Unstable Metacarpal Fractures: A comparative study between Mini-plates and percutaneus K-wire fixation at Emergency Hospital, Mansoura University, Egypt
Ilahiane M*, Abdulrazak S, Hassani I, Marzouki A and Boutayeb F
Department of orthopaedic surgery, Hassan II hospital, Fès, Morocco
Submission: October 29, 2018;Published: November 26, 2018
*Corresponding author: Ilahiane Mohamed, Department of orthopaedic surgery, Hassan II hospital, Fès, Morocco
How to cite this article: Ilahiane M, Abdulrazak S, Hassani I, Marzouki A, Boutayeb F. Acute Patella Tendon Rupture: A Case Report. Ortho & Rheum Open Access J 2018; 13(2): 555859. DOI:10.19080/OROAJ.2018.13.555859.
Abstract
Introduction: Management of metacarpal shaft fracture is dictated by the stability and personality of the fracture. It may be conservative or surgical. Surgical management of Metacarpal fractures has different techniques and different instruments.
Methods: The study included 40 patients presented at Emergency Hospital, Faculty of Medicine, Mansoura University, with 48 fractured metacarpals in 30 hands. 20 patients were fixed by open reduction and internal fixation using mini-plates, the other 20 patients were fixed by percutanous K wires.
Results: In this study, it was found that after 6 weeks of follow up, group A showed 93.3 % satisfactory results, while group B showed 86.7 % satisfactory results, while after 3 months of follow up both groups showed satisfactory and good results in 93.3 % of cases.
Conclusion: Mini-plates fixation in oblique and spiral fractures provide stable and rigid internal fixation that allows early active range of motion and early excellent results. Percutaneous K-wire fixation has the advantages of preserving the soft tissue.
Introduction
Metacarpal fractures comprise between 18–44 % of all hand fractures [1-3]. Most metacarpal fractures occur in the active and working population, particularly adolescents and young adults. Trauma to the hand is exceedingly common, frequently resulting in metacarpal, fractures and dislocations [3,4]. Appropriate treatment includes a thorough assessment, physical examination, and directed imaging. Such an approach should lead to a rational treatment plan that focuses on the rehabilitation of all damaged components, including osseous, articular, and soft tissue structures [5,6]. Management of metacarpal shaft fracture is dictated by the stability and personality of the fracture. Undisplaced fracture with any fracture configuration can be managed by conservative method with a slab or a splint immobilising the wrist in Extension and MP joint in flexion greater than 70° (Clam digger slab/cast), allowing early IP mobilisation. [7-11].
No absolute contraindications exist for treatment of metacarpal injuries. Almost all injuries are amenable to either immobilization, closed or open reduction, with or without fixation [12-14]. Disability from hand injury may result in loss of sensation, loss of strength and loss of flexibility, which are the chief functions of the hand. Prevention of disability from hand injuries is the primary goal of treatment. Maintenance of function rather than cosmesis is of paramount concern in the management of hand injuries. The most commonly reported complication is stiffness [15,16]. Extensor lag, infection, tendon rupture, malunion and non-union also are common [17] Infection rates in metacarpal fractures are low. Poor outcomes are directly correlated to the higher degrees of soft tissue injury and contamination [18-20].
Aim of the Work
Assessment of management of unstable oblique and spiral metacarpal fractures by open reduction and internal fixation using mini-plates compared to percutaneous Kirschner wire fixation.
Patients
The study included 40 patients presented at Emergency Hospital, Faculty of Medicine, Mansoura University, with 48 fractured metacarpals in 30 hands. 20 patients were fixed by open reduction and internal fixation using mini-plates (group A), the other 20 patients were fixed by percutanous K wires (group B).
Inclusion Criteria
i. Unstable spiral and oblique shaft fractures of all metacarpals
ii. Age >18 years old
iii. Recent metacarpal fractures
iv. Closed fractures
Exclusion Criteria
i. Comminuted shaft and condylar fractures
ii. Metacarpal fractures in children <18 years old
iii. Old Metacarpal fractures
iv. Open fractures
Type of Anaesthesia
General anaesthesia was used in 80% of patients in group A compared to 60% of patients in group B. on the other hand, regional anaesthesia was used in 20% of patients in group A compared to 40% of patients in group B.
Duration of the Surgery
Duration of the surgery ranged between 40 to 90 minutes in group A with a mean of 65 minutes, while in group B ranged between 10 to 45 minutes with a mean of 27.5 minutes.
Methods
Initial Assessment
40 Patients with unstable spiral and oblique fractures were seen at emergency room and thorough examination and assessment was conducted including:
History taking
The range of age of the patients was from 16 to 50 years old, 27 patients were males and 13 patients were females, 22 patients had hard manual or industrial work, while 18 patients had office jobs or domestic work.
Non-patients involved in the current study were diabetic, hypertensive nor having other debilitating diseases. 23 patients were injured by direct blow by a hard object and 3 others were injured during heavy duty exercises, while the remaining 14 patients were injured during road traffic accidents. 18 patients were assaulted by others, while the other 22 patients were accidentally injured.
Thorough clinical Examination
a. Local neurovascular assessment.
All patients in the current study had intact distal vascularity with average digital pulp capillary refill time (2-6 seconds) and neurologically free.
b. Assessment of the tendon and soft tissues integrity. All the patients in the current study had intact tendons of the hand flexor and extensor groups and intact soft tissue coverage.
Radiological Assessment
Two different pictures are usually taken of the hand: one from the back with the palm facing down (posteroanterior, or PA, view), one from the side (lateral view, or lat).
Management
i. First aid Treatment
All patients had temporarily splint for the affected part, using thumb spica for fractures of the first metacarpal and volar slab for fractures of the other metacarpals. Limb elevation with analgesics, anti-edematous measures were given until the time of operation.
Routine laboratory investigations were done before operation.
ii. Operative Treatment
a. The operation was done under general or local intravenous anaesthesia.
b. The patient was positioned supine.
c. Tourniquet was used in cases fixed by mini-plates.
d. Preparation and Draping.
e. Fluoroscopic guidance was used in all cases fixed by percutanous K-wires.
iii. Fixation by Mini-plates
Surgical Approach
a. Fracture of the shaft of the first Metacarpal
A dorsolateral incision was made to expose the fracture.
b. Fractures of the Second and Fifth Metacarpals
A dorsoradial and dorsoulnar longitudinal incisions respectively were made with a curve at the distal or proximal end (Figure 1).
c. Fractures of the third and fourth metacarpals
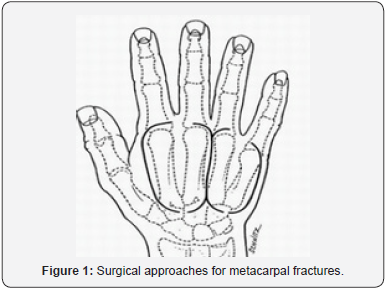
A longitudinal incision was made for these two bones, and also for internal fixation of combination of metacarpals when several bones were involved. They were placed between the metacarpal rays and were extended distally or proximally by a Y-shaped prolongation (Figure 1).
The superficial nerves and veins were identified and preserved. The extensor tendons with the paratendons were retracted. The periosteum was incised over the fracture in the longitudinal direction leaving as much as possible and preserving origins of the interosseous muscles. After surgical exposure, the fracture was opened, and the fracture line was inspected to determine the optimal position of the plates and the number of screws. Tourniquet was deflated with proper haemostasis for bleeding points. Closure of the skin. Postoperatively, a removable dorsal short arm splint was applied, and full wrist and finger motion exercises were encouraged. Sutures were removed within 14-16 days (Figures 2-4).



iv. Fixation by Percutanous K-wires
Surgery was performed under fluoroscopic guidance. The fracture was reduced using the closed method, in which the metacarpophalangeal and proximal intrphalangeal joints are flexed to an angle of 90 degrees, and upward pressure with traction was applied on the flexed finger to correct dorsal angulation and rotational deformity. Once the fracture was reduced, a K-wire was inserted through the metacarpal head in the retrograde direction, while reduction is maintained. After insertion of the first K-wire, another K-wire was inserted in the same manner for angular and rotational fracture stability. Then, the wrist was maintained into a fully flexed position, and the wires were sequentially advanced farther through the dorsal subchondral bone of the metacarpal bone, soft tissue overlying the carpal bone, and dorsal skin. The distal end of the wires was just within the subchondral bone of the metacarpal head, clear of the articular surface. The wires were bent back distally the point of bending being where the wires emerged from the metacarpal. This bend takes the wires clear of the wrist joint.
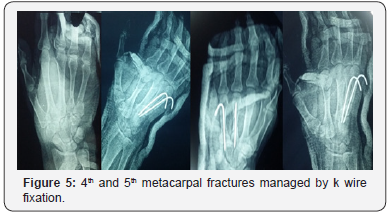

Postoperatively, a well-molded short arm slap, ulnar gutter or radial gutter in the intrinsic-plus position was applied for all the patients. Patients were encouraged to start full finger motion active and passive exercises within the splint the following day. Five weeks after surgery or when there were radiographic signs of bone healing, the wires were removed and patients were encouraged to perform wrist and finger motion exercises more vigorously without a splint (Figures 5 & 6).
Results
DASH Score
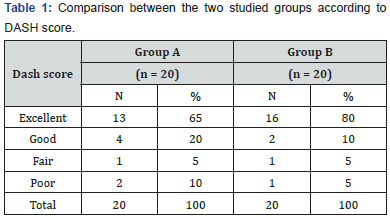
DASH score at final follow up (after 3 months) in group A was excellent in 13 patients (65%), good in 4 patients (20%), fair in 1 patient (5%) and poor in 2 patients (10%), while in group B, results were excellent in 16 patients (80%), good in 2 patients(10%), fair in 1 patient (5 %)and poor in 1 patient (5%) (Table 1) (Figure 7).

Union
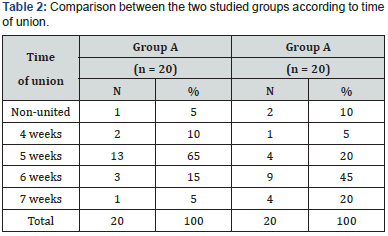
In group A, time of union ranged between 4 and 5 weeks, however one patient did not achieve union. While in group B, time of union ranged between 6 and 7 weeks. Although the mean time of union was better in group A, the results were statistically insignificant (Table 2).
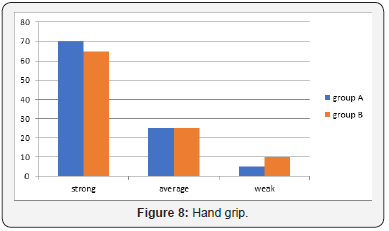
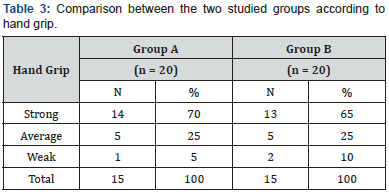
Hand grip
In group A, 14 patients had strong hand grip (70%), 5 patients had average hand grip (25%), one patient had weak hand grip (5%). While in group B, 13 patients had strong hand grip (65%), 5 patients had average hand grip (25%), 2 patients had weak hand grip (10%). Although the hand grip was better in group A, the results were statistically insignificant (Table 3) (Figure 8).
Final Results
In the present study, it was found that after 6 weeks of follow up, group A showed 93.3 % satisfactory results, while group B showed 86.7 % satisfactory results, while after 3 months of follow up both groups yielded satisfactory results in 93.3 % of cases. These results were comparable to the results of other studies:
As regard closed reduction and percutaneous intramedullary K-wire fixation, satisfactory results were reported by Elmaraghy and co-workers in 76 % of cases [21], while Eaton et al reported satisfactory results in 90 % of cases [22]. Segmuller et al. [23] in 1971, used open reduction and plate fixation and showed excellent results in 84.9% and poor in 15.1%.
Conclusion
There is no significant difference of the outcomes between mini-plates and percutaneous K-wires in management of unstable spiral and oblique metacarpal fractures. Mini-plates fixation in oblique and spiral fractures provide stable and rigid internal fixation that allows early active range of motion and early excellent results. Percutaneous K-wire fixation has the advantages of preserving the soft tissue.
References
- Kollitz KM, Hammert WC, Vedder NB, Huang JI (2014) Metacarpal fractures: treatment and complications. Hand 9(1): 16-23.
- Chung KC, Spilson SV (2001) The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am 26(5): 908- 915.
- Gudmundsen TE, Borgen L (2009) Fractures of the fifth metacarpal. Acta Radiol 50(3): 296-300.
- Bloom JM, Hammert WC (2014) Evidence-based medicine: Metacarpal fractures. Plast Reconstr Surg 133(5): 1252-1260.
- Chinchalkar SJ, Gan BS (2003) Management of proximal interphalangeal joint fractures and dislocations. J Hand Ther 16(2): 117-128.
- Ali H, Rafique A, Bhatti M, Ghani S, Sadiq M, et al. (2007) Management of fractures of metacarpals and phalanges and associated risk factors for delayed healing. J Pak Med Assoc 57(2): 64-67.
- Kamath JB, Naik DM, Bansal A (2011) Current concepts in managing fractures of metacarpal and phalangess. Indian J Plast Surg 44(2): 203- 211.
- Wilson RL, Carter MS (1978) Management of hand fractures. In: Hunter JM, Schneider LH, Mackin EJ, Callahan AD, editors. Rehabilitation of the Hand. CV Mosby St. Louis, Missouri, USA, pp. 180-194.
- Flatt AE (1972) Fractures: The Care of Minor Hand Injuries. (3rd edn), St. Louis, CV Mosby, Missouri, USA.
- Simonetta C (1970) The use of “A.O.” plates in the hand. Hand 2(1): 43–45.
- Kumar VP, Satku K (1995) Surgical management of osteochondral fractures of the phalanges and metacarpals: A surgical technique. J Hand Surg Am 20(6): 1028-1031.
- Ashkenaze DM, Ruby LK (1992) Metacarpal fractures and dislocations. Orthop Clin North Am 23(1): 19-33.
- De Jonge JJ, Kingma J, van der Lei B (1994) Fractures of the metacarpals. A retrospective analysis of incidence and etiology and a review of the English-language literature. Injury 25(6): 365-369.
- Axelrod TS (1999) Metacarpal Fractures. Hand Surgery Update 2. 1999: 11-17.
- Swanson AB (1970) Fractures involving the digits of the hand. Orthop Clin North Am 1: 261-274.
- Page SM, Stern PJ (1998) Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am 23(5): 827-832.
- Fusetti C, Meyer H, Borisch N, Stern R, Santa DD, et al. (2002) Complications of plate fixation in metacarpal fractures. J Trauma 52(3): 535–539.
- Chow SP, Pun WK, So YC, Luk KD, Chiu KY, et al. (1991) A prospective study of 245 open digital fractures of the hand. J Hand Surg Br 16(2): 137-140.
- McLain RF, Steyers C, Stoddard M (1991) Infections in open fractures of the hand. J Hand Surg Am 16(1): 108-112.
- Gonzalez MH, Jablon M, Weinzweig N (1999) Open fractures of the hand. J South Orthop Assoc 8(3): 193-202.
- Elmaraghy MW, Elmaraghy AW, Richards RS, Chinchailker SJ, Turner R, et al. (1998) Transmetacarpal intramedullary K-Wire fixation of proximal phalangeal fractures. Ann Plast Surg 41(2): 125-130.
- Eaton RG, belsky MR, lane LB (1984) Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am 9(5): 725- 729.
- London PS (1971) Sprains and fractures involving the interphalangeal joints. The Hand J 3(2): 155-158.






























