What is Degeneration of Intervertebral Disc, Cause and Its Medical Management?
Neha Saini and Priyanka Kumari*
MM Institute of Nursing, Maharishi Markandeshwer University, India
Submission: March 01, 2018; Published: March 19, 2018
*Corresponding author: Priyanka Kumari, Assistant Professor, MM Institute of Nursing, Maharishi Markandeshwer University, MullAna Ambala, Haryana, India, Email: priyankakumari@mmumullana.org
How to cite this article: Neha Saini, Priyanka Kumari. Solitary Osteocartilaginous Exostosis in a Developing Community. Ortho & Rheum Open Access 2018;11(2): 555806. DOI: 10.19080/OROAJ.2018.11.555806
Abstract
The development of disc degeneration is cell-mediated reaction to progressive structural malfunction. A degenerate disc is sign of ageing which lead to failure of structural abnormalities. Intervertebral disc degeneration may lead to biological and physical mechanism because of adjective remodeling.
Keywords: Degeneration, Intervertebral disc, Remodeling
Introduction
Degeneration of lumber disc mainly takes place in humans. There are several factors like aging, collagen abnormalities, apoptosis, vascular in growth that are according to this condition. Disc is active thing in itself that carry consequential technique for self repair [1]. Disc degeneration process is an abnormal cell mediated response to continuous structure failure combined with accelerated or faster signs of aging.
Anatomy and Physiology of Disc Degeneration & Methods
Inter vertebral disc are fibro cartilaginous pads which permits limited movements for resisting spinal compression. The intervertebral disc is consisting of elements like central portion of disc which contains nucleus populous whereas outer portion is annuls fibrosis. Nucleus populous consist of cells from primitive notochord and annuls fibrosis is composed of concentric layers of inter-mined annulas bands. , for resisting forces on the lumbar spine, these annular bands are designed in specific pattern further annular bands are divided into its inner fibers and outer fibers or s harpy fibers attached to vertebral body. The anterior and posterior longitudinal ligament strengthens the disc space. The posterior longitudinal ligament is considered less strong than anterior longitudinal ligament because all attaches more toughly to vertebral edges [2].
Disc Vascularity
Disc is a structure of low metabolic rate and its nutrition is received by the process of diffusion and supplied via capillary beds of end plate of cartilaginous vertebral body [3] with the application of acetyl chlorine the blood flow of these capillary bed increases which is under the human control [4]. The blood is supplied from the interosseous arteries from distal branches which also supplies the vertebral body [5]. Any kind of change in vascular supply rises to disc degeneration.
Collagen Distribution
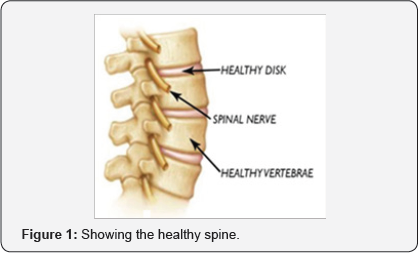
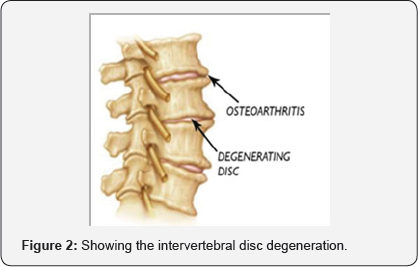
Type 1 collagen is mainly found in skin, tendon, bone, and this collagen also found in annulus fibrosis and nucleus pulpous in normal and pathologically degenerated discs. In areas of minor disc degeneration type 2 and type 9 found to be elevated [6] (Figures 1 & 2).
Etiological Factors Related to Intervertebral Disc Degeneration
The main cause of disc degeneration is considered past medical conditions like arthritis, osteoporosis, and disc aging, histological changes like decrease blood supply to vertebral endplate, decreased disc cell density and some changes also occurs due to decompressed nucleus [7].
Sign and Symptoms
Sign and symptoms appears in disc degeneration is sudden unexpected pain in lower back which radiates to legs, numbness and tingling sensation in leg and foot as well as muscle weakness [8].
Diagnostic Evaluation
Lower back Pain is the major symptom for the intervertebral disc degeneration. After taking the medical history of the patient will be send for radio imaging X ray, CT scan, MRI, disco gram to identify the herniated and compressed disc [9,10].
Treatment of Disc Degeneration
Medical management of intervertebral disc degeneration includes intake of analgesics to reduce pain like acetaminophen, steroids for reducing swelling of nerves. Non- steroidal anti inflammatory drugs like aspirin are used to reduce the inflammation. Surgical treatment is to restore disk space height as well as to decompress spinal nerves but in case of disc degeneration surgery is recommended rarely unless symptoms have not improved with medical treatment or other therapies. It involves two surgeries like spinal fusion and motion preservation surgery. In spinal fusion the bony vertebrae (1 or 2) fused together permanently whereas motion preservation surgery is done to steady spine without bones fusion together.It includes artificial disc replacement in which damaged disc is removed [11,12].
References
- Humzah MD, Soames RW (1988) Human Intervertebral disc. Structure and Function. Anat Rec 220(4): 337-356.
- Bogduk N (1976) The anatomy of the lumbar Intervertebral disc syndrome. Med J Aust 1(23): 878-881.
- Crock HV, Goldwasser M (1984) Anatomic studies of the Circulation in the region of the vertebral end plate in adult greyhound dogs. Spine 9(7): 702-706.
- Wallace AL, Wyatt BC, McVarthy ID (1994) Humeral regulation plat of blood flow in the vertebral endplate. Spine 19(12): 1324-1328.
- Roberts S, Manage J, Urban JP (1989) Biochemical and Structural properties of the Cartilage end plate and its relation to the Intrvertebral disc. Spine 14(2): 166-174.
- Nerlich AG, Boos N, Wiest I, Aebi M (1998) Immunolocalization of major interstitial collagen types in human lumbar intervertebral disc of various ages. Virchows Arch 432(1): 67-76.
- Kalichman L, Hunter DJ (2008) The genetics of Intervertebral disc degeneration. Associated genes. Joint Bone Spine 75(4): 388-396.
- Lotters F, Burdorf A, Kuiper J, Miedema H (2003) Model for the workrelatedness of low-back pain. Scand J Work Environ Health 29(6): 431440.
- Modic MT, Masaryk TJ, Ross JS, Carter JR (1988) Imaging of degenerative disk disease. Radiology 168(1): 177-186.
- Modic MT, Steinberg PM, Ross JS, Masaryk TJ, Carter JR (1988) Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 166(1): 193-199.
- Wehling P, Schulitz KP, Robbins PD, Evans CH, Reinecke JA (1997) Transfer of genes to chondrocytic cells of the lumbar spine: proposal for a treatment strategy of spinal disorders by local gene therapy. Spine 22(10): 1092-1097.
- Nishida K, Kang JD, Suh JK, Robbins PD, Evans CH, et al. (1998) Adenovirus-mediated gene transfer to nucleus pulposus cells implications for the treatment of intervertebral disc degeneration. Spine 23(22): 2437-2443.






























