Comparison of Open Wedge High Tibial Osteotomy versus Unicondylar Knee Replacement for Medial Knee Osteoarthritis
*Walaa El-Din Ahmed El-Nahas, Baseem Choudhry, Mohamad A Imam and Bahaa Kornah
Kings Mill Hospital, Mansfield Road, England
Submission: February 11, 2017; Published: February 23, 2017
*Corresponding author: Kings Mill Hospital, Mansfield Road, Sutton-In-Ashfield, NG17 4JL, Royal Derby Hospital, New Uttoxeter Road, Derby, DE22 3NE, England
How to cite this article: Walaa E-D A E-N, Baseem C, Mohamad A I, Bahaa K. Comparison of Open Wedge High Tibial Osteotomy versus Unicondylar Knee Replacement for Medial Knee Osteoarthritis. Ortho & Rheum Open Access 2017; 5(1): 555651. DOI: 10.19080/OROAJ.2017.05.555651
Abstract
Introduction: Medial knee osteoarthritis is a source of debilitating pain. Varus malalignment is associated with a 4-fold increase in unicompartmental osteoarthritis. Current non-surgical treatments include patient education, weight loss, analgesics. Two contemporary surgical treatment options for medial knee osteoarthritis are available and each procedure has its merits. These are based on different principles: high tibial osteotomy (OW- HTO) where correction of knee angular deformity with slight valgus overcorrection is the goal and unicondylar knee replacement (UKA) surgery’s aim in replacing damaged articular surface.
Aim: To review clinical outcomes of two matched populations between open wedge high tibial osteotomy (OW-HTO) and unicondylar knee (UKA).
Material and Methods: This was a prospective study of two matched populations at two different centres, employing different techniques for managing medial knee compartment osteoarthritis. The OW-HTO centre had recruited 19 patients over February 2012 to December 2013. The TomoFix® knee osteotomy. The unicondylar knee replacement (UKA) centre had 22 patients over June 2012 to August 2013 and used the Oxford™ partial knee system in these operations.
Conclusion: In conclusion, this study shows that open wedge high tibial osteotomy and unicondylar knee replacements have no significant differences in oxford scores at 6 weeks and 6 months.
Keywords:Open Wedge High Tibial Osteotomy; Unicondylar Knee Replacement; Medial Knee Osteoarthritis; Unicompartmental Osteoarthritis
Abbreviations:UKA: Medial Unicompartmental Knee Arthroplasty; HTO: High Tibial Valgus Osteotomy; BMI: Body Mass Index; AP Instability: Antero-Posterior Instability; ML Instability: Medio-Lateral Instability; Instability Grading: According to the American Medical Association (grade I = 0-5 mm, grade II = 5-10 mm, grade III = >10 mm, no hard stop); Arthrosis severity: Medial Compartment Arthrosis According To Ahlback Classification; Assuming That Lateral And Patellofemoral Compartments are Intact.
Introduction
Medial knee osteoarthritis is a source of debilitating pain. Varus malalignment is associated with a 4-fold increase in unicompartmental osteoarthritis independent of BMI, age and sex [1]. Current non-surgical treatments include patient education, weight loss, analgesics, physical therapy and bracing.
Once these conservative options fail or are exhausted, and symptoms persevere then surgical treatments are deliberated.
Two contemporary surgical treatment options for medial knee osteoarthritis are available and each procedure has its merits. These are based on different principles: high tibial osteotomy (OW- HTO) where correction of knee angular deformity with slight valgus overcorrection is the goal and unicondylar knee replacement (UKA) surgery’s aim in replacing damaged articular surface.
Indications of Unicondylar Knee Replacement
UKA is suitable for patients with moderate joint osteoarthritis, traumatic injury, a history of unsuccessful surgical procedures or poor bone density that precludes other types of knee surgery. Patients not eligible for arthroplasty are those with an active or suspected infection in or about the knee joint, have a known sensitivity to device materials, have borne infections or disease that result in an inability to support or fix the new implant to the bone, have inflammatory arthritis, have major deformities that can affect the knee mechanical axis, have neuromuscular disorders that may compromise motor control and/or stability, have any mental neuromuscular disorder, patients who are not skeletally mature, are obese, have lost a severe amount of bone from the shin (tibia) or have severe tibial deformities, have recurring subluxation of the knee joint, have untreated damage to patellofemoral joint, have untreated damage to the opposite compartment or the same side of the knee not being replaced by a device, and/or have instability of the knee ligaments such that the postoperative stability the UKA would be compromised. The anterior cruciate ligament (ACL) should be intact.
Indications of High Tibial Osteotomy
The indications for an osteotomy are malalignment with arthrosis, and/or instability, with or without an articular cartilage procedure. Patients with secondary degenerative arthritis, a varus knee, and localised medial joint pain are also candidates for an osteotomy. Total joint replacement outcomes in the young adult have been less reliable and more complex.
Contraindications for high tibial osteotomy (HTO) are smokers due to high risk of non-union. HTO should be avoided in knees that demonstrate larger areas (15 × 15 mm) of exposed bone on both the tibial and femoral surfaces. Relative contraindications include body weight greater than 90 kg, severe patellofemoral symptoms, or patients with abnormal patella infera or alta since an osteotomy may increase the forces on articular cartilage in these patients.
A well written review by [2] summarises indications for unicondylar knee replacement and high tibial osteotomy well as presented in table below (Table 1).

Aim
To review clinical outcomes of two matched populations between open wedge high tibial osteotomy (OW-HTO) and unicondylar knee (UKA).
Material and Methods
This was a prospective study of two matched populations at two different centres, employing different techniques for managing medial knee compartment osteoarthritis. These patients were matched in age, gender, body mass index (BMI), and failure of conservative treatments. Both of these populations were pre-operatively assessed and where warranted anaesthetic review was performed as part of enhanced recovery.
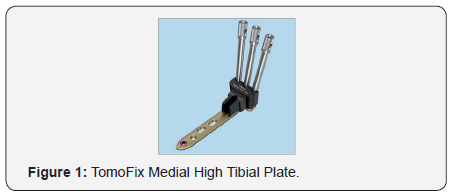
The patients in OW-HTO group had standard long leg films as part of their preoperative planning where as UKA group had standard AP, lateral and sky line radiographs. The two centres are acute service hospitals at two different geographical locations that are experienced in these techniques, and were blinded respectively to other centre results. The OW-HTO centre had recruited 19 patients over February 2012 to December 2013. The TomoFix® knee osteotomy system using its locking medial high tibial plate (Synthes Inc., Bettlach, Switzerland) during the procedure (Figures 1 & 2).

The unicondylar knee replacement (UKA) centre had 22 patients over June 2012 to August 2013 and used the Oxford™ partial knee system in these operations. Majority of patients had spinal anaesthesia with femoral nerve block and received 3 doses of Cefuroxime. First at induction and then the other two at 8 hourly intervals. All patients had tourniquet inflated to 300mgHg and were catheterised and then removed the following morning. All patients received patient controlled analgesia, which was removed when patients’ pain became manageable. Patients were discharged when patients were medically fit, able to mobilise safely with crutches, climb stairs as well as flex knee to 90 degrees.
Both groups of patients were given venous thromboembolism prophylaxis (Tinzaparin) for 28 days and provided with advice for immediate complications. These patients were followed up to 6 months in outpatient clinics and were clinically reviewed for short term complications, and also given oxford knee score questionnaires. Oxford knee score is a 12 item questionnaire over 3 domains. These are corresponding to pain, function and instability. Each question has 5 choices for answer rated from 1 to 5. Hence the score is given out of 60. 12 is the best outcome whereas 60 is the worst outcome possible.
Surgical technique for medial opening wedge tibial osteotomy
The surgery is done with the patient in the supine position using a tourniquet. Fluoroscopic imaging is used throughout the surgery. After the patient has received preoperative antibiotics, the surgical preparation is performed. An incision is made halfway between the tibial tubercle and the posteromedial border of the tibia. Dissection is then carried down to the sartorius fascia. The fascia is incised in line with the fibres of the pes anserinus tendons, which are then retracted medially, exposing the superficial medial collateral ligament. A periosteal elevator is used to retract the MCL medially, exposing the underlying tibial cortex. The patellar tendon is retracted laterally. The most superior fibres of the patellar tendon may be released to improve visualisation of the osteotomy site.
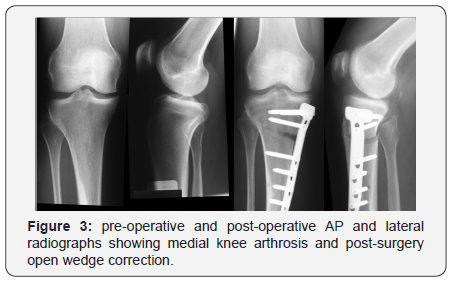
A guide pin is placed under fluoroscopic guidance starting 4 cm distal to the medial tibial plateau and angling 1 cm below the lateral tibial plateau. Orientation of this pin is marked to determine the angle of the osteotomy. An oscillating saw is placed below and parallel to the guide pin to begin the osteotomy, taking care to only cut the medial and posteromedial cortex. Thin osteotomes are used to complete the osteotomy ending approximately 1 cm short of the lateral femoral cortex to maintain a lateral hinge. Larger osteotomes are then used to slowly open the osteotomy site. A calibrated osteotome is then used to open the osteotomy to the desired correction, and then either locking or non-locking plate can be used according to the surgeon’s preference (Figure 3).
Surgical technique of UKA
With knee flexed to 90 degrees the joint was opened via an anteromedial arthrotomy starting at the medial border of the patella and ending 3 cm below the tibia plateau. The incision is deepened through to enter joint capsule and at proximal end the incision is extended 1-2cm into the vastus medialis. Part of Hoffa’s pad is excised to allow anterior tibia exposed. ACL is inspected to ensure the UKA prosthesis is suitable, otherwise TKA was decided. The osteophytes were resected and the tibial resection was performed with an oscillating saw under the guidance of a jig which is positioned according to the physiological tibial slope. The medial collateral ligament was protected with a Hohmann retractor. The vertical cut was performed first; then the horizontal cut is performed. The size of the resected plateau allowed space for a tibial component and a meniscus implant of at least 4 mm. The resected plateau serves to determine the size of the plateau.
With knee flexed at 45 degrees, hole is made into intramedullary canal of femur with 5mm awl. This is situated 1cm anterior to anteromedial corner of intercondylar notch. Insert the intramedullary rod until rod pusher is stopped against the bone. Using femoral drill guide, 4mm drill bit is drilled into upper hole into bone up to stop and left in place. Once alignments are confirmed a 6mm drill is then drilled through lower hole in the guide. Once done all instrumentation from the distal femur is removed and femoral saw block is inserted into the drilled holes. At this point any remnants of medial meniscus and osteophytes from corner of condyle are removed. 0 mm spigot was inserted into the central drill hole and the distal part of the condyle is milled. The depth of milling was determined by equalizing flexion and extension gap.
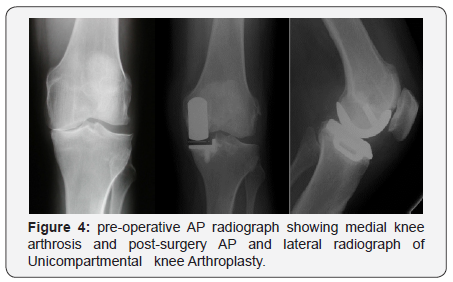
Extension and flexion gap balancing was controlled with test inlays. Posterior osteophytes and anterior aspect bone resection was needed to reduce risk of impingement. Then the tibia plateau was finally prepared. Here marginal osteophytes were excised, template is inserted and sizing of component is checked and altered if necessary. After testing implants the femoral and tibial components were cemented one stage after preparation of the bone with a jet lavage (Figure 4).
Results
19 patients were allocated to OW-HTO group and 22 patients were allocated to UKA group. In OW-HTO group 18 patients had done unilaterally and one patient had bilateral open wedge procedures done 1 year apart.
In UKA group, 13 were female and 9 were male and, in OWHTO group 9 were female and 10 male respectively. In OW- HTO group 13 patients were aged between 40-50 years where as 5 patients were in UKA group. 7 patients in OW-HTO group and 8 patients were in UKA group were aged between 50-60 years. The rest were from UKA group, these 9 patients were aged 60- 70 years.
The average length of stay (LoS) for OW-HTO group was 1.6 days compared to 2.8 days for UKA group.
At 6 week follow up 2/22 patients with UKA had significant effusion versus one patient with open wedge high tibial osteotomy, 2/22 patients with UKA compared to 4/20 OW-HTO patients had significant tenderness. 2 patients complained of stability problems in UKA group. Neither group had significant events noted at 6 months.
The mean oxford scores at 6 weeks was 46 for UKA compared to 44 for OW-HTO. Mean oxford scores at 6 months was 50 for UKA group versus 48 for OW-HTO group respectively.
Discussion
The best treatment for OA in a single compartment of the knee has been the subject of much recent debate. HTO, UKA and TKA are the typical choices of surgical procedures for treating this condition. The purpose of surgery is to reduce pain, restore function and improve quality of life. Both HTO and UKA are less invasive procedures than TKA, both preserve the bone stock, and both subsequently allow for normal kinematics by retaining cruciate ligaments [3].
Both surgeries have shown satisfactory outcomes and survival rates at mid- and long-term follow-up [4] concluded UKA performed better than CW-HTO. They performed a 20 – 40 month retrospective review of 23 knees after HTO and 21 knees after UKA. HTO had 100% survivorship at two years while UKA showed a 91% survival rate at three years. In osteotomy group there were 9% excellent, 39% good, and 52% poor results. In the unicompartmental group, there were 48% excellent, 43% good, and 9% poor results.group.
[5] performed a similar prospective randomized study on 18 HTO and 22 UKA patients. Patients (from 55 to 70 years of age) with medial knee arthritis were randomly assigned, and were examined before surgery, at 3 months, 1 and 5 years after surgery. Closed wedge osteotomy, postoperatively immobilized in a whole-leg plaster cast for six weeks) and the UKA used was Brigham (Depuy).
BOA score, range of motion, and patient satisfaction were not different between the groups. Time-distance variables of gait showed clinically significant differences in favour of the UKA group at three-months after surgery, but these became insignificant at one- and five-year follow-up.
At the 2008 AAOS Annual meeting, Dettoni et al. [2] presented study of 54 patients with medial opening wedge HTO (Puddu plate, Anthrex) to 56 patients treated with Accuris UKA (Smith & Nephew). The Knee Society score and the WOMAC were evaluated at two to four years of follow-up. The two groups were comparable in terms of preoperative assessment and gender, but differed regarding age (mean age 55 years for HTO and 65 for UKA). Both groups obtained satisfactory results: 93% good-to-excellent results in the HTO group and 95% in the UKA group. Although differences were not significant, the UKA group showed a slightly better knee score (93 points compared to 76 in the HTO group), while HTO showed a better function score (91 points compared to 84 from the UKA group) [6-11].
Conclusion and Recommendation
In conclusion, this study shows that open wedge high tibial osteotomy and unicondylar knee replacements have no significant differences in oxford scores at 6 weeks and 6 months. Patients should be informed that with open wedge high tibial osteotomies pain initially is worse but resolve by 6 months.
References
- Sharma L, Song J, Felson DT, Cahue S, Shamiyeh, Dunlop DD (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286(2): 188-195.
- Dettoni F, Bonasia DE, Castoldi F, Bruzzone B, Blonna D, Rossi R (2010) High tibial osteotomy versus unicompartmental knee arthroplasty for medial compartment arthrosis of the knee: a review of the literature. Iowa Orthop J 30: 131-140.
- Petersen W, Metzlaff S (2016) Open wedge high tibial osteotomy (HTO) versus mobile bearing unicondylar medial joint replacement: five years results. Arch Orthop Trauma Surg 136(7): 983-989.
- Karpman RR, Volz RG (1982) Osteotomy versus unicompartmental prosthetic replacement in the treatment of unicompartmental arthritis of the knee. Orthopedics 5(8): 989-991.
- Borjesson M, Weidenhielm L, Mattsson E, Olsson E (2005) Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee 12(2): 121-127.
- Atrey A, Morison Z, Tosounidis T, Tunggal J, Waddell JP (2012) Complications of closing wedge high tibial osteotomies for unicompartmental osteoarthritis of the knee. Bone Joint Res 1: 205- 209.
- Broughton NS, Newman JH, Baily RA (1986) Unicompartmental replacement and high tibial osteotomy for osteoarthritis of the knee. A comparative study after 5-10 years’ follow-up. J Bone Joint Surg Br 68: 447-452.
- Ivarsson I, Gillquist J (1991) Rehabilitation after high tibial osteotomy and unicompartmental arthroplasty. A comparative study. Clin Orthop Relat Res 266: 139-144.
- Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A (2001) High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7-10-year follow-up prospective randomised study. Knee 8(3): 187-194.
- Takeuchi R, Umemoto Y, Aratake M, Bito H, Saito I, et al. (2010) A mid term comparison of open wedge high tibial osteotomy vsunicompartmental knee arthroplasty for medial compartment osteoarthritis of the knee. J Orthop Surg Res 5: 65.
- Weale AE, Newman JH (1994) Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee. A comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res (302): 134-137.






























