The Sauvé-Kapandji Procedure for Disorders of the Distal Radio Ulnar Joint in Patients with Rheumatoid Arthritis.
Ricardo Monreal* and Enrique Faedo
Centro Médico MEDEX, South America
Submission: August 29, 2016; Published: September 16, 2016
*Corresponding author: Ricardo Monreal, Centro Médico MEDEX, República de Panama 3065 2do piso, San Isidro-Lima, Peru, South America
How to cite this article: Ricardo M, Enrique F. The Sauvé-Kapandji Procedure for Disorders of the Distal Radio Ulnar Joint in Patients with Rheumatoid Arthritis. Ortho & Rheum Open Access J. 2016; 2(4): 555593. DOI: 10.19080/OROAJ.2016.02.555593
Abstract
Background: The distal radioulnar joint (DRUJ) is often affected early in rheumatoid arthritis. This retrospective long-term study evaluates the clinical and radiological results of the Sauvé-Kapandji procedure in rheumatoid wrists.
Purpose: The aim of this study was to review our clinical experience with the Sauvé-Kapandji procedure in the reconstruction of the rheumatoid distal radioulnar joint.
Patients and Methods: Twelve patients (12 wrists) having Sauvé-Kapandji procedure for the distal radio ulnar joint (DRUJ) between the years 2006-2014 were retrospectively reviewed. There were 7 males and 5 females. The mean age was 51 years (range, 31 to 71 years, SD=12.8) and the mean duration of follow-up was 16 months. The indications for surgery were prolonged pain on prosupination, tenderness over the DRUJ, and discomfort with a piano- key test as well as radiographic findings of DRUJ arthritis. Wrist posteroanterior (PA) views were used to evaluate the existence of DRUJ arthritis.
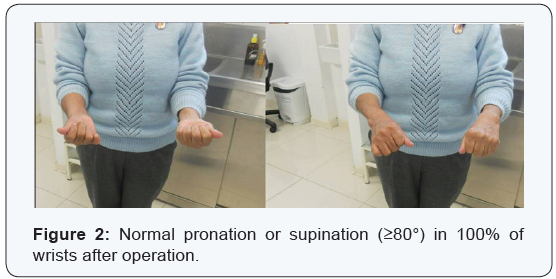
Results: The range of pronation and supination improved significantly. There was normal pronation or supination in 100% of wrists after operation. Painless bone union was achieved in all patients and carpal shift was unchanged when compared to films taken immediately after surgery. There was no dislocation of the ulnar stump on lateral radiographs.
Conclusion: The Sauvé-Kapandji procedure is a reliable treatment option. In our series it provided pain relief while preserving motion in rheumatic patients with distal radio ulnar arthritis.
Keywords: Rheumatoid arthritis; Sauvé-Kapandji procedure; Distal Radioulnar Joint; Carpal Translation
Abbreviations: RDRUJ: Distal Radio Ulnar Joint; PA: Posteroanterior; RA: Rheumatoid Arthritis; ROM: Range of Motion; MMWS: Mayo Wrist Score; TFCC: Triangular Fibro Cartilaginous Complex; ECU: Extensor Carpi Ulnaris; DRU: Distal Radio Ulnar
Introduction
Rheumatoid arthritis (RA) involves the wrist in up to 95% of cases. The distal radioulnar joint is affected in 31-75% of these patients and is frequently the first compartment of the wrist involved [1]. Long-standing rheumatoid arthritis results in ligamentous laxity. At the distal radioulnar joint this leads to the so-called ‘caput ulnae syndrome’ [2], dorsal subluxation of the distal part of the ulna, supination of the carpus on the forearm, and palmar dislocation of the tendon of the extensor carpi ulnaris [3-6]. The most common treatment for disorders of the distal radioulnar joint has been a transverse distal ulnar resection (Darrach procedure) [7]. However, postoperative ulnar carpal impingement syndrome, wrist instability, extensor tendon rupture, and diminished grip strength have all been associated with the Darrach procedure [8-11]. Another alternative in the management of distal radioulnar joint disorders is an arthrodesis with creation of a surgical pseudarthrosis of the distal ulna (Sauvé-Kapaandji procedure [12]. The aim of this study was to review our clinical experience with the Sauvé-Kapandji procedure in the reconstruction of the rheumatoid distal radioulnar joint.
Patients and Methods
Twelve patients (12 wrists) having Sauvé-Kapandji procedure for the DRUJ between the years 2006-2014 were retrospectively reviewed. There were 7 males and 5 females. The mean age was 51 years (range, 31 to 71 years, SD=12.8) and the mean duration of follow-up was 16 months. The indications for surgery were prolonged pain on prosupination, tenderness over the DRUJ, and discomfort with a piano- key test as well as radiographic findings of DRUJ arthritis. Wrist posteroanterior (PA) views were used to evaluate the existence of DRUJ arthritis. All patients provided informed consent to participate in this study.
Operative technique
The operative technique consists of a dorsal approach to the distal radio ulnar joint (DRUJ) with synovectomy and resection of 10-15 mm segment of the ulna proximal to the ulnar head. If ulnar recession for an ulnar positive variance is required, then excision of an ulnar segment of appropriate size is removed to allow the distal ulnar fragment to be pulled proximally to neutral ulnar variance maintaining a 15 mm gap while for patients with neutral or negative ulnar variance, a 15 mm segment of ulna is excised before screw fixation of the DRUJ. The cartilage from the DRUJ was removed, and the joint was fixed with one 3.5 mm Ø cancellous screw and other 3.5 mm Ø cortical screw proximally. Part of the pronator quadratus muscle was interposed between the two ends of the ulna to discourage bone healing. The ECU tendon was fixed on the dorsal aspect of the ulnar head with a flap from the retinaculum.
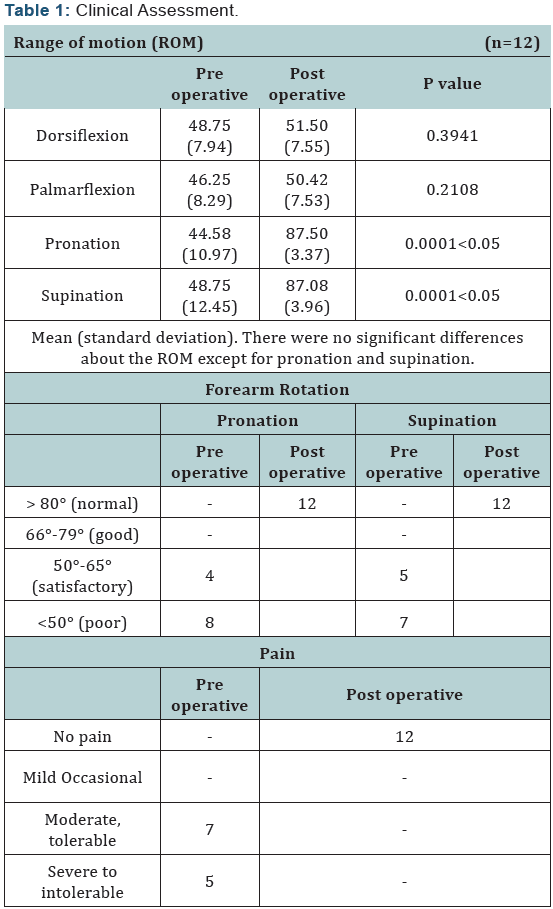
A plaster splint was worn for 10 days after surgery. Active pronationsupination exercises were started on the first postoperative day; unrestricted mobilisation was allowed after splint removal. Additional immobilization varied if extensor tendon ruptures or repairs were performed. Four of the 12 wrists with an extensor tendon rupture underwent a free tendon graft of the palmaris longus tendon. Measurements at last follow-upincluding range of motion (ROM), pain, and x-ray films were reviewed and compared with the preoperative values. The ROM measurement involved dorsiflexion, palmarflexion, pronation and supination. Differences between the groups were analyzed by Student’s t test. A P value <0.05 was considered to be statistically significant. With regard to supination and pronation, 80° of each was accepted as the lower limit of normal, 66°-79° as good, 50°-65° as satisfactory, and less than 50° as poor [13].
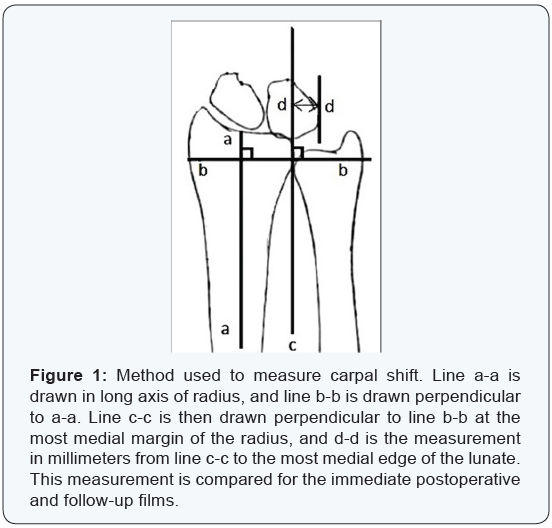
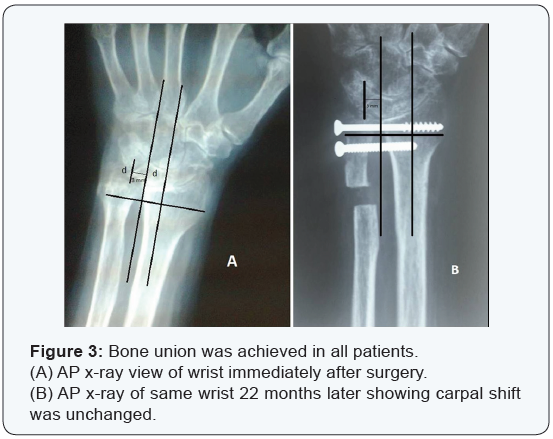
The assessment of pain was evaluated according to the Mayo Wrist Score (MMWS) [14]. Standard anteroposterior and lateral radiographs of the wrists were made. Features noted were fusion of the DRUJ, and carpal shift. Carpal shift was measured by the method shown in (Figure 1). This has been adapted from the method described by Gilula and Weeks [15]. The lunate measurement medial to the ulnar border of the radius (d-d) was compared in the immediate postoperative and follow-up x-rays. Grip strengths were not objectively measured, because they reflect multifactorial problems in the rheumatoid that cannot be appropriately controlled when evaluating a single joint [16].
Results
(Table 1) Clinical assessment indicated that there was no significant change in the dorsiflexion or palmarflexion of the wrist joint, while the range of pronation and supination improved significantly (p < 0.05).There was normal pronation or supination in 100% of wrists after operation (Figure 2). Preoperatively, all patients had moderate to severe pain facing the distal radioulnar joint but painless bone union was achieved in all patients. Carpal shift was unchanged when compared to films taken immediately after surgery (Figure 3). There was no dislocation of the ulnar stump on lateral radiographs.
Discussion
Rheumatoid arthritis (RA) involves the wrist in up to 95% of cases. The distal radioulnar joint is affected in 31-75% of these patients and is frequently the first compartment of the wrist involved [1]. Wrist involvement in rheumatoid arthritis (RA) usually begins on the ulnar side, and distal radioulnar joint (DRUJ) disorders such as arthritis and subluxation are a very common problem. The stability of the DRUJ is assured by the triangular fibrocartilaginous complex (TFCC) and the extensor carpi ulnaris (ECU). Additional stabilizers are the interosseous membrane and the pronator quadratus muscle. The distal radioulnar (DRU) joint is the keystone weight-bearing joint of the distal forearm. In rheumatoid arthritis, the ulnar column of the carpus tends to slide anteriorly with supination of the carpus. The DRU joint can dislocate with accentuation of the prominence of the ulnar head as a result of the anterior dislocation of the carpus and the radius. This creates caput ulnae syndrome [2]. The main goal of surgery of the rheumatoid wrist is a pain-free wrist with restoration of painless pronation/supination.
For DRUJ problems secondary to RA, there are two operations that are effective: resection the distal ulna and arthrodesis of the distal radioulnar joint combined with the creation of a pseudarthrosis of the distal ulna. Traditionally, resection of the distal ulna (the Darrach procedure) has been the operation of choice for most problems involving distal radioulnar degeneration but reported postoperative problems with this procedure have included distal ulnar instability, translation of the carpal bones in the ulnar direction, weakness, and pain of the wrist [8,9].
The resection of the distal end of the ulna was first report by Moore [17] in 1880 and popularized by Darrach [18,19] in 1912. The procedure was originally described and used in the treatment of traumatic derangements of the distal radio ulnar joint and the first report of its use in rheumatoid wrist surgery came from Smith Petersen [20]. This is an effective procedure in alleviating pain from DRUJ disease and distal ulna impingement on the carpus. The main concern of the Darrach procedure for RA is the potential ulnar translation of the carpus for patients with weak ligamentous support. For patients whose lunates are already migrating ulnarly, a concomitant radio-lunate fusion can be performed, provided that the midcarpal joint is intact.
Another option is the Sauvé-Kapandji procedure [12] for treating caput ulnae syndrome involving radioulnar arthrodesis with resection of an ulna segment. The review of literature shows clearly the positive effect of this procedure in terms of function [21-25]. Alternatively, arthrodesis of the distal radioulnar joint combined with a proximal ulna ostectomy and creation of a pseudarthrosis of the distal ulna to provide rotatory function (Suavé-Kapandji procedure) should be considered. The preserved ulna head gives support to the ulnar carpus and prevents ulnar translation of the carpus. A potential problem is the unpredictable fusion of the DRUJ when the bone stock in RA is not sufficient.
An interesting variation of this procedure is the Masada’s shelf arthroplasty procedure [26] in which the excised distal ulna is turned 90 degrees and inserted into the radius to promote better bone contact for fusion. There is a recent interest in replacing the distal ulna with prosthesis. The long-term outcome of this procedure has not been proven. DRU joint prostheses are under development and today are only indicated as a salvage procedure [27].
The sequential rupture of the extensor tendons of the fingers, beginning with the little finger, is a common and disabling complication of rheumatoid arthritis. It results from tenosynovial invasion of tendons or, more commonly, from their attrition on the ulnar head, as described in osteoarthritis of the distal radioulnar joint by Vaughan‐Jackson [28]. In our series 4 wrists with extensor tendon rupture underwent a free tendon graft of the palmaris longus tendon.
Conclusion
The Sauvé-Kapandji procedure is a reliable treatment option. In our series it provided pain relief while preserving motion in rheumatic patients with distal radio ulnar arthritis.
Statement of Informed Consent
All study participants provided informed written consent prior to study enrollment.
Statement of Human Rights
All procedures followed were in accordance with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study.
References
- De Smet L (2006) The distal radioulnar joint in rheumatoid arthritis. Acta Orthop Belg 72(4):381-386.
- Backhdal M (1963) The caput ulnae syndrome in rheumatoid arthritis. A study of the morphology, abnormal anatomy and clinical picture. Acta Rheum Scand 5: 1-75.
- Bachdahl M (1963) The caput ulnae in rheumatoid arthritis: a study of the morphology, abnormal anatomy, and clinical picture. Acta Rheumatol Scand 5:1-75.
- Straub LR, Ranawat CS (1969) The wrist in rheumatoid arthritis - surgical treatment and results. J Bone Joint Surg Am 51(1): 1-20.
- O’Donovan TM, Ruby LK (1989) The distal radial ulna joint in rheumatoid arthritis. Hand Clin 5(2): 249-256.
- Linscheid RL (1992) Biomechanism of the distal radioulnar joint. Clin Orthop Relat Res 275:46-55.
- Darrach W (1913) Partial excision of the lower shaft of the ulna for deformity following Colles’ fracture. Clin Orthop Relat Res 275: 3-4.
- Bell Ml, Hill Rl, McMurtry RY (1985) Ulnar impingement syndrome. J Bone Joint Surg Br 67(1):126-129.
- Bieber EJ, Linscheid RL, Dobyns JH, Beckenbaugh RD (1988) Failed distal ulna resections. J Hand Surg Am 13(2): 193-200.
- Minami A, Ogino T, Minami M (1987) Treatment of distal radioulnar disorders. J Hand Surg Am 12(2): 189-196.
- Newmeyer WL, Green DP (1982) Rupture of digital extensor tendons following distal ulnar resection. J Bone Joint Surg Am 64(2): 178-182.
- Sauvé L, Kapandji M (1936) Nouvelle technique de traitement chirurgical des luxations récidivantes isolées de l’extrémité inférieure du cubitus. J Chirurgie (Paris) 47: 589 -594.
- Rothwell AG, O’Neill L, Cragg K (1996) Simplified Sauvè-Kapandji Procedure for Disorders of the Distal Radioulnar Joint: A Simplified Technique. J Hand Surg Am 21(5): 771-777.
- Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP, et al. (1989) Scaphoid malunion. J Hand Surg Am 14(4): 679-687.
- Gilula LA, Weeks PM (1978) Post-traumatic ligamentous instability of the wrist. Radiology 129(3): 641-651.
- Vincent KA, Szabo RM, Agee JM (1993) The Sauvé-Kapandji procedure for reconstruction of the rheumatoid distal radioulnar joint. J Hand Surg Am 18(6): 978 -983.
- Moore EM (1880) Three cases illustrating luxation of the ulna in connection with Colles’ fracture. Med Rec 17.
- Darrach W (1992) Partial excision of the lower shaft of the ulna for deformity following Colles’ fracture 1913. Ann Surg 57:764 -765.
- Lau FH, Chung KC (2006) William Darrach, MD: his life and his contribution to hand surgery. J Hand Surg Am 31(7): 1056-1060.
- Smith-Petersen MN, AuFranc E, Larson CB (1943) Useful surgical procedures for rheumatoid arthritis involving joints of the upper extremity. Arch Surg 46: 764 -770.
- Low CK, Chew WY (2002) Results of Sauvé-Kapandji procedure. Singapore Med J 43(3): 135-137.
- Tran Van F, Obry C, Fardellone P, Decoopman M, Vives P (1993) Rehabilitation of the rheumatoid dorsal wrist by the Sauvé-Kapandji operation combined with a realignment stabilization synovectomy. Ann Chir Main Memb Super 12(2): 115-122.
- Taleisnik J (1992) The Sauvé-Kapandji procedure. Clin Orthop Relat Res 275: 110 -123.
- Papp M, Papp L, Lenkei B, Károlyi Z (2013) Long term results of the Sauvé-Kapandji procedure in the rheumatoid wrist. Acta Orthop Belg 79(6): 655-659.
- Toyama S, Tamai K, Sakamoto A, Hirashima T (2011) The short-term outcome of the modified Sauve´-Kapandji procedure regarding range of motion, carpal bone translation and bony shelf size. Mod Rheumatol 21(1): 37-42.
- Fujita S, Masada K, Takeuchi E, Yasuda M, Komatsubara Y, et al. (2006) Modified Sauve-Kapandji procedure for disorders of the distal radioulnar joint in patients with rheumatoid arthritis. Surgical technique. J Bone Joint Surg Am 88(1): 24-28.
- Ronit Wollstein, H Kirk Watson, Jan Phillips, Julio Clavijo, Viral Patel, et al. (2012) Ulnar sided wrist pain and distal radioulnar joint osteoarthritis; is surgical arthroplasty enough? Rheumatology Reports 4(1): 6-8.
- Vaughan‐Jackson OJ (1948) Rupture of extensor tendons by attrition at the inferior radio‐ulnar joint: report of two cases. J Bone Joint Surg Br 30(3): 528-530.






























