Hypercholesterolemia: “Protective Factor in Alzheimer's Disease“?
Gallego Moreno*1, Sanchez Santamaria2 and Corral Manuel de Villena3
1Department of Geriatrics, Spain
2Department of Geriatrician, Spain
3Department of Psychogeriatrics, Spain
Submission: July 05, 2017; Published: July 31, 2017
*Corresponding author: Jesus Alfonso Moreno Gallego, Department of Geriatrician, Tel: [+34} 912620795, [+34] 696360437; Email: gallegomoreno@yahoo.es
How to cite this article: Gallego M, Sánchez S, Corral M d V. Hypercholesterolemia: “Protective Factor in Alzheimer’s Disease”?. Organic & Medicinal Chem IJ. 2017; 3(1): 555604. DOI: 005 10.19080/OMCIJ.2017.03.555604.
Abstract
Background: Alzheimer disease (AD) has become one of the most common chronic diseases in developed countries. There are 35.6 million people worldwide with dementia in 2010. The medical literature shows that cardiovascular disease (CVD) and its risk factors (CRF) are associated with an increased risk of AD, and its precursor, mild cognitive impairment. The relationship between AD and vascular dementia is not only gnosological, but also has important therapeutic and preventive implications.
Objectives: Knowing the effect of major cardiovascular risk factors in a psychogeriatric population.
Design: Observational, transversal, with systematic selection of all patients who were admitted at the time of the study in the Nursing Home for the Elderly (RAPM) of CABM.
Setting: To compare qualitative variables, we used the chi-square test and odds ratio. We created a 2x2 contingency table with one degree of freedom, and was regarded as statistically significant p <0.05.
Participants: 212 residents from Benito Menni Complex Care (CABM).
Measurements: Hypertension was a 39.95%, the DM of 21.74%, 28.26% hypercholesterolemia, smoking a 23.91%, 30.43% obesity and a history of stroke 39.95% in patients with dementia.
Results: The odds ratio for these patients is 3.34, reaching the likelihood of dementia with the presence of more than two cardiovascular risk factors, the level of 76.95%.
Conclusion: An adequate control of cardiovascular risk factors, including hypercholesterolemia, so noticeable influence on the reduction of cognitive impairment and dementia in future generations.
Keywords: Alzheimer's Disease; Vascular Dementia; Mild Cognitive Impairment; Hypercholesterolemia; Cardiovascular Risk
Abbreviations: AD: Alzheimer disease; CVD: cardiovascular disease; DM: diabetes mellitus; CRF: Cardiovascular Risk Factors
Introduction
Alzheimer's disease (AD) has become one of the most common chronic diseases in developed countries. There are 35.6 million people worldwide suffering from dementia 2010. It's estimated that this number will double every 20 years to 65.7 million in 2030 and 115.4 million in 2050. Qne in eight men and nearly one in four women develop it during their lifetime [1]. The worldwide cost of dementia in 2005 amounted to 215 billion Euros per year, of which 155 billion (72% of world total) are invested by developed countries and 60 billion (28% of total) by countries developing and underdeveloped countries. Therefore, a better understanding of the etiology and prevention of AD is important in terms of public health.
The medical literature shows that cardiovascular disease (CVD) and its risk factors (CRF) are associated with an increased risk of AD and its precursor, mild cognitive impairment. Qn the other hand, the importance of the relationship between AD and vascular dementia is not only gynecological, but also has important therapeutic and preventive implications. To study the relationship between the two conditions is not easy. The diagnostic criteria of AD according to DSM-IV-R, exclude any patient with vascular dementia, because when there is an event or a cerebrovascular injury, a vascular dementia is considered. However, the relationship between both seems to exist at various levels [2].
Consistent epidemiological data indicate that CVD increases the risk of cognitive impairment and Alzheimer's disease [2]. Similarly, some cardiovascular risk factors are also associated with an increased risk of brain aging. Not yet established the mechanism to explain the relationship between CVD and AD, and many cardiovascular risk factors would be related to cognition regardless of its impact on vascular disease. Thus, it might be thought that changes in lifestyle and pharmacological interventions that reduce cardiovascular disease can also reduce AD and cognitive decline. The effect of CVD and cardiovascular risk factors in dementia remains an active research area, helping to establish which CRF has a clear impact on the AD. The finding of vascular risk factors for potentially correctable AD opens a new era in the field of prevention of AD [3].
Most studies seem to confirm that the harmful action of these factors occurs decades before the presentation of the disease. The fact that AD is present predominantly in the last period of life should guide our attempts to understand the factors that determine it. Probably the presence or absence of pathology is the complex result of protective and risk factors for many years and a genetic predisposition whose expression may also change over time and in relation to various environmental factors [4].
In recent years, has met major epidemiological evidence linking cardiovascular disease, cognitive impairment and AD [5]. This implies that preventive action will have very long-term planned and carried out in middle age, when the brain injury has not been yet produced. A better understanding of the role of vascular involvement in cognitive decline and Alzheimer's disease can have a significant impact on the development of effective preventive strategies. We present a study of psycho geriatric population, presenting psychiatric pathological basis, where it has been possible to establish the relationship of cardiovascular risk factors in these patients, and the presence of dementia or VD.
Materials and Methods
Design and Study Population: The target population is that people who's admitted into the Benito Menni Complex Care (CABM), from what this population was selected into the area of Psychogeriatrics, composed of 212 residents, with different pathologies. It has carried out an observational, transversal, with systematic selection of all patients who were admitted at the time of the study in the Nursing Home for the Elderly (RAPM) of CABM.
From the patient's clinical history were collected through a questionnaire on their age, the presence or absence of dementia, differentiating between Alzheimer's Disease (AD), Vascular Dementia (VD) and others, and the presence of risk factors, among those who were considered high blood pressure (hypertension), Diabetes Mellitus (DM), hypercholesterolemia, smoking, obesity and stroke (CVA). As we can see, we differentiate between patients with and without dementia and dementia type, while on the other hand we study the cardiovascular risk factors in relation to each other.
The diagnosis of AD, as well as DV, followed the DSM-IV-R. For the diagnosis of hypertension, DM, DLP is used clinical practice guidelines from the Spanish Society of Hypertension- Spanish League for the Fight against Hypertension (SEH-LELHA) for HBP [6], the American Diabetes Association for the DM [7], the European Society of Cardiology for hypercholesterolemia [8]. Within the point of obesity, the study included both overweight and obesity, cardiovascular risk factors considering body mass index (BMI) > 25. Both smoking and stroke were considered positive when there was addiction story for the first, as previous episodes for the second.
Statistical Analysis: One study describing the different variables. When qualitative variables, we used the absolute value and percentage, using the chi-square test We created a 2x2 contingency table with one degree of freedom, and was regarded as statistically significant p<0.05. They have drawn comparisons between the groups of patients with dementia for those not presented, taking into account the number of cardiovascular risk factors who had two groups, considering the breakpoint the presence of more than two risk factors, as indicated by some studies [9].
We also calculated the odds ratio of both the presence of dementia population with respect to the free of cognitive impairment, and several cardiovascular risk factors in relation to dementia, also obtaining the probability of occurrence of dementia according to cardiovascular risk factors studied. For the comparison between the AD and the VD, in some cases the patients were less than 5, so we had to use Fisher's exact test to determine statistical significance between the two conditions in our group, regarding several cardiovascular risk factors studied. Also used the odds ratio for greater or lesser likelihood of a relation to another disease, according to the CRF.
Results
We have included in the study 212 patients, of whom 46 (22%) had dementia, compared to 166 (78%) who did not. From the total, 43 (20.28%) were male and 169 (79.72%) women. Within the dementia group, 17 had AD, 10 vascular dementia, with the remaining 22, among which was the Korsakoff syndrome in 8 patients. With respect to gender, within the demented group, 43.47% were male, while in the group of non-demented men only reached 16.08%.
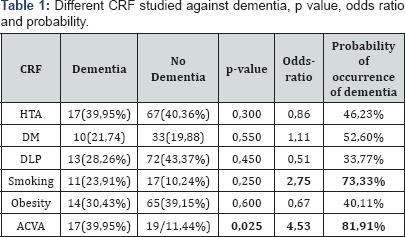
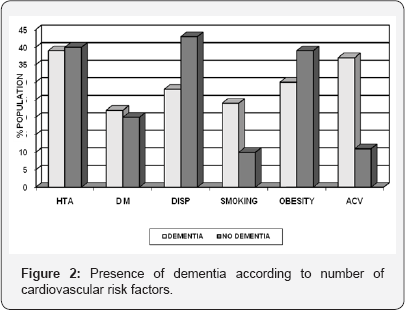
Cardiovascular risk factors: Cardiovascular risk factors compared in both groups, hypertension was 39.95% (17), DM 21.74% (10), hypercholesterolemia reached 28.26% (13), smoking by 23.91% (11), obesity, 30.43% (14) and a history of stroke 39.95% (17), all in the group of dementias. In the nondementia, the distribution was 40.36% (67) of patients suffering from hypertension, 19.88% (33) had DM, 43.37% (72) were hypercholesterolemic, 10.24% (17) smokers, 39.15% (65) were overweight or obese to be considered this factor when the BMI was greater than or equal to 25, and 11.44% (19) had suffered an acute stroke before the study time.
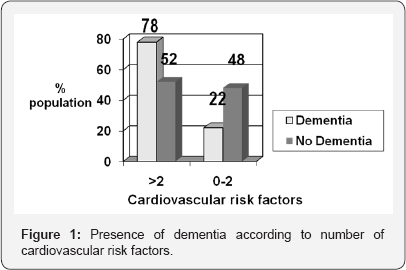
Differences according to presence or absence of dementia: We established a discretionary separation between those who had 0 to 2 CRF and those in the CRF were 3 or more. According to this criterion, we find that 10 (22%) patients with dementia and 80 (48%) without this condition belong to the first group, 36 (78%) patients with dementia and 86 (52%) dementia who belonged the second group of 3 or more cardiovascular risk factors.
In applying the chi-square, the value of it obtained for the presence of more than two cardiovascular risk factors is p=0.1, not to be significant. In contrast, if we perform the calculation of the odds ratio for these patients, the value is 3.34, reaching the likelihood of dementia with the presence of more than two cardiovascular risk factors 76.95% (Figure 1).
Differences by CRF: Table 1 presents the main differences described in the previous section, among patients with dementia and those who had not. In bivariate analysis, no statistically significant difference between various risk factors, except for the presence in their personal history of stroke (Figure 2), with p<0.05 (p=0.025). In a cross-sectional study, retrospective case- control, you cannot use the relative risk, should use the odds- ratio, which gives the association between cardiovascular risk factors and the presence of dementia. In our study, the presence of stroke both before and smoking are two factors that influence the onset of dementia, having no other factors influence this occurrence. The odds ratio of stroke compared to dementia is 4.53, and smoking about the insanity 2.75. This means that the probability of occurrence of dementia in patients who have suffered a stroke and TIA is 81.91%, while those with smoking also reached 73.33%. A striking result is the odds-ratio of the DLP about dementia, which is 0.51, which means that the probability is only 33.77%, being a protective factor of course.

Differences between AD and VD as CRF: In a comparison between AD and VD, we encounter the problem that in the sample, in one of the crosses made with several cardiovascular risk factors, the value n of the sample was equal to or less than 5. To correct this bias, we had to use Fisher's exact test (Table 2). This test allowed us to compare the AD on the VD according to several cardiovascular risk factors (Figure 3). In this comparison, we obtained figures were not statistically significant between the two processes, with regard to cardiovascular risk factors, except in the case of the previous presence of stroke, which marked a significant trend toward the presence of VD as the cause of the picture. The p, with Fisher's exact test, was in this case of 0.0034 (p<0.05), obtaining statistical significance.

Discussion
Several studies suggest that Cardiovascular Risk Factors (CRF) can affect the neurodegenerative process, leading to dementia in general and Alzheimer's disease and vascular dementia in particular [10-13]. In our study, the importance of cardiovascular risk factors is demonstrated and there is a direct relationship between the number of cardiovascular risk factors and the presence of dementia in these patients. The choice of the cutoff in the number 2 (0-2,>2), consistent with other studies [9] where from three CRF is when the difference becomes significant.
Smoking and previous history of stroke are associated with a higher risk of dementia, which is consistent with other studies in this field [14,15]. However, we also get that high cholesterol appears to be a protective factor assumption, which contradicts numerous studies that exist on this aspect [16]. The presence within the patient's history of diagnosis of hypercholesterolemia, with subsequent analytical tests, in which a large group rather return to optimal values of cholesterol and triglycerides, and lipid-lowering by diet, would explain to hypercholesterolemia appeared as a protective factor. Epidemiological studies have evaluated the relationship between statin therapy and the development of Alzheimer's disease [17,18]. These studies have found that the incidence of Alzheimer's disease is lower in the group of people treated with statins. These statins could become one of the specific treatments for patients with cognitive impairment who have cardiovascular risk factors [19].
Previous studies have found increased risk in the incidence of dementia in individuals with cardiovascular risk factors such as smoking [20], hypertension [21,22], hypercholesterolemia [9]. We only found this high risk with regard to smoking, there remains significant differences in the two other aspects Association between AD and VD is complex. Both increases in prevalence with age, and often occur concomitantly, there is considerable overlap of symptoms, pathophysiology, and comorbidity between both entities [23].
There is abundant evidence suggesting that the vascular damage produced in stroke carries a higher risk for the onset of dementia, especially vascular type [24,25]. In fact, the definition of vascular dementia according to DSM-IV-R expressly includes the presence of cerebrovascular disease that is etiologically related to the alteration (e.g. Multi-infarct involving the cortex and white matter companion). In our study, the only difference between the various cardiovascular risk factors on the two most important paintings of dementia, AD and VD, could be seen in the previous presence of episodes of stroke. The VD showed a statistically significant difference with p<0.05 (p=0.0034). The probability of dementia was Alzheimer's disease, having previously suffered an acute stroke, was only 5.39%. However, amounted to 94.61% the probability that it was a VD.
Our study has limitations as possible which is a psycho- geriatric population study in which psychiatric disorders may cause the proportion of dementia is higher, causing a population bias. Therefore, the study was carried out routinely on all patients admitted, without exclusion criteria based on age or condition, which may increase the selection bias. It has been found in some studies the association between certain cardiovascular risk factors and dementia may be biased by patient education [26,27]. As this population with a psychiatric background disease, psychiatric disease course with chronic, deteriorated patients, we believe that, despite the possible confusion that could lead to bias this circumstance is compensated because of the long detention of such patients.
Another possible limitation would be that exposure to cardiovascular risk factors are more controlled than in the general population, since it is a residential population sample, where the analytical tests, dietary and environmental requirements are more effective than in the general population. This could also be the explanation of the paradox mentioned above in that hypercholesterolemia course appears as a protective factor. As strength of our study, we noted that the population, to be admitted to the psychogeriatric area, has a homogeneous nature, allowing more weight in the results. The coincidence of results with other studies conducted on the same subject, and our study has been made on psychogeriatric population allows us to glimpse the influence of cardiovascular risk factors in the onset of dementia is universal and independent, therefore, other psychiatric disorders.
Conclusion
In conclusion, we can say that dementia is clearly influenced by different risk factors, highlighting the smoking and the presence of prior cerebrovascular disease. On the other hand, we see that the cardiovascular risk factors are common to both Alzheimer's disease as VD, establishing himself as only difference the presence in the natural history of episodes of stroke patients. This brings us to confirm the importance of primary prevention measures to the different risk factors, may assert that a proper control of these factors will influence significantly in reducing cognitive impairment and dementia in future generations.

Conflict of Interest Disclosures:
Author Contributions:
JA Gallego Moreno: Study concept and design; acquisition of subjects and data; analysis and interpretation of data; preparation of manuscript.
E Sanchez Santamaria: Acquisition of subjects and data; preparation of manuscript.
E Corral Manuel de Villena: Acquisition of subjects and data.
Sponsor’s Role: There isn’t any sponsor in the design, methods, subject recruitment, data collections, analysis and preparation of paper.
References
- Hebert LE, Scherr PA, Bienias JL, Bennett DA, et al. (2003) Alzheimer disease in the U.S. population: Prevalence Estimates using the 2000 census. Arch Neurol 60(8): 1119-1122.
- Stampfer MJ (2006) Cardiovascular disease and Alzheimer's disease: common links. J Intern Med 260(3): 211-123.
- Regalado PJ, Azpiazu Artigas P, Sanchez Guerra ML, et al. (2009) Vascular risk factors and Alzheimer's disease. Rev Esp Geriatr Gerontol 44(2): 98-105.
- Kivipelto M, Solomon A (2006) Cholesterol as a Risk Factor for Alzheimer's disease-Epidemiological Evidence. Acta Neurol Scand Suppl 185: 50-57.
- E Duron, O Hanon (2008) Vascular Risk Factors, cognitive decline, and dementia. Vas Health Risk Manag. 4(2): 363-81.
- Spanish Society of Hypertension-Spanish League for the Control of Hypertension (2005) (SEH-LELHA). Spanish Guidelines on Hypertension. Hypertension: 22.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010.
- Graham I, Atar D, Borch Johs K (2008) Clinical practice guidelines on prevention of cardiovascular disease: summary. Fourth working group of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice. Rev Esp Cardiol 61(1): E1-E49.
- Alonso A, Dontas A, Kafatos A, Kromhout D (2009) Cardiovascular Risk Factors and Mortality dementia: 40 years of follow-up in the Seven Countries Study. J Neurol Sci 280: 79-83.
- Oijen M, de Jong FJ, Witteman JCM (2007) Atherosclerosis and Risk for dementia. Ann Neurol 61(5): 403-10.
- Newman AB, Fitzpatrick AL, Lopez O (2005) Dementia and Alzheimer's disease incidence, in Relationship to cardiovascular disease in the Cardiovascular Health Study Cohort. J Am GeriatrSoc 53: 1101-1107.
- Hayden KM, Zandi PP, Lyketsos CG, Khachaturian AS (2006) Vascular Risk Factors for incident Alzheimer disease and vascular dementia: the Cache County Study. Alzheimer Dis Assoc Disord 20(2): 93-100.
- Akomolafe A, Beiser A, Meigs JB, Au R (2006) Diabetes Mellitus and Risk of Developing Alzheimer disease: results from the Framingham Study. Arch Neurol 63(11): 1551-1555.
- Hernán MA, Alonso A, Logroscino G (2008) Cigarette smoking and dementia: Potential selection bias in the elderly. Epidemiology 19(3): 448-450.
- Staessen JA, Richart T, Birkenhager WH (2007) Less atherosclerosis and lower blood pressure for a Meaningful life perspective with more brain. Hypertension 49(3): 389-400.
- Anstey KJ, Lipnicki DM, Low LF (2008) Cholesterol as a Risk Factor for dementia and cognitive decline: a Systematic review of prospective studies with meta-analysis. Am J Geriatr Psychiatry 16: 343-54.
- Zamrini E, Mc Gwin G, Roseman JM (2004) Association Between statin use and Alzheimer's disease. Neuroepidemiology 23(1-2): 94-8.
- Li G1, Higdon R, Kukull WA, Peskind E (2004) Statin therapy and of dementia in the elderly: a community-based prospective cohort study. Neurology 63(9): 1624-1628.
- Gich J, Quintana M, Zambon D (2005) Is There relation entre cholesterol and cognitive impairment? Clin Invest Arterioscler. 17 (1): 48-53.
- Anstey KJ, von Sanden C, Salim A (2007) Smoking as a Risk Factor for dementia and cognitive decline: a meta-analysis of prospective studies. Am J Epidemiol 166: 367-378.
- Launer LJ, Ross GW, Petrovitch H, Havlik RJ (2000) Midlife blood pressure and dementia: the Honolulu-Asia Aging Study. Neurobiol Aging 21(1): 49-55.
- Kivipelto M, Helkala EL, Laakso MP (2001) Midlife Vascular Risk Factors and Alzheimer's disease in Later Life: longitudinal, population based study. BMJ 322: 1447-1451.
- Kalaria R (2002) Similarities between Alzheimer's disease and vascular dementia. Neurol Sci 203-204: 29-34.
- Honig LS1, Tang MX, Albert S, Costa R, Luchsinger J (2003) Stroke and the Risk of Alzheimer disease. Arch Neurol 60: 1707-1712.
- Vermeer SE, Prins ND, den Heijer T (2003) Silent brain infarcts and the Risk of dementia and cognitive decline. N Engl J Med 348(13): 12151222.
- Caamano-Isorna F, Corral M, Montes-Martinez A (2006) Education and dementia: a meta-analytic study. Neuroepidemiology 26: 226-232.
- Fernandez, Garcia M, Schiaffino A, Borras JM (2001) Smoking Initiation and Cessation by Gender and Educational Level in Catalonia, Spain. Prev Med 32: 218-223.






























