Haemophilia C: What is Unknown
Almottesembellah Gaiz1,2 and Sapha Mosawy1*
1School of Medical Sciences, Griffith University, Australia
2 National Centre of Haematology, University of Al-Mustansiriyah, Iraq
Submission: June 01, 2018; Published: July 02, 2018
*Corresponding author: SaphaMosawy, Menzies Health Institute Queensland, Griffith University, Gold Coast Campus, Australia.
How to cite this article: Almottesembellah Gaiz, Sapha Mosawy. Haemophilia C: What is Unknown. Open Acc Blood Res Trans J. 2018; 2(3): 555589. DOI: 10.19080/OABTJ.2018.02.555589
Abstract
Haemophilia C is a rare blood coagulation disorder caused by a deficiency of coagulation factor XI. The incidence is unusually high amongst ethnic Jewish groups. Genetic mutations resulting from nonsense, insertion, splice site, deletion and missense have been shown to lead to FXI deficiency. There is little to no correlation between the FXI level and bleeding episodes. Indeed, some patients with deficient levels of FXI don’t show extensive bleeding following surgical procedures. On the other hand, some patients with moderately low levels tend to bleed post-surgery. The typical presenting feature of patients with FXI deficiency is bleeding from tissue rich in fibrinolytic activators following surgery or trauma.
Keywords: Coagulation; Factor XI;Haemophilia C;Factor XI deficiency
Abbrevations: HMWK: High Molecular Weight Kininogen;GpIb: Glycoprotein Ib;FXIIa: Activated FXII;uPA:urokinase Plasminogen Activator. tPA:Plasminogen Tonic
Introduction
The initial treatment of venous thromboembolism (VTE), consisting of patients with pulmonary embolism and proximal deep vein thrombosis, usually combines parenteral low-molecular-weight heparin (LMWH) and warfarin or other oral vitamin K antagonists, and more recently direct oral anticoagulants. If LMWH is utilized it is discontinued once the warfarin reaches a therapeutic level and after a minimum of 5 days of LMWH treatment [1]. The initiation of warfarin therapy is complicated, and although nomograms exist, there is no consensus on the ideal tool. Just as relevant is the need to maintain patients in therapeutic range as a systematic review demonstrated that in patients on vitamin K antagonists, almost half of hemorrhages occurred when INRs were above the therapeutic range, and half of the thromboembolic events took place when the INRs were below it [2]. To reduce these risks associated with either over or under dosing, it is highly desirable to determine the individual maintenance dose as soon as possibleHaemophilia C is characterised by a deficiency of the coagulation factor XI[1]. It is a sporadic bleeding disorder that was first described in 1953 in a Jewish family[1]. The prevalence of this disorder has been reported to be one in 100,000 in the United States. The prevalence is significantly higher in Ashkenazi Jews with 8% of the population are said to have factor XI deficiency[2]. The bleeding tendency in the affected individuals is variable when compared to the well-established and characterised forms of Haemophilia with both males and females are affected.Poor correlation has been reported between the levels of factor XI and bleeding severity[3]. It has been shown that in patients with severe factor XI deficiency no severe bleeding was observed, whereas, some patients with moderate factor XI deficiency bleed following surgical procedures[4]..
In the classical coagulation cascade activation of factor XI is mediated by the contact phase factors of the intrinsic pathway, the contact factor complex includes factor XII, high-molecular-weight kininogen and prekallikrein[5]. However, recent evidence demonstrates that factor XI is activated by thrombin generated by tissue factor activation[1]. Furthermore, it has been suggested that factor XI plays a role in thrombin generation and thrombus formation[1].
Biology and Role of Factor XI
The gene encoding for coagulation FXI is located on chromosome 4 and consists of 15 exons and 14 introns[6]. FXI is composed of two 80-kDa exact polypeptide subunits bound together by a disulphide bond. Within FXI molecule each subunit contains a catalytic domain and four apple domains (A1-A4). The A1 domain encompasses the binding site for prothrombin and high molecular weight kininogen (HMWK)[2]. A3 contains FXI binding site as well as the binding site for platelet glycoprotein Ib(GpIb)[7]. A4 consists of a residue for the disulphide bond that links the FXI subunits and a binding site for FXII[1]. The primary production site of FXI is the liver with reported circulating levels of 5mg/L or 50% - 150% activity[8]. Typically, FXI circulates as a zymogen complexed with HMWK the activated form of FXI is a serine protease[9].
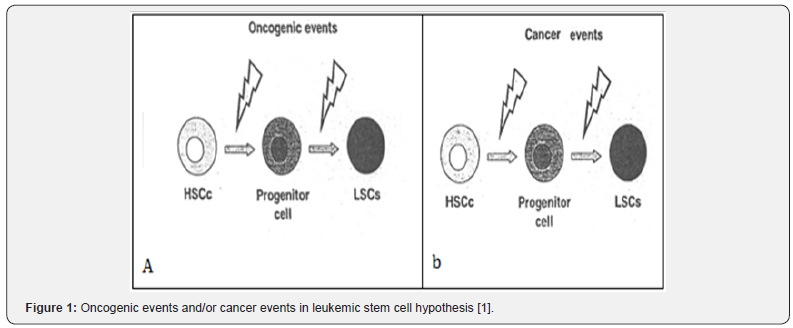
In the classical waterfall model of the coagulation cascade FXI plays an essential role in the intrinsic pathway of the coagulation process[10]. It is well established that contact with negatively charged surfaces in the presence of prekallikrein and HMWK leads to the activation of FXII[11]. Activated FXII (FXIIa) then activates FXI[11]. In the presence of Ca2+FXIaactivates FIX[12]. The combination of FIXa and its cofactor VIII also known as Xase activate FX which leads to thrombin generation and conversion of fibrinogen into fibrin monomer; the coagulation cascade is shown in Figure 1[12].
The coagulation (blue arrows) can be activated during hemostasis through the intrinsic path (contact system, red arrows) or the outer path (grey arrows) that eventually converge towards the common coagulation pathway. Both ways activate factor X and then thrombin, necessary to convert fibrinogen into fibrin and activate factor 13. The fibrin clot is overlapped and stabilized by factor 13. Fibrinolysis is stimulated at the same time as the coagulation system but works more slowly and is important to regulate hemostasis. During the dissolution of fibrin, plasmogenis converted to plasmin which degrades the fibrin network. Coagulation factors are indicated by “F” followed by a Roman numeral, an additional “a” indicates the activated form; HK, molecular weight kininogen; uPA, urokinase plasminogen activator. tPA, plasminogen tonic tonic Adopted from[13].
The revised waterfall model of coagulation suggests that FXI contributes to the amplification of thrombin generation[12]. It has been shown that thrombin activates FXI in the absence of FXII, which leads to further thrombin generation and sustainable thrombus formation. Furthermore, it was demonstrated that FXI is required for thrombin generation in the absence or at low concentrations of tissue factor. Therefore, it is apparent that FXI is essential for thrombin generation and sustainable thrombus formation [12].
Bleeding Tendency
Many FXI deficient patients are asymptomatic and do not experience bleeding episodes[14]. However, physical injury and trauma resulting from surgical procedures or physical activity can trigger bleeding particularly in the nose, tonsils and mouth as these sites contain fibrinolytic system activators. Indeed, a study by Salomon et al. reported bleeding in 49 - 67% of patients with severe FXI deficiency post-surgery involving tissue rich in fibrinolytic activity[15]. A study by Peyvandiaet al. [16] reported post-operative bleeding in 66% of Iranian FXI deficient patients[16]. In contrast, it has been notified that no bleeding in severely FXI deficient patients after trauma[6].
Diagnosis
The majority of FXI deficient patient does not exhibit specific symptoms that promote investigation[11]. The characteristic presentation is prolonged bleeding following injury or surgical procedure that initiates coagulation screening to investigate the cause of bleeding[1]. The most common laboratory finding is a prolonged activated partial thromboplastin time (aPTT)[1]. In diagnosing FXI deficiency, it is essential to record patient’s bleeding history and ethnicity. Furthermore, medical history is essential in determining the cause of the bleeding. Low FXI levels are associated with liver disease because FXI is synthesised by the liver[1]. Also, newborns up to the age of six months usually have low FXI due to the limited synthetic function of the liver. Lupus inhibitors should be considered when investigating a prolonged aPTT; it has been reported that some patients with lupus erythematosus developed anticoagulants to FXI [17]. Molecular characterisation of FXI gene will allow the detection of the genetic mutations causing FXI deficiency, DNA sequencing is becoming increasingly useful in analysing the structure and function of the gene and allows family studies to be carried to identify asymptomatic members.
Therapy and Management
It is well established that individuals with FXI deficiency are at risk of bleeding following surgical procedures from tissue with high fibrinolytic activity[15]. Therefore, it is vital that the appropriate therapy is applied during the haemorrhagic events. Currently, there are some different treatment options available to manage bleeding in FXI patients.
Fresh frozen plasma
Fresh frozen plasma (FFP) is one of most commonly transfused haemostatic agent[18]. FFP was used to treat FXI deficient patient,and it remained principle treatment until the introduction of FXI concentrates[18]. FFP is prepared from donated whole blood units.It contains levels of coagulation factors as well as albumin and immunoglobulins[18]. It has been reported that a unit of FFP comprises around 35-50U/dl of FIX with a half-life of 45 hours. One significant disadvantage of FFP use was the increased risk of disease transmission and a large number of FFP units required to normalise FXI levels. The introduction of viral inactivation methods has improved the safety of FFP transfusion.
FXI concentrates
The development of specific FXI concentrateson replacing FXI deficiency have increased the efficacy of treatment and shortened the infusion times[19]. Currently, there are two manufacturers of FXI concentrations UK Bio Products Laboratory and French LFB Biopharmaceuticals. BPL FXI concentrate contains high levels of antithrombin. Some patients experienced thrombotic episodes following FXI concentrate infusion which lead to the addition of heparin. BPL FXI concentrate had been shown to be effective in achieving appropriate haemostatic response without significant adverse effects. LFB FXI concentrate contains C1 esterase inhibitor in addition to antithrombin and heparin. The efficacy of LFB product has been shown to be similar to BPL FXI concentrate. Both products are treated to inactivate viruses. Thrombotic risks have been demonstrated with both products particularly in elderly patients with the pre-existing cardiovascular disease.
Other therapies
There are other therapies available for those patients who might not benefit from FFP or FXI concentrate. Fibrin glue is supplied in two different vials. One containing calcium and thrombin, while, the other contains fibrinogen, FXIII and aprotinin. Anti-fibrinolytic agents such as tranexamic acid and aminocaproic acid, these agents inhibit the activation of the fibrinolytic system via the inhibition of plasminogen to plasmin conversion[20].
Inhibitor Development
Acquired FXI antibodies are an uncommon complication of FXI replacement therapy[6]. These inhibitors can potentially be problematic in patients who are homozygous for type II mutation[6].FXI inhibitors have been described in patients with severe FXI deficiency. These patients do not usually appear with spontaneous bleeding. However, trauma or surgery may be accompanied by severe bleeding that cannotbe managed by the FXI or Plasma. One study investigated 118 patients not associated with acute FXI deficiency; seven had an inhibitor[21]. All seven patients were treated with plasma substitutes,and all were identical in the yellow allele. Of the 45 patients with other genotypes, identical type III or type II species, and the third type of heterozygous compound that received plasma, none had FXI inhibitors. Thus, only zygotes are similar to zygotes or heterozygous mixtures of an empty allelein that are at risk of developing post-exposure inhibitors to exogenous oxygen[6]. The seven patients who developed deoxyribonucleic acid from 21 zygote species were identical to those of the second type who received plasma, suggesting that 33% of patients with FXI levels of 1 or fewer UDL-1 were likely to develop inhibitors. Immunoglobulin G isolates from patients with inhibitor display weaken FXI activation by thrombin or FXIIa, inhibition of FXI binding to HK or decreased FXIa activation by FX[21].
References
- Gomez K, Maggs PB (2008) Factor Xi Deficiency. Haemophilia 14(6): 1183-1189.
- Asakai Rei, Chung DW, Davie EW, Seligsohn U (1991) Factor Xi Deficiency in Ashkenazi Jews in Israel.” New England Journal of Medicine 325(3): 153-158.
- Kadir RA, Economides DL, Lee CA (1999) Factor Xi Deficiency in Women. American Journal of Hematology 60(1): 48-54.
- Bolton‐Maggs (2000) Factor Xi Deficiency and Its Management. Haemophilia 6(s1): 100-109.
- Srivastava A, Brewer AK, Mauser‐Bunschoten EP, Key NS, Kitchen S, et al. (2013) Guidelines for the Management of Hemophilia. Haemophilia 19(1): e1-e47.
- Seligsohn U (2009) Factor Xi Deficiency in Humans. J Thromb Haemost 7 Suppl 1: 84-87.
- HO DH, Badellino K, Baglia FA, Sun MF, Zhao MM, et al. (2000) The Role of High Molecular Weight Kininogen and Prothrombin as Cofactors in the Binding of Factor Xi A3 Domain to the Platelet Surface. J Biol Chem 275(33): 25139-25145.
- Stavrou E, Schmaier AH (2010) Factor Xii: What Does It Contribute to Our Understanding of the Physiology and Pathophysiology of Hemostasis & Thrombosis. Thromb Res 125(3): 210-215.
- Bruce F, Furie BC (1988) The Molecular Basis of Blood Coagulation. Cell 53(4): 505-518.
- David G, Renné T (2007) Intrinsic Pathway of Coagulation and Arterial Thrombosis. Arteriosclerosis, thrombosis, and vascular biology 27(12): 2507-2513.
- Naudin C, Burillo E, Blankenberg S, Butler L, Renné T (2017) Factor Xii Contact Activation. Semin Thromb Hemost 43(8): 814-826.
- Earl DW, Fujikawa K, Kisiel W (1991) The Coagulation Cascade: Initiation, Maintenance, and Regulation. Biochemistry 30(43): 10363- 10370.
- Loof TG, Deicke C, Medina E (2014) The Role of Coagulation/ Fibrinolysis During Streptococcus Pyogenes Infection. Front Cell Infect Microbiol 4: 128.
- Bolton-Maggs PH, Patterson DA, Wensley RT, Tuddenham EG (1995) Definition of the Bleeding Tendency in Factor Xi-Deficient Kindreds- -a Clinical and Laboratory Study. Thrombosis and haemostasis 73(2): 194-202.
- Salomon O, Steinberg DM, Seligshon U (2006) Variable Bleeding Manifestations Characterize Different Types of Surgery in Patients with Severe Factor Xi Deficiency Enabling Parsimonious Use of Replacement Therapy. Haemophilia 12(5): 490-493.
- Peyvandi F, Lak M, Mannucci PM (2002) Factor Xi Deficiency in Iranians: Its Clinical Manifestations in Comparison with Those of Classic Hemophilia. Haematologica 87(5): 512-514.
- Rodrigo B, Monticielo OA, Chakr RM, Palominos PE, Rohsig LM, et al. (2009) Acquired Factor Xi Inhibitor in Systemic Lupus Erythematosus- Case Report and Literature Review. Seminars in Arthritis and Rheumatism 39(1): 61-65.
- O’Shaughnessy DF, Atterbury C, Bolton Maggs P, Murphy M, Thomas D, et al. (2004) Guidelines for the Use of Fresh‐Frozen Plasma, Cryoprecipitate and Cryosupernatant. Br J Haematol 126(1): 11-28.
- Giancarlo C, Ruggeri R, Rodeghiero F (1996) Clinical Usefulness of Desmopressin for Prevention of Surgical Bleeding in Patients with Symptomatic Heterozygous Factor Xi Deficiency. Brit J Haematol 94(1): 168-170.
- Prentice CR (1980) Basis of Antifibrinolytic Therapy. J Clin Pathol Suppl (R Coll Pathol) 14: 35-40.
- Salomon O, Zivelin A, Livnat T, Dardik R, Loewenthal R, et al. (2003) Prevalence, Causes, and Characterization of Factor Xi Inhibitors in Patients with Inherited Factor Xi Deficiency. Blood 101(12): 4783- 4788.