Increase In Neurooncology Surgeries During COVID-19 Pandemic: A Single-Center Experience
Messias Gonçalves Pacheco Junior*¹, Pedro El Hadj de Miranda², Tadeu Francisco Dos Santos², Marcus André Acioly1, Rafael Abbud Fernandes1, Nicoly Augusta da Silva Quezada dos Santos¹, José Alberto Landeiro1 and Bruno Lima Pessôa1
1Division of Neurosurgery, Antônio Pedro University Hospital, Fluminense Federal University, Brazil
2Medical student at the Antonio Pedro University Hospital, Federal Fluminense University, Brazil
Submission: January 18, 2022; Published: February 02, 2022
*Corresponding author: Messias Goncalves Pacheco Junior, Resident of Neurosurgery, Department of Surgical Specialties, Division of Neurosurgery, Antônio Pedro University Hospital, Federal Fluminense University, Av. Marques do Paraná, 303 – Centro – Niterói - RJ -Brazil
How to cite this article: Messias Gonçalves Pacheco Junior*, Pedro El Hadj de Miranda, Tadeu Francisco Dos Santos, Marcus André Acioly, Rafael Abbud Fernandes, et al. Increase In Neurooncology Surgeries During COVID-19 Pandemic: A Single-Center Experience. Open Access J Neurol Neurosurg 2021; 16(5): 555946. DOI: 10.19080/OAJNN.2022.16.555946.
Abstract
Background: The COVID-19 pandemic affected the care of patients in all specialties. During this period, the focus was treating respiratory diseases, with oncology patients being neglected. This study aims to describe the behavior of neuro-oncology care at Antonio Pedro University Hospital (HUAP). This direct impact occurred in the patients given the coronavirus pandemic identified in 2019 and compare it with the known literature.
Methods: This is an observational, retrospective, and prospective study. This study involved the tertiary neurosurgical center serving the metropolitan region of Rio de Janeiro state. All neuro-oncology admissions in the period between March 2020 and December 2020 were prospectively captured. Thus, these data were compared in the same period immediately a year before the mentioned above. In addition, one performed a review of the relevant literature in the PubMed database.
Results: An increase of 47,8% of neuro-oncology surgeries during the pandemic period was observed. Most of those cases consisted of brain tumors (92,6%), while spinal tumors were less frequent (7,35%). Emergencies surgeries were responsible for the majority of cases (65%). Neurosurgical complications rates were present in 15,25% of patients.
Conclusion: The COVID-19 pandemic brought profound consequences in the provision of treatment for neuro-oncology disorders globally. Unlike other centers worldwide, we observed an increase in the demand for neuro-oncology patients at our institution, in addition to a rise in cases of urgent surgeries.
Keywords: Covid-19 pandemic; Oncology; Neurosurgery, Neuro-oncology surgery; Public health system
Introduction
The worldwide public health crisis caused by the Coronavirus pandemic 2019 brought concerns to those who suffered from COVID itself and patients who suffered from diseases that needed immediate treatment. [1-5] Since March 2020, a significant challenge to reconcile neurosurgical demands and those arising from the pandemic have appeared [6-10]. Mostly, there was a decline in elective surgical procedures, with surgical teams being reorganized for emergency care and in some places being relocated to support the intensive care unit [6,11-14]. In addition, many countries needed to invest in measures to reduce contagion by coronavirus. Thus, the development of protocols, such as mass testing and the improvement of telemedicine, was necessary to enable neurosurgical centers to perform surgeries. [2,3,6,11,12] This manuscript describes the paradigm shift made in our institution to continue performing neurosurgeries during the pandemic.
Materials and Methods
This study is a comparative, prospective, and retrospective register of the neuro-oncologic surgeries between March and December during two consecutive years. It started before the Covid-19 pandemic (2019) and ran through the pandemic period (2020). Based on patients’ charts, one made a comparative description from the Neurosurgery service throughout these two periods. Non-oncology surgeries were excluded. One also included all neurosurgical procedures related to neuro-oncology complications. We divided the types of neuro-oncologic surgeries from 2020 between cranial and spine surgeries, urgency character, histological subtypes, postoperative complications and compared them with the 2019 series. Finally, we made a review of the relevant literature on Covid-19 vs. Neuro-oncology in the PubMed database.
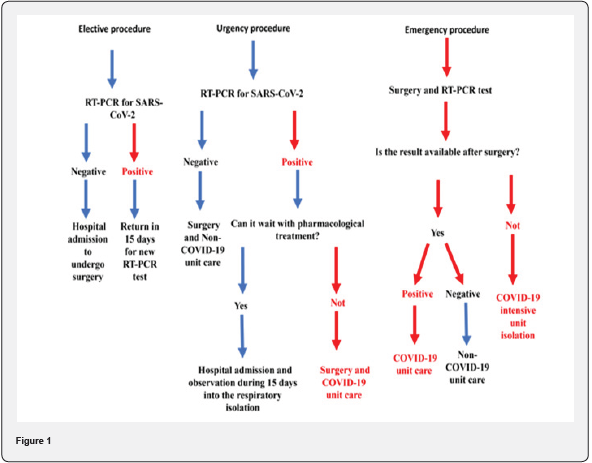
One used percentual data and means for statistical analyzes. Variables as surgical procedures number, tumor topography, classification of surgical procedure (elective, urgency, and emergency) were obtained and compared between 2019 and 2020. We also analyzed postoperative complication and histopathological types, then compared the results with other publications. The hospital infection control committee used various screening means to track the patients admitted to the hospital. Initially, patients without flu-like syndrome would undergo non-contrast chest tomography and unspecific infectious blood tests. In cases of both negative tests, the patient was transferred. Over time we included tests such as SARS-CoV-2 Antigen search and RT-PCR for SARS-CoV-2 in patients’ screening. However, we identified many cases of false negatives with antigen for SARS-CoV-2, causing the closing of the inpatient wards to isolate the patients placed there. Nowadays, RT-PCR is exclusively used for all patients who will undergo neurosurgical procedures (Figure 1).
Results
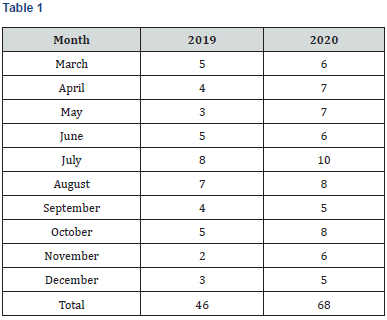
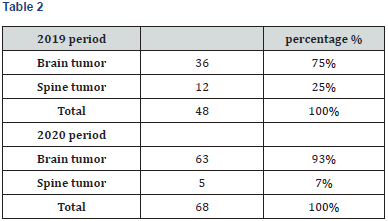
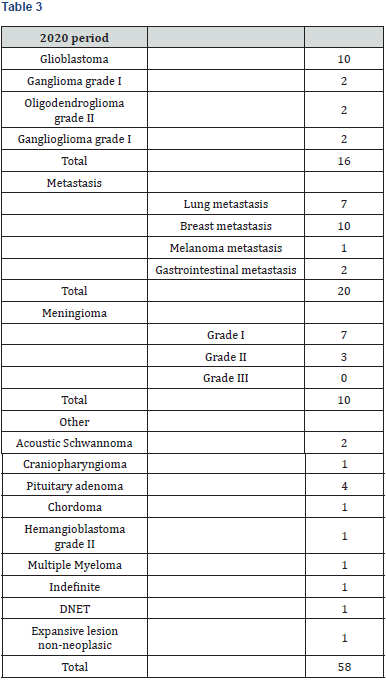
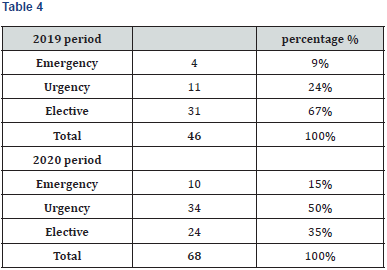
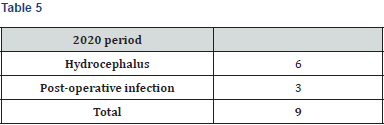
One observed an increase of 47,8% of neuro-oncology surgeries between the pre and pandemic period (Table 1). There were way more brain tumors during the pandemic than spinal tumors (Table 2). Metastatic tumors were more frequent, corresponding to 34% of the total. Unlike the existing literature, glioblastomas corresponded to the same frequency as meningiomas (17,2%). The classification of neurosurgical intervention was divided into 03 groups (Tables 3 & 4). The urgency procedures group included expansive lesions with a compressive effect and neurological deficits without threatening the patients’ lives immediately. Emergency intervention when there is an immediate risk of death. Elective procedures are classified as those that do not present an immediate or short-term risk to patients` lives. A reversal of the characteristic of the surgeries was observed during this period (Table 4). Neurosurgical complications were present in 15,25% of patients, including hydrocephalus and infections (Table 5).
Discussion
The COVID-19 pandemic profoundly altered the functioning of the health system globally. During this period, several health institutions suspended their activities, turning their resources to the care of respiratory emergencies. However, our neurosurgical department continued its activities, treating mainly cancer patients. Outpatient consultations were suspended, such as in several hospitals worldwide except for pre-and postoperative care of patients with oncological diseases attended [2,9,13]. During the period from March to December 2020, most patients operated on were admitted through inter-hospital transfer.
Before the availability of the use of the RT-PCR test for SARSCoV- 2, transnasal endoscopic surgeries were postponed due to the risk of contact with aerosols possibly infected by COVID-19 [2,4,7,8]. In cases where it was not possible to postpone the procedure, surgeries through craniotomies were the first option. In our series, we had only one case of neurosurgical emergency related to a pituitary tumor in a patient with COVID-19. This patient underwent transcranial surgery for brainstem decompression. After the RT-PCR test was routinely available, all patients with indications for transnasal endoscopic approach were operated, provided that the RT-PCR was negative.
When it was a neurosurgical emergency and the RT-PCR test for SARS-CoV-2 was detectable, the operating room was physically isolated from the rest of the surgical block. It consisted of an anesthesiologist and a resident, a scrub nurse, an assistant technician, and the surgical team. All appropriately dressed with personal protective equipment. In addition, a technical assistant was immediately outside the operating room, providing the necessary materials through the assistant who was exclusively inside the operating room. After the end of the procedure, the patient was immediately referred to the COVID-19 intensive care unit.
Contrary to most papers published in the literature, which described a reduction in the total number of general and oncological surgeries, our institution significantly increased the number of neurooncology surgeries [5,7,9,13]. Firstly, our hospital has not been center for COVID-19 treatment. Secondly, the majority of neurosurgical centers gave up doing surgeries during the pandemic, and their employees were relocated to treat Covid-19 patients, creating an increased demand for our service. Finally, with an engaged neurosurgical team we were able to keep concentrated on our patients with oncology illnesses without delaying their treatments.
Mohammad H. et al. reported that 19 patients underwent craniotomy for biopsy or brain tumor resection in the prepandemic period, whereas this number was ten patients during the pandemic moment. However, the percentage increased comparatively between two periods (9% vs. 11%) [9] N. Goyal et al. showed statistical significance in the inversion of the proportion between elective surgeries with the increase of emergent surgeries and the decrease in the total number of surgeries [5]. This finding is in the same line as ours, which is explained by the decrease in care offered by other tertiary neurosurgical services and outpatient care. This reduced offer of care increases the demand for emergency surgeries due to the disease progression of non-operated or late operated patients. Similarly, one noticed a decrease in the absolute amount of spinal surgeries comparing to the cranial ones. This observation is in the same direction as Antony G. et al. described, who reported a reduction in cranial and spinal elective procedures, even though emergency cranial surgeries had decreased less proportionally [2]. This fact can be explained by the public policy of stay at home.
Spinal oncological illnesses commonly present as isolated pain, unlike cranial disorders that lead to neurological deficits. Therefore, probably the patients with pain underestimated the symptoms and searched less to the health system. Additionally, Shakra IA. et al. made a comparative study on the characteristics of general surgery patients to admit in an Israeli hospital between three distinct periods: the COVID-19 outbreak, the Second Lebanon War in 2006, and a regular period. Compared to the routine period, patients with pain during the COVID-19 outbreak waited longer before seeking health care. They also conclude that pain was reportedly more significant during COVID-19 than in the control period (8.7 vs. 6.4 using the visual analog scale). Thus, it is probably related to the progression of the illness and the challenges of controlling pain in advanced cancers [1].
Study limitations
The patients’ data were from a single center with a relatively small number of patients. Due to the diverse nature, the collection and analysis of retrospective data from 2019 suffered losses of information that would allow comparative analysis to be more accurate. In addition, the stay-at-home policy may have underestimated the total number of patients with spinal oncological diseases that required neurosurgical evaluation and treatment.
Conclusion
The changes observed in the health system guidelines for the COVID-19 pandemic brought profound consequences in providing treatment for neuro-oncology disorders. Despite the increased supply at our institution for the treatment of neuro-oncological patients, there was a significant and unexplained decrease in the demand for cases of spinal oncological illnesses. In addition, an inversion of the profile of surgical care has occurred, with more urgent surgeries being performed. Despite the above-mentioned epidemiologic changes, we performed more neurooncology surgeries than other centers worldwide. We should keep in mind that COVID-19 is a life-threatening condition. However, neurooncology care should always be a priority.
References
- Abu Shakra I, Bez M, Ganam S, Francis R, Multi A, et al. (2021) The volume of general surgery emergency cases in a government hospital during the COVID-19 pandemic and two other periods: a comparative, retrospective study. BMC Surg 21(1): 119.
- Antony J, James WT, Neriamparambil AJ, Barot DD, Withers T (2020) An Australian Response to the COVID-19 Pandemic and Its Implications on the Practice of Neurosurgery. World Neurosurg 139: e864-e871.
- Bajunaid K, Alatar A, Alqurashi A, Alkutbi M, Alzahrani AH, et al. (2020) The longitudinal impact of COVID-19 pandemic on neurosurgical practice. Clin Neurol Neurosurg 198: 106237.
- BOUSQUET, Alex da Silva. DIAGNÓSTICO DE SAÚDE DA REGIÃO METROPOLITANA II. Niterói: Secretaria de Estado de Saúde do Rio de Janeiro, 154 pp.
- Goyal N, Venkataram T, Singh V, Chaturvedi J (2020) Collateral damage caused by COVID-19: Change in volume and spectrum of neurosurgery patients. J Clin Neurosci 80: 156-161.
- Khalafallah AM, Jimenez AE, Lee RP, Weingart JD, Theodore N, et al. (2020) Impact of COVID-19 on an Academic Neurosurgery Department: The Johns Hopkins Experience. World Neurosurg 139: e877-e884.
- Koester SW, Catapano JS, Ma KL, Kimata AR, Abbatematteo JM, et al. (2021) COVID-19 and Neurosurgery Consultation Call Volume at a Single Large Tertiary Center with a Propensity-Adjusted Analysis. World Neurosurg 146: e768-e772.
- Kondziolka D, Couldwell WT, Rutka JT (2020) Introduction. On pandemics: the impact of COVID-19 on the practice of neurosurgery. J Neurosurg 10:1-2.
- Noureldine MHA, Pressman E, Krafft PR, Greenberg MS, Agazzi S, et al. (2020) Impact of the COVID-19 Pandemic on Neurosurgical Practice at an Academic Tertiary Referral Center: A Comparative Study. World Neurosurg 139: e872-e876.
- Rothrock RJ, Maragkos GA, Schupper AJ, McNeill IT, Oermann EK, et al. (2020) By the Numbers Analysis of Effect of COVID-19 on a Neurosurgical Residency at the Epicenter. World Neurosurg 142: e434-e439.
- Rupa R, Sass B, Morales Lema MA, Nimsky C, Voellger B (2020) The Demand for Elective Neurosurgery at a German University Hospital during the First Wave of COVID-19. Healthcare (Basel) 8(4): 483.
- Sarfaty M, Feldman DR, Morris MJ, Motzer RJ, Rathkopf DE, et al. (2021) Genitourinary Medical Oncology Expert Opinion Survey Regarding Treatment Management in the COVID-19 Pandemic. Clin Genitourin Cancer 19(3): e178-e183.
- Venkataram T, Goyal N, Dash C, Chandra PP, Chaturvedi J, et al. (2020) Impact of the COVID-19 Pandemic on Neurosurgical Practice in India: Results of an Anonymized National Survey. Neurol India 68(3): 595-602.
- Zoia C, Bongetta D, Veiceschi P, Cenzato M, Di Meco F, et al. (2020) Neurosurgery during the COVID-19 pandemic: update from Lombardy, northern Italy. Acta Neurochir (Wien) 162(6): 1221-1222.






























