Rapid Onset Long Acting Brachial Plexus Blocks in Hand Surgery
*Mohamed Maher, Ahmed Elgawad, Mohamed Saleh, Andrew Logan and Fahmy Fahmy
University Hospital of Birmingham, UK
Submission:October 12, 2016; Published: October 24, 2016
*Corresponding author: Mohamed Maher, University Hospital of Birmingham, 40 Chalgrove Ave Kings Norton Birmingham, B388YP, UK
How to cite this article: Mohamed M, Ahmed E, Mohamed S, Andrew L, Fahmy F. Rapid Onset Long Acting Brachial Plexus Blocks in Hand Surgery.Ortho & Rheum Open Access J. 2016; 3(2): 555610. DOI: 10.19080/OROAJ.2016.03.555610
Abstract
Axillary brachial plexus blocks are a widely used form of anaesthesia for upper limb surgery. This has largely replaced the need for a general anaesthetic. We hereby present our technique, describing a new formula of injection that permits a fast acting block without the need to wait as with the usual local anaesthetics used in most brachial plexus blocks.
Keywords; Brachial Block; Hand Surgery; Regional Anaesthesia
Introduction
The first brachial block was performed in 1884 by RJ Hall [1,2] by injecting cocaine to provide anaesthesia. Since then many methods have been described [1,2]. Several approaches have also been described for brachial blockade; these included interscalene, supraclavicular, infraclavicular, and the axillary approaches [3]. The access to the brachial plexus can be either by a nerve stimulator with an insulated needle or by ultrasound guidance for visualization of the nerves. In our study we explored the effect of the axillary approach for brachial block with a single injection with the aid of a nerve stimulator and insulated needle using a new formula for injection.
Patients and Methods
This retrospective study included 36 patients, aged between 25 and 67 years. The study spanned 6 months. Data were collected by reviewing patients’ notes. The time lapse from anesthesia to time of “knife to skin”, and time of actual pain relief were recorded. A questionnaire was distributed to evaluate patient satisfaction post-operatively. Elective hand surgery procedures were included in the study. Trauma cases were excluded. The new formula used was a combination of 1.5% lignocaine with 1 in 200,000 adrenaline and 1 ml of 8.4% sodium bicarbonate per 10mls of mixture. The amount varied between 25 ml’s and 35 ml’s. The technique used was trans-axillary single puncture with the aid of a nerve stimulator. The average time for administration of the block was 10 minutes per patient.
Results
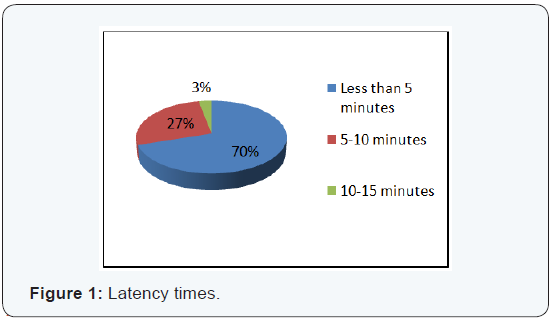
Our results were measured by time to surgery as well as the need for sedation and/or analgesia; as well as patient experience, which was recorded by a simple questionnaire taken by patients to reflect on their experience. Our study revealed an average time lapse of 15 minutes in between cases. All patients were very satisfied with the regional block. None of the patients required conversion to a general anaesthesia. Six patients required sedation (20%). This formula of injection offered rapid onset of action with latency of less than 5 minutes in 21 patients (70%), between 5-10 minutes in 8 patients (27%) and between 10-15 minutes in 1 patient (3%) (Figure 1). Long lasting post-operative pain control was achieved (average 6 hours). Six patients were excluded as we failed to collect the required data.
The success of peripheral nerve blocks is based on the ability to correctly identify nerves involved in surgery, and put an adequate dose of local anesthetic around them, to achieve a complete impregnation of all nerves involved in surgery [4].
An axillary block has been considered successful by most authors when analgesia was present in all areas subjected to surgical interventions. This definition is sufficient from a clinical point of view, but implies a falsely high success rate and makes comparison of the different block techniques difficult [5]. Techniques based on nerve location with a nerve stimulator have a higher success rate for peripheral nerve blocks than brachial plexus block [6]. However, this technique requires a nerve stimulator and, preferably, the use of insulated needles [7]. Sia et al. [1] used the four-injection axillary injection technique to achieve a faster onset and higher success rate [1]
Conclusion
Our results were measured by time to surgery as well as the need for sedation and/or analgesia; as well as patient experience, which was recorded by a simple questionnaire taken by patients to reflect on their experience. Our study revealed an average time lapse of 15 minutes in between cases. All patients were very satisfied with the regional block. None of the patients required conversion to a general anaesthesia. Six patients required sedation (20%). This formula of injection offered rapid onset of action with latency of less than 5 minutes in 21 patients (70%), between 5-10 minutes in 8 patients (27%) and between 10-15 minutes in 1 patient (3%) (Figure 1). Long lasting post-operative pain control was achieved (average 6 hours). Six patients were excluded as we failed to collect the required data.
With our technique we have a very high success rate at achieving complete anaesthesia in all the patients with a single injection, although there were differences in onset. Only 6 patients required midazolam in addition to the axillary block to control anxiety. Failure is not linked to the experience of the anesthesiologist, to the physical characteristics of patients, or to the injected volume [8]. There were no complications recorded with our technique. The common complications recorded include vascular puncture or intraneural injection and no paresthesias were observed, confirming the safety of this technique [9-12].
References
- Casati A, Danelli G, Baciarello M, Corradi M, Leone S, et al. (2007) A Prospective, Randomized Comparison between Ultrasound and Nerve Stimulation Guidance for Multiple Injection Axillary Brachial Plexus Block. Anesthesiology 106(5): 992-996.
- Dupre’ LJ (1992) Neurostimulateur en anesthesie loco-regionale. Can Anaesth 40: 503-510.
- Dupre’ LJ (1994) Brachial plexus block through humeral approach. Can J Anaesth 42: 767-769.
- a href="https://www.ncbi.nlm.nih.gov/pubmed/6486492"Ford DJ, Pither C, Raj PP (1984) Comparison of insulated and uninsulated needles for locating peripheral nerves with a peripheral nerve stimulator. Anesth Analg 63(10): 925-928.
- Gaertner E, Kern O, Mahoudeau G (1999) Block of the brachial plexus branches by the humeral route: a prospective study of 503 ambulatory patients—proposal of a nerve blocking sequence. Acta Anaesthesiol Scand 43(6): 609-613.
- Koscielniak-Nielsen ZJ, Hesselbjerg L, Fejlberg V (1998) Comparison of transarterial and multiple nerve stimulation techniques for an initial axillary block by 45 ml of mepivacaine 1% with adrenaline. Acta Anaesthesiol Scand 42(5): 570 -575.
- Martin R, Dumais R, Cinq-Mars S, Te´trault JP (1993) Axillary plexus block by simultaneous blockade of several nerves. I. Influence of the volume of the anesthetic solution. Ann Fr Anesth Reanim 12(3): 229- 232.
- Nelson ZK (2007) Axillary Brachial Plexus Block. Textbook of Anesthesia and Acute Pain Management. Hadzic A (Ed.), The Mcgraw- Hill, New York, USA, pp. 441-451.
- Sia S, Bartoli M, Lepri A, Marchini O, Ponsecchi P (2000) Multiple- Injection Axillary Brachial Plexus Block: A Comparison of Two Methods of Nerve Localization
- Urmey WF (1996) Upper Extremity Blocks. Regional Anesthesia and Analgesia. Brown DL (Ed.), W.B. Saunders Company, Philadelphia, USA, pp. 226-228.
- Wedel DJ, Horlocker TT (2005) Nerve Blocks. Anesthesia Volume 2 6th edition. Miller RD (Ed.), Churchill Livingstone, New York, USA, pp. 1685-1695.
- Gandy CL (1991) Anaesthesia for Dupuytren’s Contracture. Hand Clin 7(4): 695-704.






























