Do New knee Implant Designs Accelerate Early Motion and Function in Total knee Arthroplasty (TKA) Patients?
*Terri A Zachos and Wes Mesko
Department of Surgery, University Hospitals Cleveland Medical Center, USA
Submission: March 24, 2017; Published: April 06, 2017
*Corresponding author: Terri A (Tiffy) Zachos, MD, PhD, DVM, Resident Physician, PGY-1, Department of Surgery, University Hospitals Cleveland Medical Center, 11100 Euclid Avenue, Cleveland, OH 44106, USA, Tel: (517) 927-8865; Email: Terri.Zachos@UHhospitals.org
How to cite this article: Terri A Z, Wes M. Cunningham. Do New knee Implant Designs Accelerate Early Motion and Function in Total knee Arthroplasty (TKA) Patients?. Ortho & Rheum Open Access 2017; 5(5): 555675. DOI: 10.19080/OROAJ.2017.05.555675
Abstract
Background: Modification total knee implant designs bring hope of more rapid recovery with improved patient satisfaction and longevity. However, these proposed improvements also increase implant costs. The purpose of this study was to determine whether newer designs with greater size options of the femur and tibia result in improved short term clinical results.
Methods: Sixty DePuy Attune and 49 Zimmer Persona knees were compared to 33 DePuy Sigma and 49 Stryker Triathlon knees. All knees were done by a single high volume total joint fellowship trained surgeon. Patients were prospectively entered into a database. Variables recorded include: age, sex, weight, height, date of surgery, laterality of the operative knee joint, pre-operative and post-operative body mass index, preoperative and post-operative knee range of motion, pre- and post-operative Knee Society Scores (KSS), and lower extremity activity scale (LEAS) scores. Clinical parameters were recorded at six weeks and six months post-operatively. Data were retrospectively reviewed and statistical analyses were performed.
Results: There were no significant differences among groups when comparing: change in flexion from pre-operative values at six weeks and six months post-operatively, change in total flexion arc at six weeks and six months post-operatively, and change in KSS at six months postoperatively (p> 0.05 for all). There were no significant differences in six-month LEAS (p> 0.05) among groups.
Conclusion: This pilot study suggests higher priced, newer total knee designs give neither a speedier recovery nor improved patient function in the first six months, compared to commonly used designs when identical surgical paradigms are used.
Keywords: Total knee Arthroplasty; Outcome; Implant Design
Abbreviation: KSS: Knee Society Scores; LEAS: lower extremity activity scale; TKA: Total knee arthroplasty; ANOVA: Analysis of variance; DVT: Deep vein thrombosis; ASA: Aspirin.
Introduction
Although total knee arthroplasty (TKA) has dramatically improved the lives of many patients with disabling knee arthritis, patients rarely view it as a normal knee in terms of pain relief and function. The desire to achieve more normal feel and function is heightened as greater numbers of youthful, active patients have reached the end of non-operative options for their knee arthritis and choose surgery. The elements that lead to a "high performance total knee replacement" are multi-factorial but are thought to include design modifications that most effectively replicate host anatomy [1]. This study was a pilot to test if newer designs with greater size options of the femur and tibia result in improved short term clinical results when other variables of modern knee replacement were constant.
Material and Methods
After local institutional IRB approval, a retrospective search was conducted of the senior author's registry. This registry includes prospectively collected data routinely gathered on all total joints implanted over the preceding 24 years. A power analysis was performed, based on Knee Society Score (KSS) as an endpoint, analysis of variance (ANOVA) as the test, 80% power to detect a difference of >5 in KSS (with standard deviation of 25, consistent with a medium effect size), and 0.05 level of significance [2]. Power analysis determined adequate numbers of patients to answer the question of significance for the parameters selected to evaluate.
Demographic data, surgical event details including implants and hospital course, Knee Society Scores, and complications are included over time. All the knees included were metal backed tibia, fixed bearing, and posterior cruciate retaining. Sixty DePuy Attune and 49 Zimmer Persona knees were compared to 33 DePuy Sigma and 49 Stryker Triathlon knees. All knees were done by a single high volume total joint fellowship trained surgeon via a less invasive midvastus approach with patellar lateralization. Custom cutting jigs to accommodate this approach were used via an intramedullary referencing approach on the femur and extramedullary referencing on the tibiain all knees. All patellae were resurfaced. Regarding patellar implants: in the case of the Attune, all were oval; the Persona, all were round; and for the Sigma and Triathlon a mixture of round and oval implants were used. The specific manufacturer-designed femoral sizing and chamfer cutting jigsas well as proximal tibial spine cutting guide and drills or punches were used to finish the preparation. A measured resection technique was implemented using a posterior tibial slope of 3 degrees in the Sigma and Triathlon, 4-6 degrees with the Attune and 7 degrees with the Persona. Effort was made to secure enough numbers of cases in each group to have sufficient statistical power to make a meaningful conclusion in terms of difference in the parameters evaluated. As this was considered a pilot study, cases were gathered in the sequence in which they were implanted. All patients were evaluated pre- operatively and at six weeks and six months post-operatively.
All patients were admitted the day of surgery. Although regional anesthesia was encouraged, the decision was ultimately left to the anesthesiologist and the patient. All patients had their soft tissues infiltrated with a cocktail of ropivicaine, ketorolac (Toradol), morphine and epinephrine. Elements of these were deleted if renal compromise or allergies were present. Following surgery, a drain was placed in all knees and patients were encouraged to ambulate about the room the same day, weight- bear as tolerated with an assist device and were instructed on range of motion exercises. On postop day one multiple disciplines educated the patient on the care of their surgery site, ADL, a home exercise program, and a pain management strategy. Patients were released when they demonstrated proficiency in all areas of their training. For those who went home, an outpatient regimen of 8 sessions of physical therapy was given with the emphasis that the patient was in charge of their outcome and the therapist was to be the coach, to guide improvement, adding or modifying the exercise regimen to optimize outcome, and were a set of eyes in the event of delayed recovery.
All patients were seen if they were not progressing as expected after the eight therapy sessions to judge if an alternative treatment plan was necessary. Patients were encouraged to wean off of assist devises when they could walk without a limp and had stable balance. Deep vein thrombosis (DVT) prophylaxis revolved around time-efficient surgery with minimal tourniquet time, rapid mobilization, TED stockings during the day for two weeks, and aspirin (ASA) 81-325 mg daily for those with no personal or family history of DVT. Those who had such a history were offered warfarin (Coumadin), for a month, injectable LMWH for 2-3 weeks followed by aspirin, or rivaroxaban (Xarelto). Few people chose Xarelto because of nonpayment by insurance carriers in this region.
Results

*G: General, S: Spinal, S/G: Spinal/General.
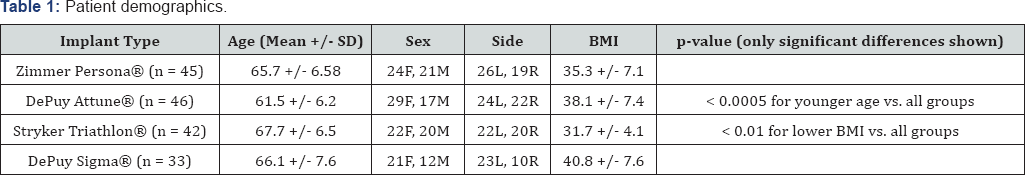
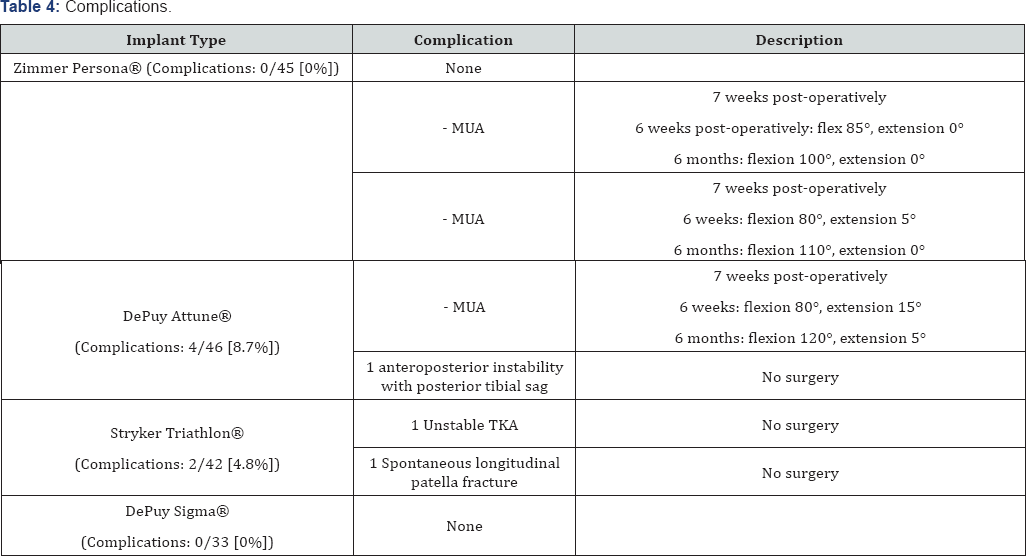
This pilot study focused on speed of recovery in the first 6 months as measured by Knee Society Scores (KSS) with a specific focus on flexion and extension and the change in arc of motion. The six-month Lower Extremity Activity Score (LEAS) was considered without a baseline as to pre-operative LEAS. Patient demographics are shown in (Table 1). Hospitalization, operative and perioperative data are shown in (Table 2). There were no significant differences among groups when comparing the following parameters: change in flexion from pre-operative values at six weeks and six months post-operatively, change in the total flexion arc at six weeks and six months post-operatively, and change in KSS at six months post-operatively (p> 0.05 for all).When considering demographics of all 4 groups there was no significant difference between the BMI's of patients in the DePuy Attune and DePuy Sigma groups (p> 0.05). There was no significant difference between the BMI's of patients in the Zimmer Persona and DePuy Attune groups (p> 0.05). The Attune and Sigma knees were implanted in those that were statistically heavier than the patients receiving the Persona and Triathlon knees (p<0.05). More specifically, mean BMI’s of patients in the Zimmer Persona group were significantly higher than those in the Stryker Triathlon group (p< 0.05). Mean BMI's of patients in the DePuy Sigma group were significantly higher than those in the Zimmer Persona group (p< 0.01). Mean BMI’s of patients in the DePuy Attune (p< 0.05) and DePuy Sigma (p< 0.05) groups were significantly higher than those in the Stryker Triathlon group. The Attune Knees were also statistically younger than the other cohorts (p< 0.05). Despite the differences in youth and weight, there did not appear to be a statistically significant difference in six-month LEAS (p> 0.05). Complications noted were, one lax knee with posterior tibial sag, one unstable TKA, one spontaneous patellar fracture, and three patients with arthrofibrosis needing a manipulation under anesthesia six weeks post-op. All three achieved a flexion of >100 degrees following manipulation under anesthesia. None of these complications required operative intervention.
Discussion
The goal to achieve a rapid recovery in a high functioning TKA includes several key variables. The surgical approach and invasiveness of that approach is considered important. Initial reports reported faster recovery times with techniques that were "quad sparing" and avoiding eversion of the patella. The importance of these elements has been called into question [3,4]. Instrumentation and the technique of surgery including precision reusable instruments, navigation and custom cutting blocks have potential to lessen soft tissue dissection and give more accurately aligned bone cuts based on the paradigms of those technologies [5]. Multimodal pain management algorithms, coupled with rapid mobilization demonstrate quicker return to function [6]. Finally, securing an implant design that best replicates the normal knee in kinematics and sizing options gives hope for quicker recovery and a more normal functioning knee, which is the objective of the newer implants.
This project was a pilot to determine if adding greater options in sizing would improve hospital length of stay or measurable recovery parameters more favorably than older designs. Newly introduced implants nearly always come with an increased price to the hospital and payers. Although it is intuitive that implants that more exactly replicate patient anatomy should allow quick recovery in terms of motion and function, this theory is untested in a clinical setting. This study supports neither more rapid return to function nor improved function in the first six months from surgery in the newer knee designs versus with more commonly used designs. Although greater manipulation under anesthesia was needed in the Attune cohort, the numbers were too small to make this statistically significant when compared to the other groups (Tables 3 & 4).

There are several strengths of this pilot study. First, all surgeries were done by a single high volume knee replacement surgeon using the same IM femoral cutting jig and EM tibial cutting jig, using the same measured resection technique. In addition, none of the patients were aware of which implant they were receiving, nor did any of them inquire about this. Regarding their expectations, these patients only expressed their general desire for a good outcome. Finally, no mention was made to patients that newer implant designs were being used, nor were any comments made implying that newer implants were superior in any way [7-25].
Conclusion
The major weaknesses of this study were lack of randomization or blinding regarding implants used by the investigator. In particular, the physician making measurements of ROM was not blinded with regard to implant used. Additionally, the Persona and Attune cases came from the early experience of the surgeon with these implants and the Triathlon and Sigma were cases done much deeper into his experience curve. A prospective, randomized multicenter study is needed to corroborate or refute the findings of this study. Additional longterm studies are needed in order to demonstrate that the newer implants are more durable and allow the recipient to ultimately return to higher levels of function than earlier designs. In the meantime, this pilot study suggests that the higher priced, newer TKA designs give neither a speedier recovery nor improved patient function in the first 6 months, compared to commonly used designs when identical surgical paradigms are used.
Financial Disclosure
The authors have no disclosures and report no conflicts of interest.
References
- Ilavov K, Cohn R, Slover J (2013) High-performance total knee replacement. Bull Hosp Jt Dis 71(1): 79-88.
- Cohen J (1992) A power primer. Psychol Bull 112(1): 155-159.
- Bonutti P, Zywiel M, Ulrich S, Stroh D, Seyler T, et al. (2010) A comparison of subvastus and midvastus approaches in minimally invasive total knee arthroplasty. J Bone Jt Surg Am 92(3): 575-582.
- Nestor B, Toulson C, Backus S, Lyman S, Foote K, et al. (2010) Mini- midvastus vs standard medial par patellar approach: a prospective, randomized, double-blinded study in patients undergoing bilateral total knee arthroplasty. J Arthroplast 25(6): 5-11.
- Cheng T, Pan X, Mao X, Zhang G, Zhang X (2012) Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. 19(4): 237245.
- Maheshwari A, Blum Y, Shekhar L, Ranawat A, Ranawat C (2009) Multimodal pain management after total hip and knee arthroplasty at the Ranawat Orthopaedic Center. Clin Orthop Rel Res 467(6): 14181423.
- Yang CC, Kim RH, Davenport PG (2015) Population-Based Evaluation of Patellar Component Design on Size , Coverage and Median Ridge Position. In: Orthopaedic Research Society Abstracts. Las Vegas, Nevada 2015: 7-10.
- Helmy N, Anglin C, Greidanus NV, Masri BA (2008) To resurface or not to resurface the patella in total knee arthroplasty. Clin Orthop Relat Res 466(11): 2775-2783.
- Dennis DA, Kim RH, Johnson DR, Springer BD, Fehring TK, et al. (2011) The john insall award: Control-matched evaluation of painful patellar crepitus after total knee arthroplasty. Clin Orthop Relat Res 469(1): 10-17.
- Conrad DN, Dennis DA (2014) Patellofemoral crepitus after total knee arthroplasty: Etiology and preventive measures. Clin Orthop Surg 6(1): 9-19.
- New Y, Health H, Corporation S (2015) Patient-Reported Outcomes Following Elective Primary Total Hip and/or Total Knee Arthroplasty : Hospital Level Performance Measure (S) Phase 3 Measure Methodology Report, USA.
- Rissanen P, Aro S, Slatis P, Sintonen H, Paavolainen P (1995) Health and quality of life before and after hip or knee arthroplasty. J Arthroplast 10(2): 169-175.
- Ritter M, Albohm M, Keating E, Faris P, Meding J (1995) Comparative outcomes of total joint arthroplasty. J Arthroplast 10(6): 737-741.
- Insall J, Dorr L, Scott R, Scott W (1989) Rationale of the knee society clinical rating system. Clin Orthop Rel Res 248: 13-14.
- The 2011 Knee Society Scoring System: Licensed User Manual (2012) The Knee Society, Rosemont, USA pp. 9.
- Scuderi G, Bourne K, Noble P, Benjamin J, Lonner J, et al. (2012) The new Knee Society Knee Scoring System. Clin Orthop Rel Res 470(1): 3-19.
- Cherian JJ, O Connor MI, Robinson K, Jauregui JJ, Adleberg J, et al. (2015) A Prospective, Longitudinal Study of Outcomes Following Total Knee Arthroplasty Stratified by Gender. J Arthroplast 30(8): 1372-1377.
- Saleh KJ, Mulhall KJ, Bershadsky B, Ghomrawi HM, White LE, et al. (2005) Development and validation of a lower-extremity activity scale. Use for patients treated with revision total knee arthroplasty. J Bone Joint Surg Am 87(9): 1985-1994.
- Noble P, Scuderi G, Brekke A, Sikorskii A, Benjamin JB, et al. (2012) Development of a new knee society scoring system. Clin Orthop Rel Res 470(1): 20-32.
- Dowsey M, Choong FM (2013) The utility of outcome measures in total knee replacement surgery. Int J Rheumatol 2013(1): 506518.
- Choong PF, Dowsey MM, Stoney JD (2009) Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty 24(4): 560-569.
- Ritter MA, Davis KE, Davis P, Farris A, Malinzak, et al. (2013) Preoperative malalignment increases risk of failure after total knee arthroplasty. J Bone Joint Surg Am 95(2): 126-131.
- Zahiri C, Schmalzried T, Szuszczewicz E, Amstutz H (1998) Assessing activity in joint replacement patients. J Arthroplast 13(8): 890-895.
- Weiss J, Noble P, Conditt MA, Kohl HW, Robert S, et al. (2002) What functional activities are important to patients with knee replacements? Clin Orthop Rel Res (404):172-188.
- Healy W, Iorio R, Lemos M (2000) Athletic activity after total knee replacement. Clin Orthop Rel Res (380): 65-71.






























