Arthroscopic Management of Slap Lesion
*Amr Hussien
Department of orthopedics, Banha University, Egypt
Submission: June 28, 2017; Published: July 06, 2017
*Corresponding author: Amr Hussien, Department of orthopedics, Banha University, Banha, Egypt, Email: YAMANYAMR@GMAIL.COM
How to cite this article: A Hussien. Arthroscopic Management of Slap Lesion. Ortho & Rheum Open Access 2017;7(4): 555718. DOI: 10.19080/OROAJ.2017.07.555718
Introduction
Superior glenoid labrum tears as a source of shoulder pain were first described by Andrews et al. [1] in 1985 in the context of the high demand throwing athlete (professional baseball pitchers). The pathology correlated with the immense stress placed on the shoulder and the biceps brachial is muscle during the throwing motion. In 1990, Snyder [2] coined the term Superior Labrum Anterior and Posterior (SLAP) tear to describe the pathology of the labrum in overhead throwing athletes. Four unique types of superior labrum pathology were classified after inspection via arthroscopy.
While the lesions that Andrews and Snyder described were associated with athletic injuries, it has been demonstrated that SLAP lesions are often found in association with other shoulder pathology especially rotator cuff tears in older patients with chronic shoulder overuse and shoulder instability [3]. The mechanism of injury can be either repetitive stress or acute trauma with the superior labrum most vulnerable to injury during the late cocking phase of throwing [3]. SLAP tears are routinely diagnosed using clinical diagnosis and Magnetic Resonance Imaging (MRI). MRI signs of a SLAP lesion include increased signal of the glenoid labrum with or without extension into the biceps tendon and cleavage of the superior glenoid labrum [4]. Synder et al. [2] subsequently described SLAP lesions in the general population and classified the lesion into 4 types. These include:
i. Type 1 (11%) - Marked fraying of the free edge of the superior labrum.
ii. Type 2 (41%) - Avulsion of the labral-bicipital complex from the glenoid.
iii. Type 3 (33%) - Displaced bucket handle tear of the superior labrum with an intact biceps anchor.
iv. Type 4 (15%) - Bucket handle tear of the superior labrum, with extension into the biceps tendon [2].
Patient selection is based on study of 25 patients with SLAP lesion who are candidates for the arthroscopic repair because of their high physical demands, aged 20 to 60 years old. Any patient with one or more of the following criteria is excluded from this study.
a. Old age (Above 60 years).
b. Younger age (below 20 years)
c. Multidirectional instability.
d. Associated arthritis.
e. Diabetic patients.
Clinical Evaluation
The patient with a SLAP tear will frequently complain of deep, nonspecific pain. Often they will localize the pain posteriorly. Symptom onset may be related to trauma, repetitive overuse, or may be insidious in nature. In addition to complaints of pain, patients may relate feelings of instability catching, grinding, or weakness [5]. SLAP lesions may coexist with other shoulder disorders including impingement, rotator cuff tears, instability, acromioclavicular arthrosis, and perilabral cysts. The nonspecific nature of the complaints juxtaposed with other associated pathologies combine to make diagnosis by history difficult Physical examination is equally problematic. Numerous examination maneuvers have been described including Speed's biceps tension test, Yergason's test, the apprehension test, the O'Brien maneuver [6], the crank test [7], Kim’s biceps load test [8], and the Jobe relocation test [9].
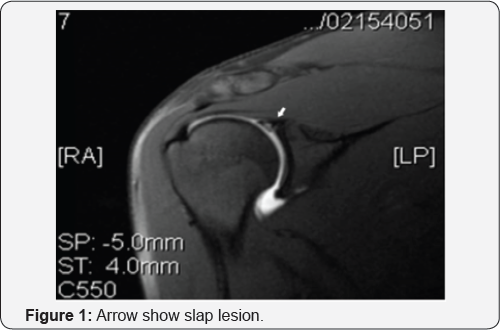
A study by Guanche and Jones [10] found only the O'Brien maneuver, the Jobe relocation test, and the apprehension sign to correlate with the presence of a SLAP tear found at arthroscopy. Even combined, none of these showed diagnostic specificity. It is recommended that multiple maneuvers be performed when examining a shoulder with a suspected SLAP tear, and the combined results may be suggestive but not definitively diagnostic. Imaging, like history and physical examination, can be suggestive but not completely sensitive. Plain radiographs, although indicated in the evaluation, are generally noncontributory. Magnetic resonance imaging, especially when performed with intra-articular gadolinium, can aid in the diagnosis ( Figure 1). Sensitivity is approximately 80% with specificity over 95% [11]. In short, the diagnosis of SLAP tears through all means can be a challenge. When history, examination, and imaging all suggest the diagnosis, then it is reasonable to pursue definitive treatment via arthroscopy.
Operative Technique
The initial operative evaluation involves an examination under anesthesia. The shoulder is examined to assess passive range of motion, inferior sulcus translation compared with the contra lateral side, and presence of asymmetric anterior or posterior load and shift at 0° and 90 of forward elevation in the scapular plane [12]. A diagnostic arthroscopy is performed next. Arthroscopy may be performed in either the beach chair or lateral decubitus position. The glenohumeral joint is evaluated via a standard posterior viewing portal and an anterior rotator interval working portal. Areas to be probed and visualized include the articular surfaces, the biceps tendon, the glenoid labrum, and the rotator cuff.
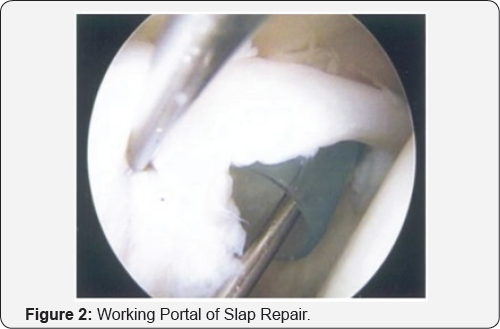
The biceps tendon, biceps anchor, and superior labrum are probed for areas of fraying or instability. An unstable or type II SLAP tear is present when the superior labrum can be displaced with a probe beyond the articular cartilage margin of the glenoid, thereby exposing underlying subchondral bone. Areas of fraying are debrided. Portals are established through which repair of an unstable SLAP is performed. Most repairs are performed through the anterior-superior rotator interval portal combined with a posterior-lateral portal of Wilmington ( Figure 2) [13]. After debridement of labral fraying, the glenoid neck and rim are abraded with a burr or shaver. Suture anchors are inserted through the working portals at an angle of approximately 45° onto the glenoid rim. Suture anchors are placed at the 10, 11, 1, or 2 o'clock positions on the glenoid depending on the anterior and posterior extent of superior labral detachment. Typically, 2 or 3 anchors are used per repair.
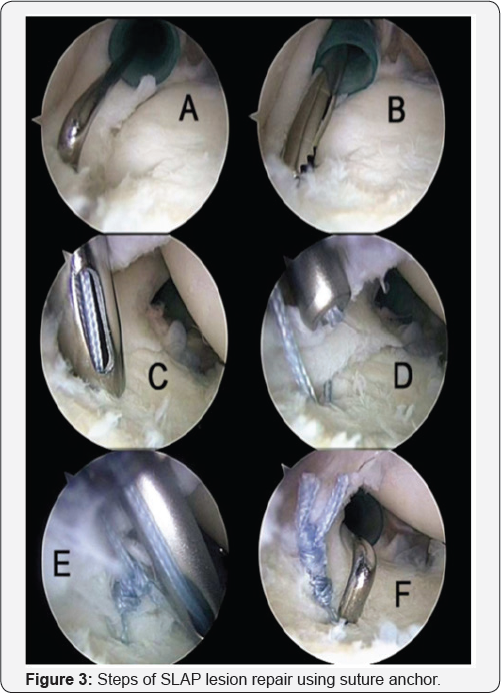
A single vertical stitch from each suture anchor is placed around the inner edge of the labrum centrally and through the capsulolabral tissue peripherally using an arthroscopic piercing instrument loaded with a shuttle suture (LinvatecInc, Largo, FL) or using a suture lasso (Arthrex, Naples, FL). A sliding arthroscopic knot reinforced with alternating halfhitches is used to secure the labrum to the glenoid ( Figure 3). After the SLAP repair, any associated pathology is addressed as appropriate.
Postoperatively, patients participate in a detailed rehabilitative protocol under the supervision of a physical therapist. Sling immobilization with pendulum, elbow, and wrist exercises are initiated during the first 3 to 6 weeks. At 3 to 6 weeks, passive and active-assisted range-of-motion exercises are begun. After 6 weeks, progressive strengthening of the rotator cuff and the scapular stabilizers is initiated. Three months after the operation, patients progress to an aggressive exercise program. Full participation in throwing sports is allowed after 6 months. Patients are returned to full active duty when at least 80% of motion and strength are regained and when they are able to confidently perform the physical requirements of their military occupational specialty.
Results
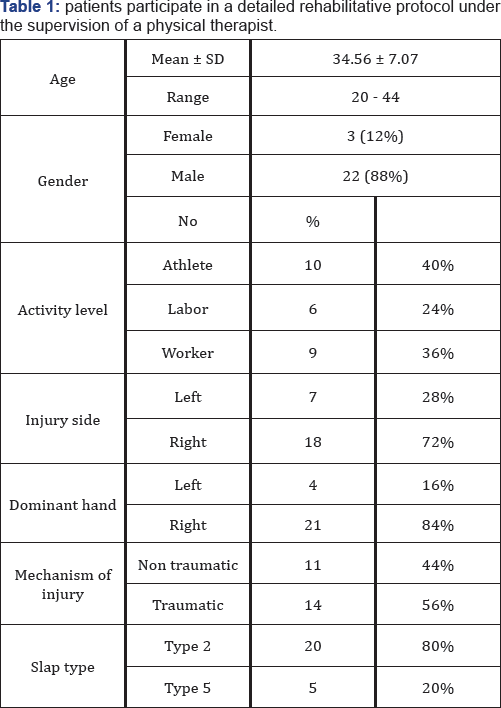
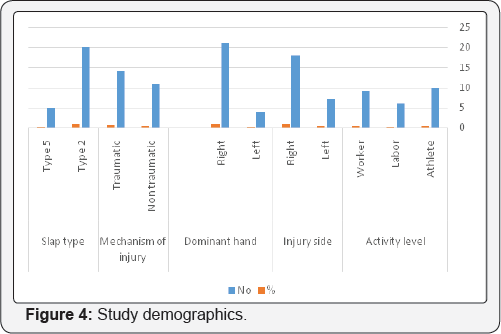
Twenty-two of the patients in this study were males with only 3 females. The mean age at the time of operation was 34.56 ± 7.07 ranging from 20 to 44 years. All patients were unilaterally involved with the dominant side being affected in 20 patients and the non-dominant side in only 5 patients. Ten of the 25 patients were athletes (Table 1).
Type of lesion
20 of the 25 patients (80%) suffered from a type 2 SLAP while the remaining 5 (20%) suffered from a type 5 SLAP, figure 52. Six of the patients (24%) had an isolated SLAP lesion while the remaining 19 (76%) had associated lesions; 8 had associated bankart lesion, 9 had subacromial impingement, 1 had C shaped acromine need acromioplasty, 1 one had a small PASTA (Partial Articular Side Tendon Avulsion) lesion. Seven of the patient (26%) had central position anchor, 18 patients (72%) had non central position of the anchor. Sixteen of the patients (64%) had 1 anchor for fixation of SLAP, nine patients (36%) had 2 anchor Patients were assessed pre-operatively and at 6 and 12 months post-operatively using UCLA score. UCLA score before operation was 17.56 ± 2.33 with range from 13-21. UCLA score after 6 months from operation was 28.72 ± 4.02 with range from 14-33.
UCLA score after 12 months from operation was 31.40 ± 3.37 with rang from 21-35. Table 2 show UCLA score before operation and 6 months after and 12 months after operation. Comparing UCLA score before operation with UCLA score at 6 months and at 12 months showed highly significant improvement before and 6 months (p < 0.001) and 12 months after operation (p < 0.001). There is no significant relation between sex and UCLA score after 6 month and 12 months (P-value 0.785, 0.299 respectively). Although there was statistically significant better in left dominant before operation (P- value <0.05), no statistically significant difference after 6 month and 12 months (P- value >0.05). Although there was better UCLA score at non traumatic patient, there was statistically insignificant before after 6 month and 12 months (P >0.05). There was statistically insignificant between central and non-central position of the anchor (P >0.05) before, after 6 months and 12 months after operation. No statistically insignificant relationship between the number of the anchor 6 month, 12 month and UCLA score (P >0.05). There was statistically significant inverse correlation found between age of the studied patients and UCLA score at 12 months while no statistically significant correlation found between age and UCLA score before operation or at 6 months ( Figures 4 & 5).


Discussion
Despite being unveiled to the orthopedic community by Snyder [4], the diagnosis of SLAP lesions still remains a controversial issue. This controversy extends from the clinical tests for SLAP up to arthroscopic evaluation. This was evident by the study done by Gobezie et al. in which revealed that there is substantial interobserver and intraobserver variability among experienced shoulder arthroscopic specialists with regard to diagnosis and treatment of SLAP tears. Intraobserver agreement using the Snyder classification indicated only moderate agreement [14]. Aydin N et al. [15] also evident that by study that reveal that diagnosis of the SLAP tears is based on clinical history, a detailed physical examination and MRI. MR arthrography is the best imaging technic for evaluating SLAP lesions. But Arthroscopic SLAP repairs remain the gold standard.
Diagnosis of SLAP lesion requires a high index of suspicion with the exclusion of other causes of shoulder pain. Therefore, to be confident about our diagnosis of SLAP lesion, the history, clinical examination, and radiological studies must all point to the same direction. This high index of suspicion should be confirmed by arthroscopic evaluation in which exposed sublabral bones as well as other evidence of labral separation such as granulation tissue and fissuring are demonstrated. Many types of physical examinations are useful for the diagnosis of SLAP lesions. On the other hand, the number of tests used for SLAP assessment itself suggests that its diagnosis is difficult, and no clinical test can decisively confirm the presence of a SLAP lesion. This is evident by study done by kevin et al in which reveal Clinical examination is often difficult due to the numerous injury mechanisms and the widely varied extent of labral pathology. Proper identification of the exact mechanism and specific severity of pathology is vital to accurately diagnose and manage these injuries [16].
Gorantla et al. [17] performed a systemic review on the outcome of repair in type II SLAP lesions. The general outcome for type II SLAP repair as determined by the authors is reasonable, and the percentage of good and excellent results ranged for all patients from 40% to 94%. A frequently used measure of treatment success is return to previous level of performance before injury/surgery. For all athletes in these studies, this ranged from 20% to 94%. All the studies analyzed had a minimum of 2 years follow up. Kim et al. [18] published a Level IV retrospective study evaluating the results of arthroscopic repair of isolated superior type II SLAP tears using suture anchors in 34 patients. The mean patients' age was 26, and mean follow-up was 33±9 months. According to the UCLA scoring system, the outcome was graded as excellent in 27 patients, good in 5, fair in 2, and poor in 0, with a success rate of 94%.The mean DASH score improved from 33.2 to 13.6. In addition, 100% of patients in the non-overhead sports activity group had a good to excellent result whereas 89% of patients in the overhead sports activity group had a good to excellent result. Overall, 14 of the 34 patients (41%) were able to return to their pre-injury level of activity.
Ide et al. [19] examined the outcome of type II SLAP repair using suture anchors in overhead-throwing athletes in a Level IV case series. The mean age was 24 years and mean follow- up was 41 months by an independent examiner. According to the modified Rowe scoring system, the results were graded as excellent in 30 patients, good in 6, fair in 4, and poor in 0, translating into a success rate of 90%. Of the 40 athletes, 30 (75%) were able to return to their pre-injury level of performance without limitation. Frei et al. [20] in a retrospective study of 48 patients who underwent arthroscopic SLAP repair using bio- absorbable suture anchors showed significant improvement in Constant, ASES, VAS, and short form 12 after a minimum 2 year follow up. No differences were seen between the outcomes of non-athletes, non-overhead athletes, recreational overhead athletes, and collegiate overhead athletes, suggesting that SLAP type II repair is successful independent of the patient’s vocation or sport.
Rachel M et al. [21] in retrospective study of Sixty-two patients with an average age of 36 ± 13 years and men follow up 3.3 years by independent examiner. There were statistically significant improvements in the average ASES (preoperative: 64.8±19; postoperative: 83.9±18.3; p< 0.001), SST (preoperative: 8.6 ± 2.9; postop: 10.3 ± 2.3, p = 0.004) and VAS (preoperative: 3.3 ± 2.3; postoperative: 1.6 ± 1.9, p< 0.001) scores. Suggestion was slap repair was successful in young patient group. Reinold et al. [22] prospective study of 84% of athletes with a concomitant SLAP repair returned to competition with good to excellent outcomes using the Modified Athletic Shoulder Outcome Scale. In our prospective study 25 patients age ranging from 20 to 44 years and the mean age at the time of operation was 34.56 ± 7.07. The mean follows up period was 12 months. UCLA score before operation was 17.56 ± 2.33. After operation UCLA score became 31.40 ± 3.37. The UCLA score was excellent in 23 patients, good in 2 patients and poor in 1 patient. The patient satisfaction was 96%.
In addition, there was a statistically significant improvement in both the UCLA score between 6 and 12 months postoperatively.These results suggest, like most published studies, that rehabilitation from SLAP repair takes a longer time than most other shoulder pathologies and return to pre-injury level of activity may take up to a year. This was confirmed by Neri et al. [23] who found a mean time to return to play of 10 months' post SLAP repair in a cohort study performed on 31 athletes. In our study was show that there was statistically significant inverse correlation found between age of the studied patients and UCLA score at 12 months while no statistically significant correlation found between age and UCLA score before operation or at 6 months. This might be due to that the younger had motivation to doing well in order to return back to sport or work.
Denard et al. [24] in prospective, Level IV study Fifty-five patients were available for long-term follow-up at a mean of 77 months, concluded that 87% of cases, a good or excellent functional outcome can be anticipated after arthroscopic repair of type II SLAP lesions. They conclude a poor outcome with Workers’ Compensation cases and older age (≥40 years). In discussing the results of SLAP repair with age, Neri et al. [25] and Alpert et al. [26] in that no statistical difference was found in outcome scores with increasing age of the patient. This was despite the fact that older patients did slightly worse than younger ones. But they conclude that older patients tend to have longer recovery periods and are more prone to complications, especially stiffness, thus they require early supervised physiotherapy.
As in our study, in Boileau et al. [27] compared the outcome of type II SLAP repair with that of biceps tenodesis in a Level III cohort study. In this prospective study 10 patients with a mean age of 37 years (range, 19 to 57 years) had SLAP repairs with suture anchors, whereas 15 patients with a mean age of 52 years (range, 28 to 64 years) had a biceps tenodesis performed. Patients were not randomized, and treatment option was based on the age of the patient. The authors found an increase in Constant score in both groups, but a much higher percentage of patients were satisfied with the results of the surgery in the tenodesis group (87% v 40%). In addition, a higher percentage of athletes returned to their previous level of sports participation in the tenodesis group compared with the SLAP repair group (87% v 20%). In this study physical examinations were performed by an independent examiner. This is increase believe that with increasing patient age the slap repair will be less satisfactory.
Considering the best anchor configuration for SLAP repair, several studies have concentrated on measuring the biomechanical strength of different anchor configuration. Baldini et al. [28], in a biomechanical cadaveric study on 10 matched shoulders, found no statistically significant difference between one double loaded anchor and two single loaded anchors in terms of pullout strength. Domb et al. [29], in another biomechanical study, compared the strength of 3 common anchor configuration
a. A single simple suture anterior to the biceps;
b. Two simple sutures, one anterior and one posterior to the biceps; and
c. A single mattress suture through the biceps anchor.
Their results suggested that a single anchor with a mattress suture may be a biomechanically advantageous construct for the repair of type II SLAP lesions.
In our study, no biomechanical testing was performed, but clinical outcome showed no statistically significant difference between one or two anchor fixation. Also it showed insignificant clinical outcome with centrally placed anchors when compared to non-central anchors. In Coleman et al. [30] reviewed the results of a Level IV retrospective case series that compared the outcome of type II SLAP repair with or without concomitant acromioplasty. The study obtained follow-up in 50 of 73 patients who underwent type II SLAP repair. Both groups' SLAP tears were stabilized with a bioabsorbable tack. At follow-up, the patients completed an L'Insalata questionnaire, a physical examination, and ASES questionnaire were conducted by an independent examiner. According to both scoring systems, there was no statistically significant difference in outcome between the 2 groups after an average of 3.5 years follow up. The authors stated that 47 of the 50 patients (94%) in the study were able to return to their pre-injury level of competition.
Enad [31] performed a Level III retrospective cohort study to compare the outcome of SLAP repair between those patients with isolated SLAP injuries (group I) and those with concomitant pathologies (subacromial impingment and/or partial rotator cuff tear) (group II). The mean age was 31.6 years with a minimum follow-up of 24 months. All SLAP lesions were arthroscopically repaired with bioabsorbable suture anchors. There was no significant difference in UCLA scores between the 2 groups, with overall success rate of 92%. However, there was a statistically significant difference in the mean ASES and VAS scores. Group II had a higher ASES score and a lower VAS score compared with group I. The cohort was only matched based on age, and thus selection bias may have been introduced by not controlling other issues; such as arm dominance, acute versus chronic onset, activity level, and so on. An independent examiner was not identified, potentially introducing detection bias.
In our study 11 of the 25 patients had an associated impingement problem. In agreement with the results of Coleman et al, the results of this study showed no statistically significant difference in the UCLA score at 12 months’ post-operative between the two groups. These results, however, were not matched on other criteria such as age, level of activity, traumatic versus atraumatic onset, and type of surgery done. In addition, an independent examiner was not identified. Therefore, these factors may introduce detection bias, which may result in inaccurate conclusions.
Summary
The present study was conducted on 25 patients with a mean age of 34.56 ± 7.07 years for a mean follow up of 12 months. There were 22 males and only 3 females, with 20 dominant shoulders and 5 non-dominant shoulders. The UCLA score improved from 17.56 ± 2.33 preoperatively to 31.40 ± 3.37at 12 months' post-operative. The overall patient satisfaction was 96%. Furthermore, our results support the good clinical outcome achieved with SLAP repair especially with younger, traumatic patients, with suture anchors placed either anterior or posterior to the biceps anchor.
References
- Andrews JR, Carson WG, McLeod WD (1985) Glenoid labrum tears related to the long head of the biceps. Am J Sports Med 13(5): 337-341.
- Snyder SJ, Karzel RP, Del Pizzo W, Ferkel RD, Friedman MJ, et al. (1990) SLAP lesions of the shoulder. Arthroscopy 6(4): 274-279.
- Maffet MW, Gartsman GM, Mosley B (1995) Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med 23(1): 93-98.
- Warner JJP, Kann S, Marks P (1994) Arthroscopic repair of combined Bankart and superior labral detachment anterior and posterior lesions: technique and preliminary results. Arthroscopy 10(4): 383-391.
- Nam EK, Snyder SJ (2003) The diagnosis and treatment of superior labrum, anterior and posterior (SLAP) lesions. Am J Sports Med 31(5): 798-810.
- O'Brien SJ, Pagnani MJ, Fealy S, McGlynn SR, Wilson JB (1998) The active compression test: A new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med 26(5): 610-613.
- Liu SH, Henry MH, Nuccion SL (1996) A prospective evaluation of a new physical examination in predicting glenoid labral tears. Am J Sports Med 24(6): 721-725.
- Kim SH, Ha KI, Ahn JH, Kim SH, Choi HJ (2001) Biceps load test II: A clinical test for SLAP lesions of the shoulder. Arthroscopy 17(2): 160164.
- Hamner DL, Pink MM, Jobe FW (2000) A modification of the relocation test: Arthroscopic findings associated with a positive test. J Shoulder Elbow Surgery 9(4): 263-267.
- Guanche CA, Jones DC (2003) Clinical testing for tears of the glenoid labrum. Arthroscopy 19(5): 517-523.
- Waldt S, Burkart A, Lange P, Imhoff AB, Rummeny EJ, et al. (2004) Diagnostic performance of MR arthrography in the assessment of superior labrum anterioposterior lesions of the shoulder. AJR Am J Roentgenol 182(5): 1271-1278.
- Altchek D, Warren RF, Skyhar MJ, Ortiz G (1991) T-plasty modification of the Bankart procedure for multidirectional instability of the shoulder. J Bone Joint Surgery Am 73(1): 105-112.
- Morgan CD, Burkhart SS, Palmeri M, Gillespie M (1998) Type II SLAP lesions: Three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy 14(6): 553-565.
- Gobezie R, Zurakowski D, Lavery K, Millett PJ, Cole BJ, et al. (2008) Analysis of interobserver and intraobserver variability in the diagnosis and treatment of SLAP tears using the Snyder classification. Am J Sports Med 36(7): 1373-1379.
- Aydin N, Sirin E, Arya A (2014) Superior labrum anterior to posterior lesions of the shoulder: Diagnosis and arthroscopic management. World J Orthop 5(3): 344-350.
- kiven wilk, Macrina LC, Cain EL, Dugas JR, Andrews JR (2013) The recognition and treatment of superior labral (slap) lesions in the overhead athlete. Int J Sports Phys Ther 8(5): 579-600.
- Gorantla K, Gill C, Wright RW (2010) The Outcome of Type II SLAP Repair: A Systematic Review. Arthroscopy 26(4): 537-545.
- Kim SH, Ha KI, Kim SH, Choi HJ (2002) Results of arthroscopic treatment of superior labral lesions. J Bone Joint Surg Am 84(6): 981-985.
- Ide J, Maeda S, Takagi K (2005) Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med 33(4): 507-514.
- Friel NA, Karas V, Slabaugh MA, Cole BJ (2010) Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg 19(6): 859-867.
- Rachel M Frank, Shane J Nho, Kevin C McGill, Robert C Grumet, Brian J Cole, et al. (2013) Retrospective Analysis of Arthroscopic Superior Labrum Anterior to Posterior Repair: prognostic factors associated with failure. Adv Orthop 2013: 125960.
- Reinold MM, Wilk KE, Hooks TR, Dugas JR, Andrews JR (2003) Thermal-assisted capsular shrinkage of the glenohumeral joint in overhead athletes: a 15- to 47-month follow-up. J Orthop Sports Phys Ther 33(8): 455-467.
- Neri BR, El Attrache NS, Owsley KC, Mohr K, Yocum LA (2011) Outcome of Type II Superior Labral Anterior Posterior Repairs in Elite Overhead Athletes Am J Sports Med 39(1): 114-120.
- Denard PJ, Ladermann Alexandre, Burkhart SS (2012) Long-Term Outcome after Arthroscopic Repair of Type II SLAP Lesions: Results According to Age and Workers' Compensation Status: Arthroscopy 28(4): 451-457.
- Neri BR, Emily A, Kvitne RS (2009) Isolated Type II Superior Labral Anterior Posterior Lesions: Age-Related Outcome of Arthroscopic Fixation. Am J Sports Med 37(5): 937-942.
- Alpert JM, Wuerz TH, O'Donnell TF, Caroll KM, Brucker NN, et al (2010) The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med 38(11): 2299-2303.
- Boileau P, Parratte S, Chuinard C, Roussanne Y, Shia D, et al. (2009) Arthroscopic Treatment of Isolated Type II SLAP Lesions: Biceps Tenodesis as an Alternative to Reinsertion Am J Sports Med 37(5): 929-936.
- Baldini T, Snyder L, Peacher G, Bach J, McCarty E (2009) Strength of Single- Versus Double-Anchor Repair of Type II SLAP Lesions: A Cadaveric Study. Arthroscopy 25(11): 1257-1260.
- Domb BG, Ehteshami JR, Shindle MK, Gulotta L, Zoghi Moghadam, et al. (2007) Biomechanical comparison of 3 suture anchor configurations for repair of type II SLAP lesions. Arthroscopy 23(2): 135-140.
- Coleman SH, Cohen DB, Drakos MC, Allen AA, Williams RJ, et al (2007) Arthroscopic repair of type II superior labral anterior posterior lesions with and without acromioplasty: A clinical analysis of 50 patients. Am J Sports Med 35(5): 749-753.
- Enad JG, Kurtz CA (2007) Isolated and combined Type II SLAP repairs in a military population. Knee Surg Sports Traumatol Arthrosc 15(11): 1382-1389.






























