Accuracy of a Warfarin Maintenance Dose Predictor after Completion of the 10mg Initiation Nomogram
Parvaneh Fallah1*, Melissa A Forgie2 and Philip S Wells2
1 Department of Medicine, McGill University, Canada
2 Department of Medicine, University of Ottawa, Canada
3Department of Medicine, Ottawa Hospital Research Institute, Canada
Submission: May 16, 2018; Published: June 15, 2018
*Corresponding author: Parvaneh Fallah, Department of medicine, McGill University, Canada.
How to cite this article: Parvaneh Fallah, Melissa A Forgie, Philip S Wells. Accuracy of a Warfarin Maintenance Dose Predictor after Completion of the 10mg Initiation Nomogram.Open Acc Blood Res Trans J. 2018; 2(3): 555588. DOI: 10.19080/OABTJ.2018.02.555588
Abstract
Introduction: A 10mg warfarin initiation nomogram safely establishes the INR target of 2.0-3.0 in outpatients treated for venous thromboembolism (VTE). A prediction formula for the warfarin maintenance dose previously proposed has not been validated for more standard maintenance dose definitions.
Objective: To compare the dose determined by the warfarin maintenance dose calculator (maintenance dose [in mg] = 2.5 + 10% of the first week cumulative dose - INR value at Day 8 + 1.5 if INR was below 2.0 at Day 5), to the actual maintenance dose in patients treated for acute VTE.
Methods: We retrospectively analysed a consecutive cohort who used the 10mg warfarin initiation nomogram and were subsequently managed using the Dawn 5.0 software. The maintenance dose was defined as the dose that maintained the INR between 2.0 and 3.0 for three or more consecutive measurements at least 6 weeks apart at any time in months 2 to 4 after treatment initiation and the dose that provided a time in therapeutic range (TTR) of ≥65%. We compared the actual maintenance dose to the dose calculated by the formula.
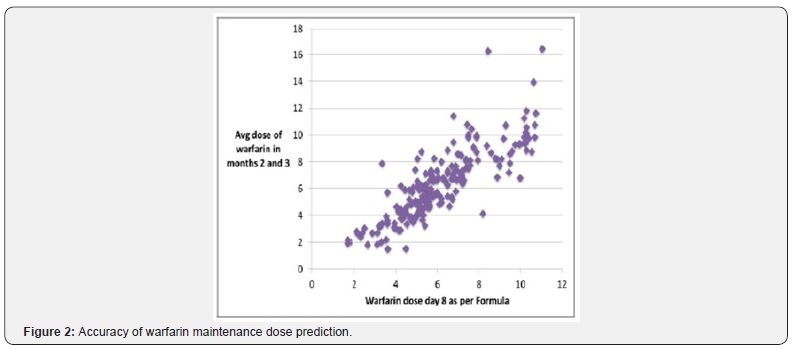
Results: Of 286 patients, 76 did not meet the maintenance dose criteria leaving 210 patients for analysis. The Pearson correlation coefficient was 0.84 (p<0.0001) between the actual and calculated doses of warfarin. Mean and Standard deviation of the difference between actual and predicted were similar.
Conclusion:The prediction formula for Warfarin maintenance dose can be used to predict the maintenance dose in months 2 and 3 of treatment.
Keywords: Venous thromboembolism; Treatment; Warfarin; Clinical prediction rule; Medication therapy management
Abbrevations: VTE: Venous Thromboembolism; TTR: Time in Therapeutic Range; LMWH: Low-Molecular-Weight Heparin; NOACs: Novel oral anticoagulants
Introduction
The initial treatment of venous thromboembolism (VTE), consisting of patients with pulmonary embolism and proximal deep vein thrombosis, usually combines parenteral low-molecular-weight heparin (LMWH) and warfarin or other oral vitamin K antagonists, and more recently direct oral anticoagulants. If LMWH is utilized it is discontinued once the warfarin reaches a therapeutic level and after a minimum of 5 days of LMWH treatment [1]. The initiation of warfarin therapy is complicated, and although nomograms exist, there is no consensus on the ideal tool. Just as relevant is the need to maintain patients in therapeutic range as a systematic review demonstrated that in patients on vitamin K antagonists, almost half of hemorrhages occurred when INRs were above the therapeutic range, and half of the thromboembolic events took place when the INRs were below it [2]. To reduce these risks associated with either over or under dosing, it is highly desirable to determine the individual maintenance dose as soon as possible.
We have previously shown in a randomized trial that a “10mg nomogram” warfarin initiation protocol was able to reach a therapeutic INR value more quickly than an equivalent “5mg nomogram protocol [3]. The “10mg nomogram” was also shown to be effective and safe “outside” of a clinical trial protocol. Eighty six percent of patients reached an INR between 2 and 3 within the first five days in an outpatient thrombosis clinic [4]. Subsequently, we derived a warfarin maintenance dose calculator that accurately predicted the maintenance dose of warfarin to be given after the completion of the “10mg nomogram” warfarin initiation protocol [5]. Maintenance dose was defined as the mean dose in the last 10 days of the first month of treatment but in some cases the maintenance INR is still being determined at the end of the first month of therapy. We sought to determine in a separate group of patients if the warfarin maintenance dose calculator accurately predicted the mean dose to maintain an INR between 2 and 3 in the second and third months of treatment.
Patients and Methods
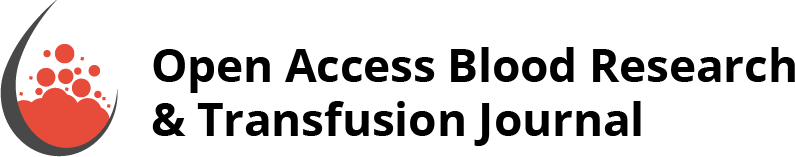
We retrospectively analysed warfarin management of consecutive patients with VTE referred to the Thrombosis Unit at our university affiliated, tertiary care Ottawa Hospital starting on the “10mg warfarin initiation nomogram” (Figure 1) during a 22 month period from July 2010 to May 2012. The start time was chosen to ensure no overlap with prior studies and the end point was chosen since a student was hired at that time for the project. Approval was obtained from our Institutional Research Ethics Board. The study was internally funded. After day 7 of the nomogram patients were managed by a pharmacist with physician support using the dosing software program “Dawn”, version 5.0. All data relevant to the treatment for VTE is kept in the Dawn database and in our hospital electronic medical record. Patients were excluded from the analysis if they failed to complete the initiation nomogram due to an inability to perform INR testing on the required days or failure to obtain INR results on the day of testing. Patients in whom:
i. Previous treatment with warfarin had identified a probable maintenance dose;
ii. The baseline INR greater than 1.3;
iii. The target INR was not 2.0-3.0;
iv. VTE was associated with cancer (Since it was recommended that these patients receive LMWH monotherapy) did not get started on the initiation nomogram and no data was collected on these patients.
We collected warfarin doses and INR results over the course of treatment. The maintenance dose was defined as the dose that maintained the INR between 2.0 and 3.0 for three or more consecutive measurements at least a 6 weeks period at any time in months 2 to 4 after treatment initiation and provided a time in therapeutic range (TTR) of at least 65% as previously defined [6]. We compared this value to the dose predicted by the maintenance dose formula using the Pearson Correlation Coefficient. The formula is: maintenance dose in mg = 2.5 + 10% of the first week cumulative dose ¬ INR value at day 8 + 1.5 if INR was below 2.0 on day 5.
Results and Discussion
Of the 286 patients initiated on and completing the nomogram, 76 did not meet the maintenance dose criteria leaving 210 patients for analysis. Patients had clinic visits one week and three months after diagnosis and annually thereafter, but phone contact occurred after every INR test. No patients were lost to follow-up. These patients had a mean age of 57 ± 15 years and 53% were male. The mean maintenance dose by the formula was 6.11±2.1mg and the calculated mean maintenance dose was 6.26±2.6mg with a Pearson Correlation co-efficient of 0.84 (p<0.0001). Mean and standard deviation of the difference between these two doses were also calculated (0.97mg and mg, respectively) and were not clinically significant. The charts of the 5 patients in whom the difference between predicted and actual maintenance dose was higher than 4mg were reviewed. In two patients, the maintenance doses were 5.4 and 4.1mg higher than the predicted dose. Respectively, we determined these two patients were abusing alcohol and antibiotics at the same time. A third patient was on carbamazepine which could explain the difference but in two patients we could find no explanation. After the exclusion of these five patients, the correlation coefficient between the predicted dose and the actual maintenance dose, was 0.87 (p<0.0001). The mean and standard deviation of the difference between predicted and actual maintenance dose was 0.86±0.75mg.
Our simple formula predicted the maintenance dose of warfarin in patients who initiated and completed our published nomogram that uses 10mg of warfarin on the first two days of treatment. The maintenance dose prediction formula is based on the cumulative dose of warfarin given during the first week of treatment and on the INR values at Day-5 and at the end of the initiation nomogram.
Previous attempts to link the initial dosing to the maintenance dose are limited due to the need for daily INR measurements [7], by the need to use an INR measured two weeks after a fixed 2mg daily dose of warfarin (and this study only predicted 70% of the variability of the maintenance dose) [8], the need for a pharmacogenetics-based approach [9], and that many prediction models only explain 35 to 55% of the inter-individual response to warfarin [10-14]. Our study suggests that simple initiation parameters can reliably predict the maintenance dose. The standardization of warfarin initiation in the nomogram likely contributes to our good results, the parameters used in the rule reflecting patients’ sensitivity to the initial doses given, including factors such as age, weight, and background genetics.
We should highlight that despite having novel oral anticoagulants (NOACs), the low cost, several reversal agents, ease in monitoring anticoagulation, and efficacy better than NOACs in prosthetic heart valve patients make warfarin superior to NOACs in many case scenarios.
It is important to note the limitations of our study. First, there is no one definition of the maintenance dose. However, the definition we have used is reasonable and clinically sensible. Second, our results might not apply to all patients started on warfarin. The reasons for not applying the warfarin nomogram in our patient populations were not recorded and it is unclear whether this could have biased our results. Anecdotally, most cases are related to the logistics of obtaining blood work. Third, we did not use a pharmacogenetic approach. We and others have published algorithms using the polymorphisms known to influence warfarin metabolism [15-19]. However, genetic testing is expensive, none of these studies produced R2 values better than we obtained, and our model is much easier to apply. Fourth, only 73.4% of patients reached a maintenance dose in the 2 to 4 months after warfarin initiation so we could not determine if the formula works for all patients. However, a TTR over 65% in 73% of patients is better than usually achieved according to published data. Our clinic eventually achieves rates of over 82% (unpublished data). So it would still be reasonable to apply the formula in all patients who use the 10mg initiation nomogram. Finally, to follow the nomogram means that INRs must be done on the days prescribed by our initiation nomogram. This could have selected educated and/or more compliant patients [20,21].
In patients started on warfarin and fully managed according to our “10mg nomogram” warfarin initiation protocol, simple parameters related to patients’ treatment course over the 7-days of the nomogram can accurately predict the warfarin maintenance dose in months 2 and three of treatment.
References
- Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, et al. (2012) Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis (9th edn). American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl): e419S-e494S.
- Oake N, Fergusson DA, Forster AJ, van Walraven C (2007) Frequency of adverse events in patients with poor anticoagulation: a meta-analysis. CMAJ 176(11): 1589-1594.
- Kovacs MJ, Rodger M, Anderson DR, Morrow B, Kells G, et al. (2003) Comparison of 10-mg and 5-mg Warfarin Initiation Nomograms Together with Low-Molecular-Weight Heparin for Outpatient Treatment of Acute Venous Thromboembolism. A Randomized, Double-Blind, Controlled Trial. Ann Intern Med 138(9): 714-719.
- Wells PS, Le Gal G, Tierney S, Carrier M (2009) Practical application of the 10-mg warfarin initiation nomogram. Blood Coagul Fibrinolysis 20(6): 403-408.
- Le Gal G, Carrier M, Tierney S, Majeed H, Rodger M, et al. (2010) Prediction of the warfarin maintenance dose after completion of the 10mg initiation nomogram: do we really need genotyping? J Thromb Haemost 8(1): 90-94.
- Rosendaal FR, Cannegieter SC, van der Meer FJ, Briet E (1993) A method to determine the optimal intensity of oral anticoagulant therapy. Thromb Haemost 69(3): 236-239.
- Fennerty A, Dolben J, Thomas P, Backhouse G, Bentley DP, et al. (1984) Flexible induction dose regimen for warfarin and prediction of maintenance dose. Br Med J 288(6426): 1268-1270.
- Oates A, Jackson PR, Austin CA, Channer KS (1998) A new regimen for starting warfarin therapy in out-patients. Br J Clin Pharmacol 46(2): 157-161.
- Schwarz UI, Ritchie MD, Bradford Y, Li C, Dudek SM, et al. (2008) Genetic determinants of response to warfarin during initial anticoagulation. N Engl J Med 358(10): 999-1008.
- Wadelius M, Chen LY, Downes K, Ghori J, Hunt S, et al. (2005) Common VKORC1 and GGCX polymorphisms associated with warfarin dose. Pharmacogenomics J 5(4): 262-270.
- Sconce EA, Khan TI, Wynne HA, Avery P, Monkhouse L, et al. (2005) The impact of CYP2C9 and VKORC1 genetic polymorphism and patient characteristics upon warfarin dose requirements: proposal for a new dosing regimen. Blood 106(7): 2329-2333.
- Gage BF, Eby C, Milligan PE, Banet GA, Duncan JR, et al. (2004) Use of pharmacogenetics and clinical factors to predict the maintenance dose of warfarin. Thromb Haemost 91(1): 87-94.
- Carlquist JF, Horne BD, Muhlestein JB, Lappe DL, Whiting BM, et al. (2006) Genotypes of the cytochrome p450 isoform, CYP2C9, and the vitamin K epoxide reductase complex subunit 1 conjointly determine stable warfarin dose: a prospective study. J Thromb Thrombolysis 22(3): 191-197.
- International Warfarin Pharmacogenetics Consortium, Klein TE, Altman RB, Eriksson N, Gage BF, et al. (2009) Estimation of the Warfarin dose with clinical and pharmacogenetic data. N Engl J Med 360(8): 753-764.
- Wells PS, Majeed H, Kassem S, Langlois N, Gin B, et al. (2010) A Regression model to predict warfarin dose from clinical variables and polymorphisms in CYP2C9, CYP4F2, and VKORC1: Derivation in a sample with predominantly a history of venous thromboembolism. Thromb Res 125(6): e259-e264.
- Moreau C, Pautas E, Gouin-Thibault I, Golmard JL, Mahe I, et al. (2011) Predicting the warfarin maintenance dose in elderly inpatients at treatment initiation: accuracy of dosing algorithms incorporating or not VKORC1/CYP2C9 genotypes. J Thromb Haemost 9(4): 711-718.
- Gong IY, Tirona RG, Schwarz UI, Crown N, Dresser GK, et al. (2011) Prospective evaluation of a pharmacogenetics-guided warfarin loading and maintenance dose regimen for initiation of therapy. Blood 118(11): 3163-3171
- Kangelaris KN, Bent S, Nussbaum RL, Garcia DA, Tice JA (2009) Genetic testing before anticoagulation? A systematic review of pharmacogenetic dosing of warfarin. J Gen Intern Med 24(5): 656-664.
- Gong IY, Schwarz UI, Crown N, Dresser GK, Lazo-Langner A, et al. (2011) Clinical and genetic determinants of warfarin pharmacokinetics and pharmacodynamics during treatment initiation. PLoS One 6(11): e27808.
- Santos PC, Marcatto LR, Duarte NE, Gadi Soares RA, Cassaro Strunz CM, et al. (2015) Development of a pharmacogenetic-based warfarin dosing algorithm and its performance in Brazilian patients: highlighting the importance of population-specific calibration. Pharmacogenomics 16(8): 865-876.
- Hospodar AR, Smith KJ, Zhang Y, Hernandez I (2018) Comparing the Cost Effectiveness of Non-vitamin K Antagonist Oral Anticoagulants with Well-Managed Warfarin for Stroke Prevention in Atrial Fibrillation Patients at High Risk of Bleeding. Am J CardiovascDrugs 10: 1007