Metal Hypersensitivity after a Total Knee Arthroplasty: A Case Report
Svetlana A Zemlyanskaya1, Ronald S LaButti2, Keivan A Abtahi2 and Aric J Warren1*
1Department of Athletic Training, Oklahoma State University Center for Health Sciences, USA
2Department of Orthopedic Surgery, Oklahoma State University Medical Center, USA
Submission: June 02, 2017; Published: June 19, 2017
*Corresponding author: Aric Warren, Associate Professor, Department of Athletic Training, Oklahoma State University Center for Health Sciences, 1111 W. 17th St, Tulsa, OK, 74107, USA, Email: aric.warren@okstate.edu
How to cite this article: Zemlyanskaya SA, LaButti RS, Abtahi KA, Warren AJ. Metal Hypersensitivity after a Total Knee Arthroplasty: A Case Report. Ortho & Rheum Open Access 2017;7(3): 555714. DOI: 10.19080/OROAJ.2017.07.555714
Abstract
The case presented is of a 65 year old male who presented with pain, swelling, and erythema in left knee 8 months status post total knee arthroplasty by another surgeon. Radiographs demonstrated a mildly oversized femoral component and an asymmetric patella. Periprosthetic joint infection workup was negative. On subsequent visits, pain was out of proportion to what would be expected for oversized or malpositioned components. Patient had no documented history of metal allergy however, testing was performed. Patient was found to be reactive to nickel, which is a common alloy, used in most total knee arthroplasty implants. Patient was then scheduled for revision to a nickel free, Oxinium (Smith & Nephew) total knee arthroplasty implant.
Keywords: Metal hypersensitivity; Total knee arthroplasty; Revision surgery
Introduction
According to the Nationwide Inpatient Sample (NIS) survey, there were 619,000 knee arthroplasties performed in 2009 in the U.S. alone with the numbers likely to double by 2020. The increased demand for total knee arthroplasty (TKA) has also led to an increased overall revision rate. Interest has been placed in determining what leads to TKA failures and what we can do as surgeons to increase the longevity of the index arthroplasty procedure [1]. Many factors have been investigated to determine what lead to negative results after primary total knee arthroplasty. Female gender, greater preoperative pain, and psychological factors such as depression and anxiety have been considered as possible factors related to poor outcomes [2]. Metal hypersensitivities, such as chromium, cobalt, and nickel can cause implant failure [3], however, there is limited data on this [4]. Thus the role of allergies in total knee failures remains a controversial issue. In this paper we present the outcomes of a unique case of a patient experiencing unexplained pain and effusion status post TKA, requiring a revision procedure resulting from hypersensitivity to nickel.
Case Report
65 year old male patient presented status post total knee arthroplasty eight months prior by another surgeon. On initial visit, he complained of severe, diffuse left knee pain. Patient's pain was described as constant. The patient complained of painful crepitus with associated edema. There was no pain free interval after the initial surgery. Patient denied any history of wound complications, fevers, or chills.
Upon physical examination, it was noted that the patient had a large joint effusion on the left knee and was slightly warm to touch when compared to contralateral knee. The incision site had healed with a supple scar and good cosmesis. Focal tenderness to palpation was noted over medial and lateral femoral condyle. Range of motion was 0-105 degrees measured with a goniometer. The patient had well balanced ligaments throughout arc of motion with appropriate patella tracking and no subsequent subluxation or dislocation. Longstanding lower extremity radiographic evaluation showed 1.3 degree valgus mechanical axis with 91.5 degree medial femoral articular angle and a 90 degree medial tibial articular angle. Radiographs including AP/ Lateral/merchant views showed overhang of lateral aspect of femoral component. Tibial component was well sized. The joint line and patella height appeared within normal limits.
The initial plan was to perform a basic infectious workup with erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Knee arthrocentesis was performed and sent for synovial fluid cell count with differential, gram stain, culture and sensitivities, crystal analysis, alpha defensin, synovial CRP and human neutrophil elastase testing. Results revealed an ESR of 60 (normal range 0-22), and a CRP of 1.03 (<.8 normal). Cell count with differential was 606 white blood cell counts with 15% segmented neutrophils which decreased the likelihood of prosthetic joint infection. Crystal analysis was negative and final cultures showed no growth. Synovial CRP, alpha defensin and human neutrophil elastase testing were negative or within normal limits. The patient returned three weeks later with knee pain out of proportion to what would be expected for oversized or malpositioned components. ESR and CRP were again repeated with similar results. A metal allergy serum assay was ordered to rule out metal hypersensitivity. One month later, the results of the metal allergy testing did show reactivity to nickel. The patient elected to proceed with TKA revision with oxidized zirconium (Oxinium, Smith & Nephew) hypoallergenic components. (Figures 1-4) Postoperative lower extremity radiographs.

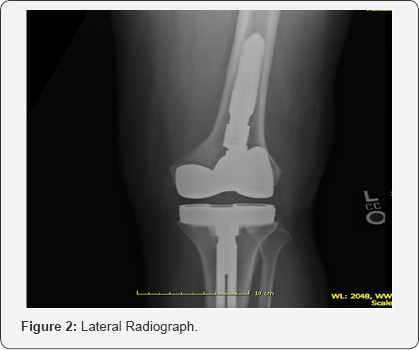


On subsequent postoperative visits, patient progressed well and was ambulating with a cane by 8 weeks. His pain was overall improved and he had an arc of motion of had 0-110 degrees of flexion. The knee was stable to varus and valgus stress. At 20 weeks postoperative, the patient continued to progress well. Passive range of motion was 0-110 degrees and full strength in quadriceps and hamstring was noted. Radiographs showed overall well sized and well positioned components.
Discussion
Metal sensitivity among the general population is approximately 10-15%. Sensitivity to nickel is present in about 20.4% of females and 5.8% of males [3]. Therefore, routine allergy testing is not recommended unless the patient has a strong medical history of metal sensitivity [5]. Some studies show that patients may even tolerate implants containing metals to which they are allergic [6]. Others argue that metal allergy should be taken into consideration prior to implantation because it is a potential risk factor for total knee arthroplasty failure or poor outcomes [7]. Patch testing is currently the gold standard for in vivo assessment, but is still controversial because it does not include the whole variety of antigens relevant for hypersensitivity in orthopaedic surgery. Therefore, these cases have to be reviewed on an individual case by case basis.
Part of the issue may be the unobservable local effects of metal hypersensitivity on the implant bone interface. Polymeric debris activates the innate or nonspecific immune system. The local effect of metal debris is not completely understood, but some generalizations have been made. The inflammatory response is proportional to the particulate load, metal particles are more proinflammatory than polymer-debris, and wear particle generation causes osteoclastic activation via macrophage ingestion. Some individuals are more at risk of aseptic loosening due to a heightened response to particulate and non-particulate debris [8]. This case demonstrates the unique situation of subacute postoperative pain and stiffness after TKA due to metal hypersensitivity. It further demonstrates that ceramic implants are a favorable solution for patients suffering from hypersensitivity to metal ions in total knee arthroplasty. This is a diagnosis of exclusion but may be considered when infection, osteolysis or poorly sized or malpositioned implants have been ruled out.
References
- Bravo D, Wagner ER, Larson DR, Davis MP, Pagano MW (2016) No increased risk of knee arthroplasty failure in patients with positive patch testing for metal hypersensitivity: A matched cohort study. J Arthroplasty 31(8): 1717-1721.
- Hinarejos P, Ferrer T, Torres-Claramunt R, Sanchez-Soler J, Monllau C (2016) Patient-reported allergies cause inferior outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrose 24(10): 32423246.
- Bergschmidt P, Bader R, Mittelmeier W (2012) Metal hypersensitivity in total knee arthroplasty: Revision surgery using a ceramic femoral component- A case report. Knee J 19(2): 144-147.
- Middleton S, Toms A (2016) Specialty update: knee allergy in total knee arthroplasty a review of the facts. Bone Joint J 98-B(4): 437-441.
- Faschingbauer M, Renner L, Boettner F (2017) Allergy in total knee replacement. Does it exist? HSS J 13(1): 12-19.
- Dietrich KA, Mazoochian F, Summer B, Reinert M, Ruzicka T, et al. (2009) Intolerance reactions to knee arthroplasty in patients with nickel/cobalt allergy and disappearance of symptoms after revision surgery with titanium-based endoprostheses. J Dtsch Dermatol Ges 7(5): 410-413.
- Granchi D, Cenni E, Tigani D, Trisolino G Baldini N, et al. (2008) Sensitivity to implant materials in patients with total knee arthroplasties. Biomaterials 29(10): 1494-1500.
- Lohmann CH, Hamester R, Singh G (2017) Allergies in orthopaedic and trauma surgery. Orthop Traumatol Surg Res 103(1): S75-S81.






























