Are Psychosocial Factors Worsening Chronic Low Back Pain? Study to Assess Radiological and Psychological Parameters Affecting Back Pain and to Assess Remedial Effects of Duloxetine
Varun Singh and Rakesh Bhargava*
1Assistant Professor, Department of Orthopaedics, Rajasthan University of Health Sciences, India
2Senior Professor, Department of Orthopaedics, India
Submission: December 28, 2018;Published: February 11, 2019
*Corresponding author: Rakesh Bhargava, MS Orthopaedics, Assistant Professor, Department of Orthopaedics, Rajasthan University of Health Sciences Jaipur, India
How to cite this article: Varun Singh, Rakesh Bhargava. Are Psychosocial Factors Worsening Chronic Low Back Pain? Study to Assess Radiological and Psychological Parameters Affecting Back Pain and to Assess Remedial Effects of Duloxetine. Ortho & Rheum Open Access J 2019; 13(4): 555866.DOI: 10.19080/OROAJ.2019.13.555866
Abstract
Background: Low back pain is one of the most common musculoskeletal disorders. Present study focuses on identifying psychological factors along with assessing the relationship between change in lumbo-sacral spine parameters and low back pain, further we have assessed the outcome of different treatment regimens given to patients with different severity.
Material and Methods: Study is prospective and interventional in nature; 100 patients were included in the study. All patients were assessed clinically and given treatment according to the severity group. Six radiological parameters and four subjective questionnaires were chosen as to measure clinical and psycho-social status on every follow-up.
Result: Low back pain causes reduction in lumbar lordosis (Lumbo-pelvic lordosis and lumbar lordotic angle) and improvement in back pain caused normalization of lordosis values. All the subjective outcome measurement tools indicated significant change and improvement specially in patients who received Duloxetine in conjunction to the normal treatment.
Conclusion: Psycho-social factors have major contribution in causation of non-specific low back pain and vice-versa. Patient develops a vicious cycle and use of Duloxetine in non-specific chronic low back pain breaks this vicious cycle, provides early and sustained pain relief as well as improves patient’s illness perception and quality of life.
Keywords: Back Pain; Severity; Radiological parameters; Psychosocial; Lordosis; Duloxetine
Introduction
Low back pain is one of the most common complaints presented to the Orthopedic surgeons. It has been estimated that 60 % to 80% of all adults experience chronic low back pain [1,2]. It is in the region from below the twelfth rib to the inferior gluteal fold [3].
Low Back Pain Places Large Demands on Health, Social and Economic Systems
Although the majority (80%-90%) of low back pain incidents resolve in six-week time, while 5%-10% experience chronic low back pain. Low back pain is a multi-factorial problem. Minor risk factors include genetic factors, age and smoking. Major causes include same work postures for long time, lifting heavy weight, obesity and psychosocial factors [4]. Non-Specific back pain may originate from the vertebrae or soft tissues surrounding the spinal column. Usually no pathology can be detected5,6,7. Low back pain can be acute (<4 weeks), sub-acute (4-12 weeks) or chronic (>12 weeks) in duration. Chronic back pain is more difficult to treat, which may have strong psychological connection.
Hypothesis for this study was whether radiological parameters change during treatment and whether psychological factors such as depression and anxiety play any major role in severity and chronicity of low back pain. The purpose of this study was to examine relationship between low back pain and radiological lumbo-sacral spinal parameters and to find out psychosocial factors associated with low back pain and to measure outcome of treatment.
Materials and Methods
Study conducted is prospective and interventional in nature. The Study was initiated on total 138 patients, (36 patients had incomplete follow-up records) , 100 patients were finally included in the study for statistical ease
Inclusion Criteria
a. All patients above 20 years of age.
b. Nonspecific chronic low back pain except for occasional episodes after work or exertion.
c. Duration of at least three months.
Exclusion Criteria
a. Patients with previous back surgery,
b. Serious mental health problems for whom participation in study would not be feasible.
c. Spondylolisthesis.
d. Radiculopathy or lumbar canal stenosis.
e. Definite clinical spine deformities from physical examination and X-ray.
In outpatient department the severity of pain was assessed using the VAS scale. Patients were segregated into the three groups according to their severity of pain as per the VAS (Visual Analogue Scale) scoring system8. 0-3: Mild Pain (Group A), [4-6]: Moderate Pain (Group B), [7-10]: Severe Pain (Group C). Third group C was again subdivided into two (C1 and C2), based on treatment given, C1 patients were given duloxetine in addition. Range of motion (including Flexion, Extension, Lateral Bending Right and Left) was evaluated and measured in degrees using Goniometer.
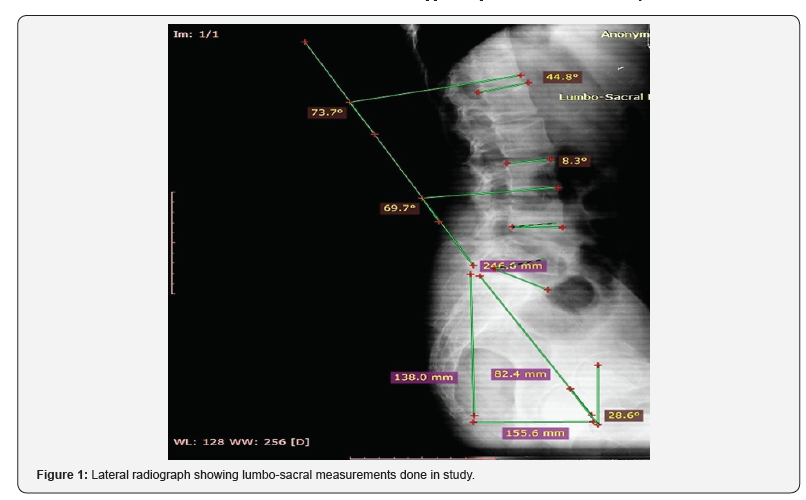
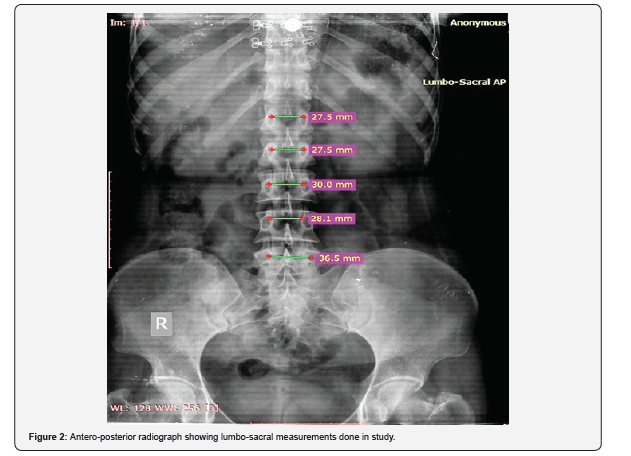
Aproforma was explained to the patients in their own language and their responses were noted down at same time. Radiological Assessment was done withantero-posterior and lateral view ski grams of the lumbo-sacral spine. Pelvic radius measurement was done with the help of PR-T12 line and Cobb’s Technique was used for the lumbar lordotic angle measurement. Computer software RadiAntDiacom Viewer was used for all measurements. The hip axis is midway between the two hip centers and a line was drawn to the postero-superior corner of sacral end plate for the pelvic radius. Length was measured in millimeters.
Figures 1 & 2 shows Lateral and AP Radiographs showing lumbo-sacral measurements done in study. Parameters measured on standing AP and Lateral ski grams are Interpedicular Distance: Transverse distance between left and right pedicles is measured of each level from L1 to L5, Pelvic Radius: Distance from hip axis to posterior superior corner of S1 [10], Pelvic Angle: Angular measurement between the pelvic radius line and a vertical line draw through the hip axis, Sacral Translation: Horizontal distance between the vertical line through hip axis, Total Lumbopelvic Lordosis: Angular measurements between from the PR line and a tangent line along the inf end plate of T12 body, Lumbar Lordotic Angle: Angular measurement between upper endplate of L1 and that of S1 by cobb’s method.
To observe outcome of management three different treatment regimen were instituted to the three different severity groups of patients:
Group A: Patients with mild back pain were classified at low risk of a poor outcome, patients were prescribed Physiotherapy (McKenzie’s Exercise approach [9]) and Analgesics [(Non- Steroidal anti-inflammatory drug): Diclofenac Sodium 75mg twice daily].
Group B: Patients with moderately severe pain and disability and were at moderate or high risk of poor outcome, they were prescribed Physiotherapy, Analgesics as above and Muscle relaxant (Thiocholchicoside 4 mg twice daily).
Group C: Severe levels of back pain related symptoms with associated functional limitations, Group C1 patients were prescribed Physiotherapy and Analgesic along with Muscle Relaxants as in group B and Duloxetine [Tablet Duloxetine (Selective Serotonin and Nor-epinephrine reuptake inhibitor): 60 mg once daily [8]. Group C2 patients with severe pain were also prescribed similar treatment regimen as group C1 except Duloxetine.
Antacid: [Pantoprazole (Proton Pump inhibitor) 20 mg once daily] for prevention of NSAID induced ulcers were given to all the patients.
To assess associated psychological factors four questionnaire were used as subjective outcome measures for every followup visit: Visual Analogue Scale [11], Disability Questionnaire (Modification of Roland-Morris Low Back Pain and Disability Questionnaire) [12], B-IPQ, Brief illness perception questionnaire [13], Anxiety and Depression Scale (Modification of Hospital Anxiety and Depression Questionnaire) [14].
Follow Up Protocol
All Patients underwent clinical and radiological examination along with subjective outcome questionnaires at first visit and on every follow-up. Radiological angles were measured on regular follow up and difference in values with treatment were documented. Initial treatment was given for 2 weeks. Those who had complete pain relief were stopped with the treatment but continued with the follow-up. Those who got partial relief continued with the same regimen for 2 weeks more and were reviewed again. There after patients were advised to report back on recurrence of bouts of low back pain. Follow-up of the patients was done on three, six, nine and at twelve months. Degree of improvement in lumbo-sacral spine parameters were correlated with the degree of improvement in the clinical symptoms.
Statistical Method
Mean and Standard Deviation of each parameter were analyzed. The one-way analysis of variances (ANOVAs) was used to compare the mean of radiographic parameters. The statistically significant difference was considered for a P value less than 0.05. Ethical Committee approval was taken before start of study.
Results
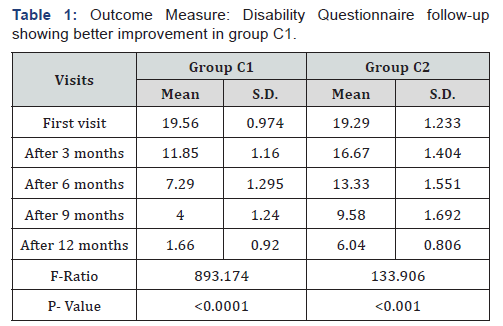
Among total number of patients in the present study 70% were males and 30 % were females. Vas Scores (group A, B and C), range of movements including flexion, extension, lateral flexion (right), lateral flexion (left) improved significantly in group C, specially C1 where the Duloxetine was given to the patients along with the routine treatment regimen. Regarding Groups A and B, mean VAS scores changed from 3.16 ± 3.57 to 1.48 ± 5.96 in group A, from 5.29 ± 0.75 to 0 in group B. Regarding male and female patient’s value of lordosis at completion of treatment. Mean male lumbo-pelvic angle is 79.88 and for female is 82.28 in degrees, comparison showed significant P value of 0.013 (<0.05).
Mean lumbar-lordotic angle at 12 months, for male it is 46.04 while for female it is 45.6 in degrees (Non-significant P value = 0.38). No statistically significant difference was found among three different age groups in relation to lumbo-pelvic lordosis angle and lumber lordotic angle with p value 0.159 and 0.238 respectively. Total Lumbo-pelvic Lordosis in all four groups on each follow-up visit. P-Values are Significant indicating improvement of lordosis in all four groups with constant improvement in lumbar lordotic angle in all four groups, measured on first and then subsequent follow-up visits. Subjective Assessment of Psychosocial Status which was deteriorated as the pain and discomfort increased, showed significant improvement in patients who were given duloxetine.
In present study mean Brief Illness Perception Questionnaire scores changed impressively in group C1, and from 18.9±7.11 to 0.80±1.19 in group A and from 34.25±3.16 to 0.75±0.84 in group B. Anxiety and Depression Scale, among groups C1 and C2 on every follow-up visit. Group C1 showing Highly Significant P-Value <0.0001, showing good improvement. Regarding Groups A and B, it changed from 4.32 ± 3.5 to 0.24 ± 0.66 in Group A and from 8.45 ± 1.17 to 0 in Group B.
Statistical Method
Mean and Standard Deviation of each parameter were analyzed. The one-way analysis of variances (ANOVAs) was used to compare the mean of radiographic parameters. The statistically significant difference was considered for a P value less than 0.05.
Discussion
Low back pain is a multi-factorial problem. Apart from describing the lumbo-sacral spine parameters involved, the present study has identified key relations between determinants and episodes of low back pain. Findings of the study indicate psychological issues as major risk factor for chronic non-specific low back pain. Study observes that females have inherently higher values of lumbo-pelvic lordosis angle while lumbar lordotic angle was found to be almost similar in both gender patients, with non-significant P value of 0.38. Stagnaraet [15] have shown that females had a greater degree of lumbar lordosis when compared to the male subjects. Present study observes that low back pain reduces the range of movement, consistent with finding of Deniz Evcik & AylinYücel [16,17].
Low back pain reduces lumbar lordotic angle as well and these findings are consistent with the previously done studies. Tsuji [10] found that lumbar lordosis was approximately 4 degrees less in the low back pain group and there was no relationship to age or sex in either group. VAS was significantly inversely correlated with lumbar lordosis (P = 0.025, at rest). VAS score improved with treatment. Present study shows that Group C1 showed better improvement as compared with C2. Regarding other radiological parameters no significant changes were seen in Inter-pedicular Distance, Pelvic Radius, Pelvic Angle and Sacral translation, hence no relationship between these parameters and low back pain could be established (Table 1).
Christoph Herrmann [13] showed that The Hospital Anxiety and Depression Scale (HADS) is a useful psychological screening tool, it is sensitive to measure response of psychotherapeutic intervention. It has been shown that in adolescent population psychosocial factors play stronger predictor of low back pain than mechanical factors17. In adult populations, psychosocial factors influence the chronicity and are more strongly related to the outcome than any other clinical or mechanical factors [18,19]. In present study, patients who received Duloxetine in addition to standard treatment regimen, showed better results in terms of early and sustained pain relief.
A study done by Howard G [20] concluded that patients on Duloxetine had a significantly greater reduction in the BPI 24- hour average pain from baseline to endpoint (P = 0.004 at week 13). These results are consistent with present study, additionally, the Duloxetine group of patients had better Roland-Morris Disability Questionnaire scores. Skljarevski [8] also concluded in their study that Duloxetine significantly reduced pain and improved functioning in patients with chronic low back pain. They showed that 60mg once daily dose is efficacious in chronic low back pain. Howard S Smith [21] showed modest efficacy but found to be associated with complication such as serotonin syndrome with high doses. While Pinky Dharmshaktu [22] found that, analgesic effects of selective serotonin reuptake inhibitors (fluoxetine, paroxetine, citalopram) are less, yet they have better tolerability as compared with tricyclic antidepressants.
All the subjective outcome measures to measure the efficacy of treatment showed significant change and improvement in symptoms in terms of function, range of movement, illness perception, reduction in disability and reduction in anxiety and depression scores, especially in patients who received Duloxetine in conjunction to the normal treatment. Psycho-social factors have major contribution in causation of non-specific low back pain and vice-versa. Patient develops a vicious cycle and the disease worsens. Use of Duloxetine in non-specific low back pain breaks this vicious cycle, provides early and sustained pain relief, as well as improves patient’s illness perception and quality of life. These findings have raised important questions for future research about the relation of early psychological distress to the development of subsequent low back pain and suggest that management of the onset of occupational low back pain may be improved by management of psychological issues thus medicines like duloxetine can serve major role in management of such cases.
Conclusion
Present study shows importance and prevalence of psychological issues as a major factor for low back pain in adults. The study opens a new window for Duloxetine’s regular use in non-specific chronic low back pain patients. This study provides baseline values of various lumbo-sacral parameters in rural population of Jaipur (Rajasthan, India). Till date there has been no other study in literature which has provided or interpreted similar data in the Indian population. Present study strengthens the relationship between lumbar lordosis and low back pain. Study shows females have higher lordosis values as compared to males. These findings may prove to be important clinical predictor and a prognostic factor, however further studies are needed to throw more light on this correlation. However, sample groups in this study were small as compared to the large number of patients with non-specific low back pain present in general population. More research work in this direction which includes larger sample size would be helpful to improve practical interventions to reduce this burden of low back pain.
Financial Statement
We have taken no external source of funding, no source of support, conflict of interests NIL. We certify that we have obtained all appropriate patient consent forms. In the form the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity.
References
- Anderson GBJ (1998) Epidemiology of low back pain. Acta Orthop Scand 281: 28-31.
- COST B13 (2004) Working Group on Guidelines for the Management of Acute Low Back Pain in Primary Cale. p. 8.
- De Wet MM (2003) Low Back Pain in the Corporate Workplace-a South African Review. Masters dissertation. University of Johannesburg, Johannesburg, South Africa.
- Manchikanti L (2000) Epidemiology of low back pain. Journal of Pain Physician 3(2): 167-192.
- Carey TS, Evans AT, Hadler NM (1996) Acute severe low back pain: a population-based study of prevalence and care-seeking. Spine 21(3): 339-344.
- Frymoyer JW, Cats-Baril WL (1991) An over view of the incidences and costs of low back pain. Orthopaedic Clinics of North America 22(2): 263-271.
- Federico Balagué, Anne F Mannion, Ferran Pellisé, Christine Cedraschi (2012) Non-specific low back pain. The Lancet, 4 379(9814): 482 - 491.
- Skljarevski V, Desaiah D, Liu-Seifert H (2010) Efficacy and safety of duloxetine in patients with chronic low back pain. Spine, 35(13): E578-E585.
- Williams PC (1955) Examination and conservative treatment for disc lesions of the lower spine. Clin orthop 5: 28-40.
- Tsuji T, Matsuyama Y (2001) Epidemiology of low back pain in the elderly: correlation with lumbar lordosis. J Orthop Sci 6(4): 307-311.
- Chapman (2011) Evaluating Common Outcomes for Measuring Treatment Success for Chronic Low Back Pain. Spine, 36: S54-S68.
- Elizabeth Broadbent, Keith J Petrie, Jodie Main, John Weinman (2006) The Brief Illness Perception Questionnaire. Journal of Psychosomatic Research, 60(6): 631-637.
- Christoph Herrmann (1997) International experiences with the Hospital Anxiety and Depression Scale-A review of validation data and clinical results. Journal of Psychosomatic Research, 42(1): 17-41.
- William H, Kirkaldy-Willis, Thomas N Bernard Jr (1999) Managing Low Back Pain, 4e Hardcover.
- Stagnara P, De Mauroy JC, Dran G, Gonan GP, Costanzo G, et al. (1982) Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine 7: 335-336.
- Deniz Evcik, Aylin Yücel (2003) Lumbar lordosis in acute and chronic low back pain patients. Rheumatol Int 23(4):163-165.
- Walker BF, French SD, Grant W, Green S (2010) Combined chiropractic interventions for low-back pain. Cochrane Database Syst Rev 4: CD005427.
- Smeets RJ, Severens JL, Beelen S, Vlaeyen JW, Knottnerus JA (2009) More is not always better: cost-effectiveness analysis of combined, single behavioral and single physical rehabilitation programs for chronic low back pain. Eur J Pain 13(1): 71-81.
- Nawal A Alarfaj, Reda A Ammar, Maha F El-Tohamy (2012) Disposable screen-printed sensors for determination of duloxetine hydrochloride. Chemistry Central Journal 6: 6.
- Howard G Birnbaum, Evan Kantor, Matt Schiller, Ralph W Swindle (2012) Duloxetine Use in Chronic Low Back Pain. Pharmaco Economics, 30(7): 595-609.
- Howard S Smith, Eric J Smith, Benjamin R Smith (2012) Duloxetine in the management of chronic musculoskeletal pain. therapeutics and clinical risk management 8: 267-277.
- Pinky Dharmshaktu, Vandana Tayal, Bhupinder Singh Kalra (2012) Efficacy of Antidepressants as Analgesics: A Review. The Journal of Clinical Pharmacology 52(1): 6-17.






























