bearing implants in 56 knees (Biomet, Warsaw, IN, USA) were used. Jones bandage, Ranawat coctail and tranexamic acid were applied postoperatively.

All patients had the same physiotherapy with starting Continuous Passive Motion (CPM) at the same day after operation and mobilized with crutches the day after surgery. Follow-up clinical and radiological interventions were planned at 6 weeks, 3 months, 6 months and 1 year postoperatively at our outpatient clinic. Further follow-ups were then set at yearly intervals. All data was analyzed statistically using SPSS ver.22.0. For statistical analysis the t test of comparison of means for paired data was used, and p<0.05 was considered significant.
Results
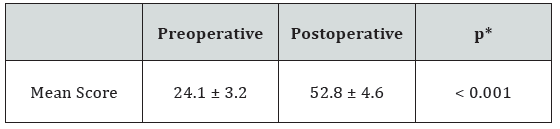
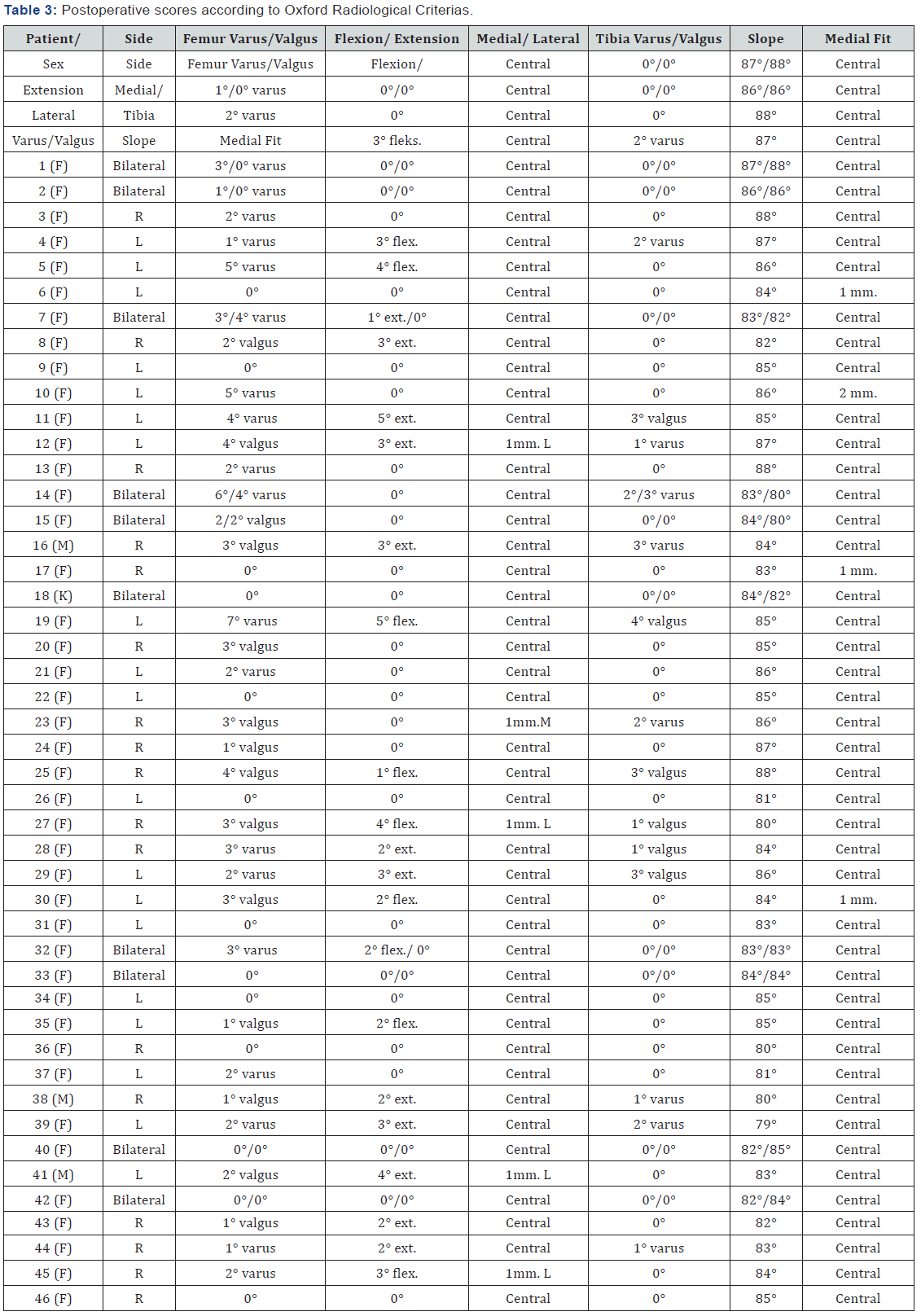
Preoperative mean range of motion was increased from 116° (range, 100-126°) flexion to 123° flexion (range 115- 135°), whereas there was no limitation in knee extension preor postoperatively. The mean KSS was increased from 54.6 ± 7.5 to 90.1 ± 6, the mean OKS increased from 24.1 ± 3.2 to 52.8 ± 4.6, and the mean VAS was decreased from 7.96 ± 1.02 to 2.29 ± 0.89 (p<0.001). Regarding the radiological assessment, no femoral or tibial component showed radiological loosening. Postoperatve short to mid-term radiographic measurements showed that the position of the femoral components was within acceptable ranges with a mean of 1.8° varus (range 7° varus to 3° valgus), whereas the position of the tibial component was within acceptable ranges with a mean of 0.5° varus (range 2° varus to 4°valgus) and a mean slope of 84.5° (range 79°-88°). All of the tibial components, except an overflow of 1mm. in three and 2mm. in one, showed full congruency with medial plane.
Preoperative and postoperative scores were summarized in Table 2, and radiological scores were summarized in Table 3. During follow-up, 1 male patient had insert dislocation at 6 weeks postoperatively. İnitially, insert was replaced with the manuplation of closed reduction under sedative anesthesia. He returned to his pre-dislocation level of activity, however he had insert dislocation again after 4 weeks of reduction. 4-mm. insert was replaced with a thicker and more anatomical 6-mm one. Furthermore, 2 female patients had persistent anterior and medial knee pain postoperatively without any sign of insert dislocation or implant-related problems, however complete pain relief was achieved with continous physiotherapy at 1 year postoperatively. None of the paients had deep vein trombosis, infection, implant loosening, osteolysis, implant-related fracture or opposite compartment osteoarthritis. The overall satisfaction in this study was noted as very satisfied in 36 patients’ 42 knees (75 %), satisfied in 6 patients’ 9 knees (16 %), uncertain in 3 patients’ 4 knees (7 %), and dissatisfied in one patients’ knee (2 %). The overall survival rate of implants were %100 at 5 years postoperatively.
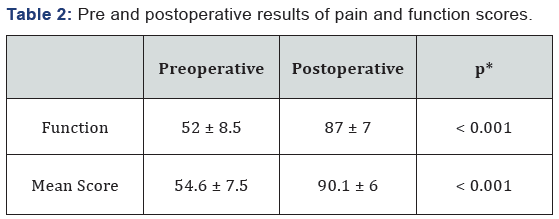
Pre and postoperative Knee Society Scores.
*paired samples t test
*paired samples t test
Pre and postoperative Oxford Knee Scores.

*paired samples t test
VAS (Visual Analog Scala).
Discussion
The survival rate after UKA depends on many factors. In the current study, the survival rate of prosthesis was 100 % at 4-year follow-up in patients with the mean age of 54 years, results of which is found better than the aforomentioned studies. In similar studies, Cepni et al. [1] reported 95.6 % survival rate of UKA implants at 5.5 years with the mean age of 61 ± 7.3 years, while Tadros et al. [16] reported 93 % survival rate at a mean follow-up of 4.7 years with the mean age of older than 57.9 years, Clement et al. [17] reported 87.7 % survival rate at 5 years with a mean age of 69.5 years, and Pandit et al. [18] 97.3% at seven years with a mean age of 66.4 years [18]. In these studies, younger age (<60 years) was accepted a predictor of failure, at the end they explain the reason as younger and males expect greater improvement in knee function than the prosthesis can offer. However, our study group has disproved those scientific publications.
Many complications dedicated to UKA has been reported such as progression of lateral compartment osteoarthritis, periprosthetic fracture (mostly medial tibial plateau), and polyethylene insert dislocation of mobile implants [8,11-13,19- 21]. All these problems occurred due to non-anatomical implant designs, inappropriate patient selection, overcorrection and malposition of the implants. Depending on the increase in the incidence of complications, more anatomical and minimally invasive implant designs were produced by manufacturers which contributed less soft tissue injury, more bone stock preservation, early postoperative rehabilitation due to less blood loss and pain, and shorter hospital stay resulting with rapid recovery [2,10,22,23]. Bearing dislocations in mobile design implants are considered higher and the most important cause of this complication would be inappropriate gap balancing between flexion and extension. Lewold et al. reported that the reason of the bearing dislocation is mostly attributed to implant malposition and soft tissue imbalancing [24]. Other possible reasons are the posterior impingement by remaining meniscus, osteophytes and excessive release of medial collateral ligament, respectively [25]. In our study, all implants were mobile, however we had only one insert dislocation as a major complication. Probably the reason of our complication is considered the use of early-designed non-anatomical mobile bearing implants. İn terms of higher incidence of dislocation, Oxford group developed a new anatomical bearing which had an extended length of medial wall to protect further dislocations. Moreover the new implant increased the amount of rotation that the bearing had to undergo, and the anteromedial corner of the bearing has been reduced to decrease anterior overhang in extension.
In the literature, there are some reports about this subject which was managed with revision surgeries. Clement et al. reported 3 revisions due to unexplained persistant symptomatic knee pain in the second postoperative year. They emphazised that unnecessarily revisions before two-year follow-up may result higher early revision rates [17]. In a similar study, Lewold et al. reported 6 revisions of 1000 UKA due to unexplained pain three of which were reported as unhappy after the second operations. In our study, two patients had unexplained anterior knee pain after the operation which was managed by further physiotherapy at postoperative first year.
In our study we had also 100% survivorship with the careful preoperative planning and patient selection at 4 years follow-up. Supporting our results, Andrew et al. reported %91 survival for the Oxford mobile implants by following the correct indications in appropriate selected patients at 20 years follow-up [12], and Bell et al. reported 100% survivorship at a mean of 24 months follow-up with the accurate preoperative plan and patient selection [20]. Comparison of the survivorship and functional results of mobile and fixed bearing implants is another subject that should be discussed. Arthroplasty registries suggested no conclusive advantage of one bearing design over another, however this is an individual subject that should be discussed. Inoue et al. [26] reported that some laxity should be provided in medial collateral ligament (MCL) in fixed bearing implants, whereas there must be appropriate tension in MCL in mobile bearing implants to prevent dislocation. We considered this feature in our study which resulted without any revision.
In a study, Aldinger et al. [27] reported higher wear and failure rates of fixed bearings than mobile bearings. In a review by Ko et al. [28] while the progression of arthritis and dislocation were the main reasons of complications for the mobile bearing implants, wear was the only main complication requiring reoperation with fixed bearing implants. There is a limited follow-up of comparative studies between fixed and mobile bearing implants in terms of survivorship, however they found no difference [29,30]. On the other hand, In a long-term study, comparing the results of fixed and mobile bearing designs of UKA, Parratte et al. found no difference in survivorship and function between two bearing designs [31]. The meniscal mobile bearing moves to posterior with the knee fully flexed which permits and restores isometric function of the ligaments. Regarding this subject, we therefore used only mobile-bearing implants.
To our knowledge, there are no reports on the outcomes of the radiological positioning and congruency of the UKA. Optimal positioning between components in terms of tibial slope, medial fit, varus/valgus, and flexion/extension angle resulting neutral alignment of the knee was achieved in all cases. Few limitations should be noted. First, the study was retrospective with the risk of attendence of selection bias. Second, 3 of 46 patients, included in this study, were male, so we could not compared the gender demografic, clinical and radiological effects on survivorship. Lustig et al. [32] reported that the gender effect on outcome of UKA has no difference in terms of range of motion, radiologic progression of arthritis and alignment. There is no comprehensive study about gender effect on results of UKA, there may be further investigations requiring this subject. Third this study has a short- to midterm follow-up ,thus we can comment on whether our intervention provides outcomes superior to those provided by nonoperative treatment, TKA or HTO or if the surgical procedure provides an advantage over these procedures. More prospective randomised trial would be the best method to determine this.
However we can comment on performing the surgeries experienced team could provide significant contribution to achieve the success. Because the level of experience of the surgeon is considered a key factor to the overall survival of the implants and satisfactory outcomes in many scientific reports. Also It is reported that low volume UKA performing centers have caused higher revision rates in many reports [17,20,33,34]. Bini et al. [33] evaluated the surgeon volume effects on revision rates and declared the yearly volume of less than twelve UKA had been significant risk for failure. In a high volume study reported by Baker et al., 23400 UKA were evaluated and concluded that high volume centers and surgeons specialized in UKA showed superior outcomes, and the minimum number of UKA’s per surgeon should be more than thirteen per year [34]. Nevertheless, we are encouraged by our short to midterm results using UKA for the treatment of medial compartment osteoarthritis of the knee, with complete satisfaction with the outcome of their surgery at last interventions.
Conclusion
Our study results suggest that UKA in patients with isolated medial compartmental osteoarthritis can yield promising results if it remains faithful to the proper patient selection and surgical technique. However, we recommend large-scale and long-term, prospective, clinical studies to confirm the efficacy of the technique.
Competing Interest
The authors declare that they have no competing interests.
Source of Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgement
None.
References
- Cepni SK, Arslan A, Polat H, Yalçin A, Parmaksizoğlu AS, et al. (2014) Mid-term results of Oxford Phase 3 unicompartmental knee arthroplasty in obese patients. Acta Orthop Traumatol Turc 48(2): 122-126.
- Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470(1): 84-90.
- Arirachakaran A, Choowit P, Putananon C, Muangsiri S, Kongtharvonskul J (2015) Is unicompartmental knee arthroplasty (UKA) superior to total knee arthroplasty (TKA)? A systematic review and meta-analysis of randomized controlled trial. Eur J Orthop Surg Traumatol 25(5): 799-806.
- Alnachoukati OK, Barrington JW, Berend KR, Kolczun MC, Emerson RH, et al. (2017) Eight Hundred Twenty-Five Medial Mobile-Bearing Unicompartmental Knee Arthroplaties: The First 10-Year US Multi- Center Survival Analysis. J Arthroplasty 33(3): 677-683.
- SooHoo NF, Sharifi H, Kominski G, Lieberman JR (2006) Costeffectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. J Bone Joint Surg Am 88(9): 1975-1982.
- McKeever DC (1960) Tibial plateau prosthesis. Clin Orthop 18: 86-95.
- Marmor L (1979) Marmor modular knee in unicompartmental disease: minimum four-year follow-up. J Bone Joint Surg Am 61(3): 347-353.
- Marmor L (1988) Unicompartmental arthroplasty of the knee with a minimum ten-year follow-up period. Clin Orthop 228: 171-177.
- Murray DW, Goodfellow JW, O’Connor JJ (1998) The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br 80(6): 983-989.
- Panzram B, Bertlich I, Reiner T, Walker T, Hagmann S, et al. (2017) Cementless Oxford medial unicompartimental knee replacement: an independent series with a 5-year-follow-up. Arch Orthop Trauma Surg 137(7): 1011-1017.
- Khanna G, Levy BA (2007) Oxford unicompartmental knee replacement: literature review. Orthopedics 30(5 suppl): 11-14.
- Price AJ, Svard U (2011) A Second decade lifetable survival analysis of the Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res 469(1): 174-179.
- Svard UC, Price AJ (2001) Oxford medial unicompartmental knee arthroplasty. A survival analysis of an independent series. J Bone Joint Surg Br 83(2): 191-194.
- Dawson J, Fitzpatrick R, Carr A, Murray D (1996) Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br 78(2): 185-190.
- Insall JN, Dorr LD, Scott RD, Scott WN (1989) Rationale of the Knee Society Clinical Rating System. Clin Orthop Relat Res 248: 13–14.
- Tadros BJ, Dabis J, Twyman R (2017) Short-term outcome of unicompartmental knee arthroplasty in the octogenarian population. Knee Surg Sports Traumatol Arthrosc 26(5): 1571-1576.
- Clement ND, Duckworth AD, MacKenzie SP, Nie YX, Tiemessen CH (2012) Medium-term results of Oxford phase-3 medial unicompartmental knee arthroplasty. J Orthop Surg (Hong Kong) 20(2): 157-161.
- Pandit H, Jenkins C, Barker K, Dodd CA, Murray DW (2006) The Oxford medial unicompartmental knee replacement using a minimallyinvasive approach. J Bone Joint Surg Br 88(1): 54-60.
- Robertsson O, Knutson K, Lewold S, Lidgren L (2001) The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone Joint Surg Br 83(1): 45-49.
- Bell SW, Stoddard J, Bennett C, London NJ (2014) Accuracy and early outcomes in medial unicompartmental knee arthroplasty performed using patient specific instrumentation. Knee 21 Suppl 1: S33-S36.
- Li CS, Karlsson J, Winemaker M, Sancheti P, Bhandari M (2014) Orthopedic surgeons feel that there is a treatment gap in management of early OA: international survey. Knee Surg Sports Traumatol Arthrosc. 22(2): 363-378.
- Peersman G, Jak W, Vandenlangenbergh T, Jans C, Cartier P, et al. (2014) Cost-effectiveness of unicondylar versus total knee arthroplasty: a Markov model analysis. Knee 21 Suppl 1: S37-S42.
- Manzotti A, Cerveri P, Pullen C, Confalonieri N (2014) A flat allpolyethylene tibial component in medial unicompartmental knee arthroplasty: a long-term study. Knee. 21 Suppl 1: S20-S25.
- Lewold S, Goodman S, Knutson K, Robertsson O, Lidgren L (1995) Oxford meniscal bearing knee versus the Marmor knee in unicompartmental arthroplasty for arthrosis. A Swedish multicenter survival study. J Arthroplasty 10(6): 722–731.
- Emerson RH Jr (2005) Unicompartmental mobile-bearing knee arthroplasty. Instr Course Lect 54: 221-224.
- Inoue A, Arai Y, Nakagawa S, Inoue H, Yamazoe S, et al. (2016) Comparison of Alignment Correction Angles Between Fixed-Bearing and Mobile-Bearing UKA. J Arthroplasty 31(1): 142-145.
- Aldinger PR, Clarius M, Murray DW, Goodfellow JW, Breusch SJ (2004) Medial unicompartmental knee replacement using the “Oxford Uni” meniscal bearing knee. Orthopade 33(11): 1277-1283.
- Ko YB, Gujarathi MR, Oh KJ (2015) Outcome of Unicompartmental Knee Arthroplasty: A Systematic Review of Comparative Studies between Fixed and Mobile Bearings Focusing on Complications. Knee Surg Relat Res 27(3): 141-148.
- Whittaker JP, Naudie DD, McAuley JP, McCalden RW, Mac- Donald SJ, et al. (2010) Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin Orthop Relat Res 468(1): 73–81.
- Bonutti PM, Dethmers DA (2008) Contemporary unicompartmental knee arthroplasty: fixed vs mobile bearing. J Arthroplasty 23: 24–27.
- Parratte S, Pauly V, Aubaniac JM, Argenson JN (2012) No long-term difference between fixed and mobile medial unicompartmental arthroplasty. Clin Orthop Relat Res 470(1): 61-68.
- Lustig S, Barba N, Magnussen RA, Servien E, Demey G, et al. (2012) The effect of gender on outcome of unicompartmental knee arthroplasty. Knee 19(3): 176-179.
- Bini S, Khatod M, Cafri G, Chen Y, Paxton EW (2013) Surgeon, implant, and patient variables may explain variability in early revision rates reported for unicompartmental arthroplasty. J Bone Joint Surg Am 95(24): 2195-2202.
- Baker P, Jameson S, Critchley R, Reed M, Gregg P, et al. (2013) Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am 95(8): 702–709.






























