Tuberculosis Tenosynovitis of Flexor Digitorum Tendons: A case Report
Truc Tam Vu2 and Tri Quang Phan1
1Orthopedic department, Pham Ngoc Thach University of Medicine, Vietnam
2Spinal surgeries department B, Hospital for Traumatology and Orthopedics, Vietnam
Submission: January 25, 2018; Published: February 15, 2018
*Corresponding author: True Vu, Spinal surgeries department B, Hospital for Traumatology and Orthopedies at Ho Chi Minh eity, 929 Tran Hung Dao street, 5th district, Vietnam, Tel: +84 28 3923 7007; Email: tamtruc240384@yahoo.com
How to cite this article: Tri Quang Phan, Truc Tam Vu. Tuberculosis Tenosynovitis of Flexor Digitorum Tendons: A case Report. Ortho & Rheum Open Access 2018; 10(4): 555792. DOI: 10.19080/OROAJ.2018.10.555792
Abstract
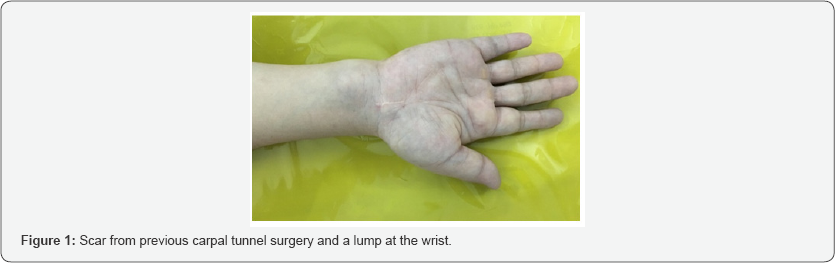
Tuberculosis infections in developing countries like Vietnam are currently the one of the most challenging problems. Among musculoskeletal involvement, upper limb affection is relatively rare. A 46 year-old female patient came to our department of Upper Limb Surgery because of a progressive swelling of her Right wrist in six months with no response to oral anti-inflammatory medications. Two years before, she had a surgery to treat her carpal tunnel syndrome of the same wrist with a satisfactory result. On clinical examination, beside a scar from previous operation, a 3 x 4 cm lump with well define margin and normal overlaying skin was noticed. Blood tests were normal except a rise of ESR and C-reacitve protein. Ultrasound suspected a ganglion of the wrist.
T2 MRI showed synovial fluid collection in flexor tendon sheath, thickened tenosynovium with heterogeneous signal, highly suspecting a condition of tuberculosis tenosynovitis. The patient underwent a surgical treatment with synoviectomy and thorough debridement. The biopsy result showed a synovial and fibro collagenous tissue infiltrated by multiple epitheloid aggregates, Langerhans giant cells with presence of central caseous necrosis, which confirm the diagnosis of tuberculosis. Nine-month chemotherapy was indicated and at final follow-up, there was no sign of recurrence and the patient was satisfied with the treatment result. Tuberculosis tenosynovitis of the wrist area can occur with insidious onset and confusing clinical symptoms and therefore, early diagnosis remains a challenge for physicians and surgeons. MRI is considered as a useful imagery test to orient the diagnosis.
Keywords: Tuberculous synovitis; Anti-tuberculous chemotherapy; Caseous necrosis
Abbreviations: ESR: Erythrocyte Sedimentation Rate; MRI: Magnetic Resonnance Imagery
Introduction
Tuberculosis infections in developing countries like Vietnam are currently the one of the most challenging problems. Musculoskeletal involvement represents 10-15% of all extra pulmonary cases. Upper extremity involvement is relatively rare. Tuberculosis tenosynovitis is usually misdiagnosed as nonspecic tenosynovitis. Therefore, it is important to correct diagnosis in order to avoid mistreatment. This article is going to describle one case of tuberculosis tenosynovitis.
Case Report
A 46 year-old female patient was admitted to our department of Upper Limb Surgery due to a progressive swelling at her Right wrist. Two years ago the patient was diagnosed tunnel carpal syndrome on right hand and operated by releasing the tunnel carpal. The result was satisfying and the postop follow-up was uneventful. All her signs and symptoms have disappeared overtime. However, 6 months ago, she has noticed a swelling on her right wrist just proximal to the scar of the carpal tunnel operation. Despite that she had no numbness or pain, the progression of the condition made her worry and she has visited hospitals and private clinics before visiting our hospital. She was treated with oral medications for months without any obvious results. No constitutional symptoms such as loss of weight, loss of appetite, night fever have been noticed. She had no past history of pulmonary tuberculosis and family history was irrelevant. No history of local steroid injection in the right hand or wrist, either before or after the previous surgery.
At admission, physical examination revealed (Figure 1):
i. A scar at her Right wrist.
ii. An approximately 3x 4cm lump proximal to the wrist line with well defined margin and normal overlying skin, relatively soft with no tenderness at palpation.
iii. A normal range of motion of Right wrist and hand with full strength of extrinsic and intrinsic hand muscles.
iv. A negative Phalen and Tinel tests.
v. No thenar atrophy.
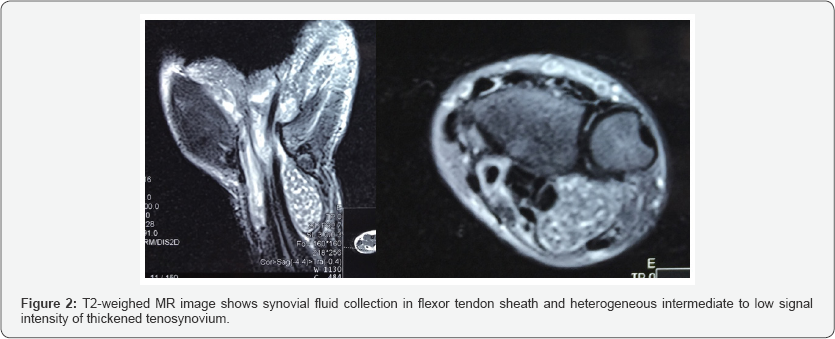

Systemic examination was normal. Blood tests including blood count test, C-reative protein and erythrocyte sedimentation rate were within normal values. The wrist ultrasound revealed a suspected ganglion at right wrist. The T2 weighed MRI of affected area showed synovial fluid collection in flexor tendon sheath, thickened tenosynovium with heterogeneous signal, highly suspecting a condition of tuberculosis tenosynovitis (Figure 2). The surgical management involved exploring the Right wrist by using the previous incision line, which revealed a swelling tendon sheath of both flexor digitorum superficial is and profundus containing synovial fluid and numerous yellowish rice bodies inside (fig 3). Pathological tissue was removed and thorough debridement was preformed. Care was taken in order to protect the tendons. Specimen of rice bodies and synovium were sent to the Pathology department for histopathological study.
The biopsy result showed a synovial and fibro collagenous tissue infiltrated by multiple epitheloid aggregates, Langerhans giant cells with presence of central caseous necrosis. The conclusion confirmed a tuberculous tenosynovitis. Polymer chain reaction and culture of tuberculosis were negative. With a confirmation from the biopsy test, antituberculous chemotherapy was started immediately postop with a nine- month protocol. There was no sign of recurrence at final follow- up (Figure 4). She could return to her previous job and was satisfied with the treatment result.

Discussion
With an onset often insidious and a slow and benign progression, early diagnosis of tuberculosis tenosynovitis can be challenging for physician. Non specific symptoms including swelling, pain, and diminished range of motion at later stages can occur in other musculoskeletal conditions. Patients may be admitted because of symptoms of tenosynovitis, peripheral carpal tunnel syndrome and a non-specific synovitis mimicking De Quervain's disease or gout [1].
The disease may present in one of four stages depending on the duration of the infection and host immunity [2].
i. Stage 1 which involves a thin synovitis with free synovial may be seen.
ii. Stage 2 can occur up to 2 years after the onset, characterized by granulation tissue, thick tenosynovial pro-liferation, and rice bodies appear.
iii. Stage 3 is defined when the infection invades the tendons. They may be frayed, ruptured, or becomes caseated. Fraying of tendons occurs at an average of 3 years and rupture of tendons occurs at an average of 4 years from the onset of tenosynovitis.
iv. Stage 4 occurs very late, the infection spreads to the adjacent joints or bone and a sinus may be present with or without superim-posed pyogenic infection.
In our case, rice bodies appeared, and the flexor tendons still had a smooth surface and especially there was no evidence of the invasive infection into. According to the above classification, the condition of our patient is classified as second stage. The disease probably started more than 2 years with the onset which was tunnel carpal syndrome. The patient was operated by released the tunnel carpal (transverse carpal ligament was released). All signs of the tunnel carpal syndrome were reduced such as Phalen test and Tinel test negative; however, the treatment may be inadequate and therefore the disease would have been progressing.
The differential diagnosis for tuberculosis tenosynovitis includes rheumatoid arthritis, pyogenic infection, gouty arthritis, giant cell tumor of the tendon sheath, and fungal tenosynovitis. Diagnosis of articular involvement depends on the isolation of the organism from synovial fluid or synovial biopsy. Prompt diagnosis is critical to preserve joint function and anatomy. The patients who have tuberculosis tenosynovitis are usually misdiagnosed for having nonspecific tenosynovitis. Rheumatoid synovitis is another condition that should be taken into consideration for differential diagnosis. Misdiagnosing as rheumatoid or nonspecific tenosynovitis could lead to steroid injections, which aggravates the infection. [3].
The confirm diagnosis of tuberculosis is made by histologic and microbiologic studies [4]. Blood tests and imaging before biopsy may be helpful for the diagnosis. Wrist X-ray imaging in tenosynovitis may show soft tissue swelling and osteoporotic changes around the wrist joint. T2-weighed MRI is the most useful imagery test to orient the diagnosis. On T2-weighted sequences, hypointense focus, hypointense synovial membrane together with central erosion, and abscesses with surrounding contrast are significant for distinguishing tuberculosis from other genres of inflammatory arthritis [5].
There are different reports regarding the treatment options of hand and wrist tuberculous tenosinovitis. Surgical treatment without antituberculous chemotherapy often results in recurrence. Bush and Schneider [6], Cramer et al. [7], and Regnard et al. [8] had reported good clinical results with surgical treatment and antituberculosis chemotherapy combination. Visuthikosol et al. [9] had compared antituberculous chemotherapy and surgery chemotherapy combination. No recurrence occurred in both groups. Kotwal & Khan [2] had reported successful clinical results with only antituberculous chemotherapy. Surgery should be considered if there is no response up to 8 weeks of antituberculous chemotherapy. However, in daily clinical practice in our country, most of these cases are diagnosed after histological examination following the surgical debridement and synovectomy. If the formation of rice bodies was noticed, the wide surgical debridement would be indicated to avoid the recurrences [10].
In our case, the patient was managed by synoviectomy and debridement of the inflammatory tendon sheath (2nd stage: the present of rice bodies) associated with the 9-month antituberculous chemotherapy protocol. At final follow-up, there was no sign of recurrence and the patient was satisfied with the treatment result.
References
- Ozçelik IB, Aydin A, Sezer I, Oztaj S (2006) Treatment algorithm in synovial tuberculosis of the hand and wrist: a report of three cases. Acta Orthop Traumatol Turc 40(3): 255-259.
- Kang HJ, Park SY, Shin SJ, Kang ES, Hahn SB (2009) Tuberculous tenosynovitis presenting as carpal tunnel syndrome. J. Korean Soc Surg Hand 5: 137-141.
- Ergun T, Lakadamyali H, Aydin O (2008) Multiple rice body formation accompanying the chronic nonspecific tenosynovitis of flexor tendons of the wrist. Radiat. Med 26: 545-548.
- Butorac R, Littlejohn GO, Hooper J (1987) Mycobacterial disease in the musculo skeletal system. Med J Aust 147(8): 388-391.
- Hsu CY, Lu HC, Shih TT (2004) Tuberculous infection of the wrist: MRI features. Am J Roentgenol 183(3): 623-628.
- Bush DC, Schneider LH (1984) Tuberculosis of the hand and wrist. J Hand Surg Am 9(3): 391-398.
- Cramer K, Seiler JG III, Milek MA (1991) Tuberculous tenosynovitis of the wrist. Two case reports. Clin Orthop Relat Res 262: 137-140.
- Regnard PJ, Barry P, Isselin J (1996) Mycobacterial tenosynovitis of the exor tendons of the hand. A report of ve cases. J Hand Surg Br 21: 351354.
- Visuthikosol V, Kruavit A, Nitiyanant P (1996) Tuberculous in- fection of the hand and wrist. Ann Plast Surg 37: 55-59.
- Kotwal PP, Khan SA (2009) Tuberculosis of the hand: clinical presentation and functional outcome in 32 patients 91(8): 1054-1057.
- Dlimi F, Bellarbi S, Mahfoud M, Berrada MS, El Bardouni A, et al. (2011) Tuberculosis of the hand and wrist: different aspects of 30 cases. Chir Main 30(3): 198-204.






























