Surgical Management of Delayed Presentation of Osteochondral Knee Injuries in Adolescents - Case Series and Literature Review
*Samuel McMahon
Craigavon Area Hospital, Ireland
Submission: October 05, 2016; Published: October 21, 2016
*Corresponding author: Samuel McMahon, Craigavon Area Hospital 68 Lurgan Road Portadown BT63 5QQ, Ireland.
How to cite this article: Samuel M. Surgical Management of Delayed Presentation of Osteochondral Knee Injuries in Adolescents - Case Series and. 2016; 3(2): 555607. DOI: 10.19080/OROAJ.2016.03.555607
Abstract
Objective:Osteochondral fractures (OCF) are injuries to the articular surface of a joint containing both cartilaginous and bone components. Various methods have been reported for the treatment of these fractures in the acute setting. There is limited data on delayed fixation. We report two cases of delayed presentation and primary fixation of OCF with bioabsorbable osteochondral dart.
Cases: The first case was of a sixteen-year old boy with a twisting knee injury resulting in a displaced 22 mm OCF on the medial facet of the patella, identified on Magnetic Resonance Imaging (MRI). The second case was of a fifteen-year old boy who presented five months following a soccer injury with persistent left knee swelling and pain. MRI identified a displaced 22.5mm OCF of the lateral femoral condyle. Both patients underwent arthroscopic inspection followed by arthrotomy and fixation of the OCF using osteochondral darts, 5 weeks post injury in the first patient, and 6 months post injury in the second. There were no intra-operative or post-operative complications. Post-operatively, both were initially kept non-weight bearing in extension for 4 weeks, with graded increase in range of motion and weight bearing. Clinically at final follow up at 12 months both had a pain free, full range of motion. MRI in the second patient demonstrated osseous union of the fragment with some superficial fibrillation of the cartilage.
Conclusion: OThese cases demonstrate that late presenting OCFs can be successfully treated by primary internal fixation using bioabsorbable osteochondral darts.
Abbreviations: OCF: Osteochondral fractures; MRI: Magnetic Resonance Imaging; MPFL: Medial Patella Femoral Ligament; BMAC: Bone Marrow Aspirate and Concentrate Cells; MCIC: Mesenchymal Cell Induced Chondrogenesis
Introduction
Intertrochanteric fractures are very common among elderly patients. These fractures are cause of significant morbidity and mortality in conservatively treated patients. Because of that the treatment of choice is surgery. The most commonly used surgical method is internal fixation which is associated with intraoperative blood loos and prolonged anesthesia. The elderly patients are high risk patients for surgery and conservative treatment is a bad alternative as it is associated with a high mortality rate. The aim of this retrospective study was to evaluate the results of the external fixation for the treatment of intertrochanteric hip fractures in a group of high surgical risk elderly patients.
Surgical treatments have been developed, and are based on either fixation, via several methods, or regenerative procedures such as microfracture, osteochondral transplantation (allograft or autograft) or autologous chondrocyte implantation. Procedures such as microfracture, osteochondral transplantation (allograft or autograft) and autologous chondrocyte implantation. The current literature is dominated by case studies and small case series reporting the use of different methods in the acute setting. The impact of time to fixation on results has been identified as an important question that has not been addressed [5]. This is a pertinent question due to challenging nature of diagnosis in these patients by plain radiographs [6], leading to a large proportion of late presentations. We describe the results of two cases of OCF with fixation by bioabsorbable osteochondral darts, following late presentation.
Case 1
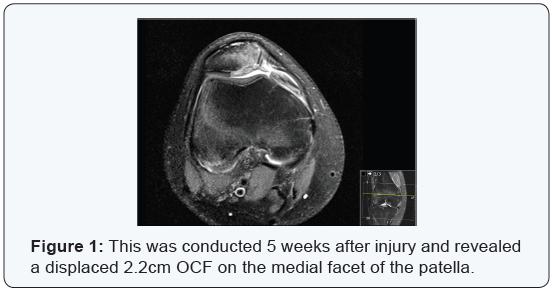
A sixteen-year-old boy reported a twisting injury while playing soccer, resulting in an acutely painful and swollen left knee. He had no history of previous trauma to the knee. On examination in the emergency department, there was an acute haemarthrosis and limited range of movement with the knee held in 20 degrees of flexion. There was no medial collateral or lateral collateral ligament instability. Cruciate ligament exam was precluded by pain. Anterior-posterior and lateral knee radiographs showed a skeletally mature knee with a haemarthrosis, but no acute bony injury was identified. He was placed in to an extended cylinder cast. Due to ongoing pain, he underwent magnetic resonance (MR) imaging. This was conducted 5 weeks after injury and revealed a displaced 2.2cm OCF on the medial facet of the patella (Figure 1).
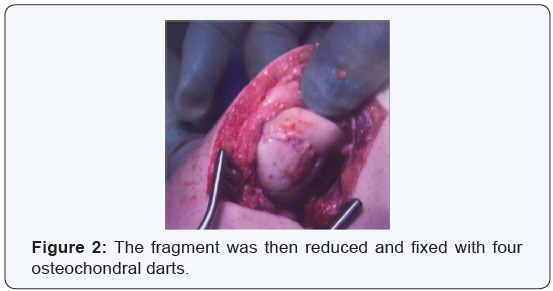
Seven weeks post injury; he underwent arthroscopic assessment followed by limited open arthrotomy and internal fixation of the fractured fragment. After confirming the presence of the fragment, he underwentmini-open arthrotomy. A tear of the Medial Patella Femoral Ligament (MPFL) was identified. The fragment was trimmed, and the base debrided of soft tissue, back to bleeding bone. The fragment was then reduced and fixed with four osteochondral darts (anthrax) (Figure 2), and stability checked in flexion. The MPFL was also repaired.
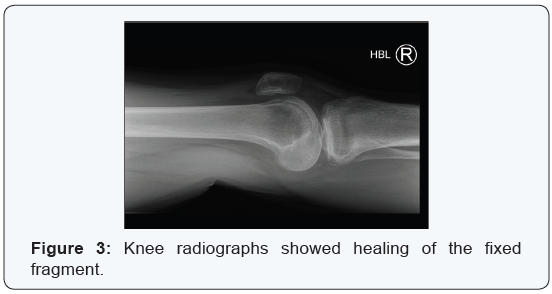
There were no intra-operative or post-operative complications. He was kept in an extension splint, with nonweight bearing mobilisation for 4 weeks. Under physiotherapist supervision, range of movement was progressively increased from 0 to 90 degrees, maintaining non-weight bearing for 6 weeks. He was then allowed flexion up to 90 degrees, with partialThere were no intra-operative or post-operative complications. He was kept in an extension splint, with nonweight bearing mobilisation for 4 weeks. Under physiotherapist supervision, range of movement was progressively increased from 0 to 90 degrees, maintaining non-weight bearing for 6 weeks. He was then allowed flexion up to 90 degrees, with partial
Case 2
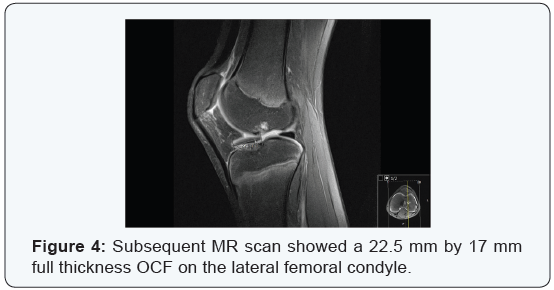
This fifteen-year-old boy presented to fracture clinic with a five-month history of left knee pain and swelling following an injury while playing soccer. Examination revealed a joint effusion and a range of movement from 10 to 135 degrees. There was moderate lateral joint line tenderness, and no ligamentous instability. Antero-Posterior and lateral knee radiographs demonstrated a skeletally immature knee, with a lucency in the lateral femoral condyle suggestive of an OCF. Subsequent MR scan showed a 22.5 mm by 17 mm full thickness OCF on the lateral femoral condyle (Figure 4), with subchondral cysts present anteromedially. On further review his range of movement had deteriorated 30 to 135 degrees. He underwent open reduction and internal fixation six months following onset of symptoms.
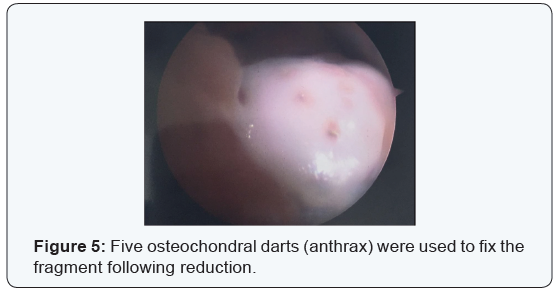
He underwent initial arthroscopy, which confirmed the presence of the fragment, and proceeded to open arthrotomy and internal fixation. Via a lateral parapatellar incision, the fragment was identified, and trimmed. The base of the fracture was debrided back to bleeding bone. Five osteochondral darts (anthrax) were used to fix the fragment following reduction (Figure 5). Stability was checked prior to closure. There were no intra-operative or post-operative complications. Postoperatively he was kept non-weight bearing in an extension splint for 6 weeks. Following this, flexion was increased to 0-30,
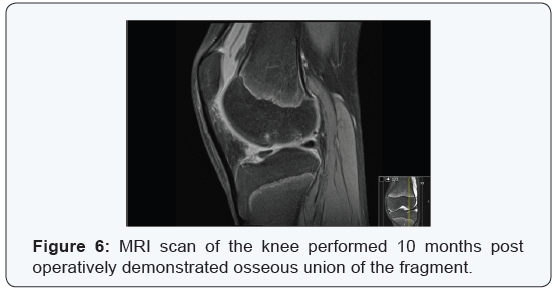
maintaining non-weight bearing. He was then allowed to flex from 0-90 and progress to partial weight bearing, for 6 weeks. After this, he was allowed free flexion and full weight bearing mobilisation under physiotherapist supervision, avoiding contact sport, while encouraging swimming and cycling. MRI scan of the knee performed 10 months post operatively demonstrated osseous union of the fragment (Figure 6). There was also some superficial fibrillation of the chondral component, but at no point was this full thickness. Clinically at final follow up at 12 months, he had a pain free, full range of movement. He was discharged back to previous levels of activity and sport.
Discussion
These cases demonstrate that late presenting OCFs can be successfully treated by primary internal fixation techniques. Diagnosis of OCF at the time of presentation requires a high level of clinical suspicion. Plain antero-posterior radiograph should be carefully inspected in the presence of a twisting knee injury or patella dislocation and haemarthrosis in an adolescent. Any suspected abnormalities should prompt urgent knee specialist referral and MR imaging, to allow early identification and appropriate management. The use of bioabsorbable dart fixation has previously been reported in the acute setting [7, 8], with good results. Historically, it was felt that late presenting fractures could not be accurately repaired, and therefore should be excised [1]. However, the cartilage defect predisposes to the development of early osteoarthritis [9], and therefore this does not provide an ideal long-term option. We therefore felt that anatomic reduction and fixation of these lesions provided the best chance of a good long-term functional outcome in these active young adolescent patients
We elected to confirm the presence, size and placement of the fracture via arthroscopic inspection prior to open arthrotomy. This ensures that the fragment is present as described on MRI, and further guides the extent and position of the arthrotomy incision. We feel that arthrotomy is particularly necessary in late presenting cases to ensure that a thorough debridement of both fragment and fracture site can be conducted. This allowed accurate and stable reduction and fixation of the fragment using bioabsorbable screws. These preclude the risk of metalwork displacement and damage to articular surfaces, and the potential need for a second procedure to remove them. A cautious approach to weight bearing and mobilisation is essential in these patients to protect the fixation of the fragment, preventing displacement, as both boney and chondral healing occur. Although this can result in short term knee stiffness, graded increase in range of motion provides a reliable return to full movement in these young patients. There are a number of different surgical options for these patients that can broadly be divided in to fixation methods or regenerative therapies. Fixation methods include the use of bioabsorbable screws, as in this study, and conventional headless screws [10]. Regenerative procedures are designed to stimulate healing and repair of cartilage. These include microfracture, osteochondral transplantation and autologous chrondrocyte implantation.
Microfracture aims to stimulate new cartilage growth and repair. An awl is used to make multiple holes in the subchondral bone beneath the defect. Bleeding creates a healing response, with the goal of producing new healthy cartilage. Microfracture provides good early results; however, there is evidence to suggest that clinical outcomes following microfracture deteriorate after eighteen to twenty four months [11]. Osteochondral autograft transplantation (OAT) involves taking a plug of cartilage and subchondral bone from a non-weight bearing part of the knee and then implanting it in to the defect. This can either utilise a single transplant, or multiple small plugs in a ‘mosaicplasty’. OAT and microfracture have recently been compared in a metaanalysis [12]. This appeared to show better clinical results with a higher rate of return to sport and maintenance of their sports function from before surgery compared to microfracture. The authors suggested that OAT is appropriate for lesions smaller that 2cm2.
There is also evidence to suggest that clinical outcomes following microfracture deteriorate after eighteen to twenty four months [11].Osteochondral allograft transplantation is a similar procedure to autograft transplantation, however cadaveric bone is used. This technique is burdened by cost, and difficulty finding appropriate donors. However, good clinical and functional outcomes have been demonstrated in systematic review [13], and this is an appropriate technique in large defects. Autologous chondrocyte implantation is a two-stage procedure. Healthy cartilage tissue is removed via an arthroscopy and cultured for 3 to 5 weeks. An arthrotomy is then performed to allow preparation of the defect site and a covering patch of periosteum to be placed over the defect. The chondrocytes are then injected in to the defect underneath the periosteal sleeve. This is postulated to form ‘hyaline like’ cartilage that is histologically closer to healthy articular cartilage than microfracture techniques. This has been shown to have a successful outcome in 72% of cases at a mean of 10.2 years in a recent meta-analysis [14]. However it does appear that failure rate increases as the size of the lesion increases. The recently developed technique of autologous bonemarrow Mesenchymal Cell Induced Chondrogenesis (MCIC) using bone marrow aspirate and concentrate cells (BMAC) for treating chondral defects [15,16] shows promising early results, but requires long term studies to evaluate its efficacy.
Conclusion
Early diagnosis and management of these fractures is ideal. However, good results can be achieved using primary fixation with bioabsorbable screws in late presenting cases especially in young skeletally immature patients who have the best chance of cartilage healing.
References
- Nomura E, Inoue M, Kurimura M (2003) Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 19 (7): 717-721.
- Matthewson MH, Dandy DJ (1978) Osteochondral fractures of the lateral femoral condyle: a result of indirect violence to the knee. J Bone Joint Surg Br 60-B (2): 199-202.
- Nietosvaara Y, Aalto K, Kallio PE (1994) Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 14(4): 513-515.
- Flachsmann R, Broom ND, Hardy AE, Moltschaniwskyj G (2000) Why is the adolescent joint particularly susceptible to osteochondral shear fracture? Clin Orthop Relat Res (381): 212-221.
- Kühle J, Angele P, Balcarek P, Eichinger M, Feucht M, et al. (2013) Treatment of osteochondral fractures of the knee: a meta-analysis of available scientific evidence. Int Orthop 37(12): 2385-2394.
- Stanitski CL, Paletta GA Jr (1998) Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med 26(1): 52-55
- Walsh SJ1, Boyle MJ, Morganti V (2008) Large osteochondral fractures of the lateral femoral chondyle in the adolescent: outcome of bioabsorbable pin fixation. J Bone Joint Surg Am 90(7): 1473-1478.
- Nakayama H, Yoshiya S (2014) Bone peg fixation of a large chondral fragment in the weight bearing portion of the lateral femoral condyle in an adolescent: a case report. J Med Case Rep 8: 316.
- Buckwalter JA, Brown TD (2004) Joint injury, repair, and remodelling: roles in post-traumatic osteoarthritis. Clin Orthop Relat Res (423): 7-16
- Lidder S, Thomas M, Desai A, Skyrme A, Armitage A, et al. (2016) Osteochondral fractures of the knee in skeletally immature patients: short-term results of operative fixation using omnitech screws. Acta Chir Orthop Traumatol Cech 83(1): 16-20.
- Harris JD, Siston RA, Pan X, Flanigan DC (2010) Autologous chondrocyte implantation: a systematic review. J Bone Joint Surg Am 92(12): 2220- 2233.
- Lynch TS (2015) Systematic review of autogenous osteochondral transplant outcomes. Arthroscopy 31(4): 746-754.
- De Caro F, Bisicchia S, Amendola A, Ding L (2015) Large fresh osteochndral allografts of the knee: a systematic clinical and basic science review of the literature. Arthroscopy 31(4): 757-765.
- Pareek A (2016) Long-term outcomes after osteochondral autograft transfer: a systematic review at mean follow-up of 10.2 years. Arthroscopy 32(6): 1174-1184.
- Chiang H (2011) Differences between chondrocytes and bone marrowderived chondrogenic cells, Tissue Eng Part A 17(23-24): 2919-2929.
- Shetty AA (2014) Autologous bone-marrow mesenchymal cell induced chondrogenesis: single-stage arthroscopic cartilage repair. Tissue Eng Regen Med 11: 247.






























